To understand why itching occurs between the toes, it is necessary to collect an anamnesis and conduct laboratory and instrumental diagnostics. There are various reasons, including the presence of a hereditary predisposition to various pathologies.
basic information
If a patient has a hereditary predisposition to the formation of itching between the toes, a simple test is performed:
- hold it with a hard object, look at the reaction;
- if the patient has a hereditary predisposition, initially the skin becomes pale, then turns red, and you want to scratch it;
- When a person scratches the skin and then stops, the itching occurs again.
A person feels the recurrence of itching constantly. A vicious circle is formed.
The second reason why the epidermis begins to itch is a violation of the water-electrolyte balance. The condition occurs due to increased dryness and flaking of the epidermis, which leads to itching. The reasons are the following reactions:
- skin diseases (dermatitis, eczema);
- hereditary predisposition;
- use of certain types of medications (antibiotics, antiseptics);
- temperature changes causing increased sweating, especially between the fingers;
- consumption of food to which allergies or individual intolerances occur;
- severe forms of hypersensitivity - atopic dermatitis, urticaria, dermatosis.
That is, a person is influenced by external factors, under the influence of which the immune system cannot resist, so an inflammatory process is formed. Often, such symptoms cannot be treated, are eliminated only temporarily, and then relapse occurs again.
Often the patient is affected by cosmetics with an aggressive composition. For example, deodorants, talc, soaps, shampoos, shower gels, cleaning products. If you completely eliminate their use, the condition will gradually return to normal. Therefore, it is important before purchasing any cosmetics to carefully read the composition and take into account individual intolerances.
In most patients, negative symptoms are caused by a fungal infection that causes mycosis. The condition is accompanied by abundant peeling, wetting of tissues, and severe itching. Therefore, patients should first take this deviation into account when doing laboratory tests and a general examination.
How to diagnose
If the skin between your toes itches, you need to make an appointment with a dermatologist. In addition to a visual examination, he will prescribe diagnostic tests. If an allergy is suspected, a blood test is taken for several types of allergens, as well as a skin test. Mycotic eczema is quite specific in nature and is usually detected at the first examination. However, the doctor makes a scraping to confirm his version. The analysis identifies the specific source of the problem. The same is done in the case of dermatophytosis and psoriasis. Scabies is also characterized by obvious symptoms. If the etiology of the disease is not clear, the scraping is examined under a microscope.
Foot fungus
Fungal growths on the feet occur in almost every second man or woman. The pathology can develop in a chronic form, leading to periodic relapses. Therefore, the following conditions arise:
- rest period
- there are no uncomfortable symptoms at all, the person does not think about the need for therapy, but mycosis still gradually develops, intensifies under the influence of external factors with the development of itching (hot water in the shower, rubbing with a towel, using cosmetics); - period of exacerbation
- a person is bothered by very strong peeling of the epidermis, microcracks and larger wounds form, active and severe itching develops, and when scratched, the wound becomes larger.
To diagnose and receive quality treatment, consultation with a dermatologist is recommended. He will be able to suggest pathology with a simple general examination. But confirmation of the assumption can only be obtained using microbiological analysis.
When fungus develops on the foot, the following clinical symptoms form:
- increased peeling and peeling of the skin;
- increasing pain, burning, itching;
- thickened skin on the soles of the feet;
- deformation of the nail plate, it becomes bumpy, with uneven and flaky edges;
- yellowness of nails;
- formation of cracks on the soles of the feet and the nail plate;
- severe sweating of the feet at any time of the year, regardless of the ambient temperature.
Initially, no symptoms may occur. But then the fungus continues to spread deeper, attacking the epidermis and nail plate, as well as the tissue underneath. At this stage, the signs can no longer be ignored. The disease causes severe discomfort, unpleasant odor from the feet, and a cosmetic defect.
A group of patients is identified who have an increased risk of developing the disease. These include people with an infection while being treated with antibiotics, as well as patients with diabetes.
If therapy is started in a timely manner, the disease is easily controlled and the prognosis is positive. It is important not to waste time, since deep mycosis is more difficult to cure. If it has spread to the deep layers of the epidermis, it will take at least 1 year to restore normal tissue structure.
If a patient has advanced foot fungus, pathogenic microorganisms can gradually spread to other parts of the body. For example, armpits, abdomen, scalp.
Remedies for fungal diseases
The fungus can be treated at home. For this, antifungal ointments are usually used, the most popular of which is nystatin. It has proven itself well in the treatment of mycoses in adults along with systemic drugs (for example, Fluconazole).
There are other external remedies for the treatment of fungus based on ketoconazole, miconazole, clotrimazole, terbinafine. They can have a variety of trade names: Thermikon, Lamisil, Exoderil, Mikoderil, Nizoral, Mikospor, Batrafen and others.
It is advisable that such remedies be prescribed by a doctor, taking into account the type of fungus and all related factors.
But treatment also requires more thorough than usual daily care. You need to wash your feet with warm, but not hot water (it makes the skin itch even more). But it shouldn’t be cold either, because this makes the skin rougher, which aggravates the situation. After washing, it is recommended to powder your feet with talcum powder or a medicinal antifungal composition. Classic remedies also help well - iodine or brilliant green, which are applied directly to areas where the skin is cracking.
Often the infection spreads to the nails. This is clearly visible on the thumb, where the nail plate turns yellow and cracks. In this case, it is advisable to immediately consult a doctor who will select an antifungal agent based on bifonazole and clotrimazole.
Fungal diseases are much less common in children than in adults.
Folk remedies for treating fungus are not suitable as basic ones. They can only be auxiliary, that is, used together with drug therapy. For example, a soap and soda bath. It is prepared like this: 1 tbsp. l. soda and 50 g of grated laundry soap are dissolved in 2 liters of warm water. Place your feet in the water for 10-15 minutes. After this, the skin is blotted and treated with the prescribed ointment. If the fungus appears on the nails, then the layers softened after the bath are removed using nail clippers or disposable nail files.
Methods for treating itching between the toes
If a fungal infection is detected, it is recommended that you initially discard any socks that the patient has been wearing since the onset of the illness. It is also recommended to change your washcloth and slippers. Towels can be thoroughly boiled. It is recommended to remove and disinfect the insoles from shoes, treat them with antifungal drugs or citric acid.
If the disease was detected at an early stage, it will take only 1 month to complete treatment. In addition to medications, additional techniques are used that quickly improve a person’s well-being.
Medicinal ointments
Of the ointments, the following drugs have the greatest effect:
- Clotrimazole;
- Miconazole.
When using ointments, the following treatment measures are recommended, regardless of the drug chosen:
- undergo a full range of therapy according to the instructions for use;
- Apply for at least 2 more weeks to prevent the possibility of re-infection.
If the patient is prescribed a long course of treatment, the ointment is changed every 14 days so that it contains a different active component. This will prevent the fungus from developing resistance.
Burov's solution
Compresses are made using Burov's solution. They are performed according to the following method:
- a cotton swab or disk is soaked in the solution;
- cotton wool is placed between the fingers;
- the foot is lightly bandaged so that the fluid does not spread to the surrounding tissues and concentrates in the lesion;
- after 20 minutes, the cotton wool and bandages are removed.
Among folk remedies, soda has a similar effect. It causes an antiseptic, antifungal effect. Compresses are made using an identical method.
Pills
When a fungal infection penetrates deeply and the pathological process spreads all the way to the nails and soft tissues underneath, it is recommended to use oral tablets. They spread through the systemic bloodstream, penetrating into lesions. Therefore, the effect will be complete. The following types of oral agents are recommended:
- Lamisil;
- Nizoral;
- Griseofulvin.
To enhance immune activity, it is recommended to use immunostimulants. Then the body can cope with the infection faster.
Additional techniques
In order for the treatment to help faster, it is recommended to use the following additional measures:
- daily hygiene with washing your feet at least 2 times a day, for this it is recommended to use laundry soap and thoroughly dry with a towel;
- After each hygiene procedure, antifungal cream must be applied;
- using open shoes in which the feet do not sweat and the skin actively breathes;
- constant change of socks, they must always be clean;
- wiping the insoles of shoes with high-percentage table vinegar, which eliminates odor and has disinfectant properties;
- the use of an ionizing device for disinfecting shoes; it is based on an ultraviolet lamp.
Pharmacies sell special liquids designed to treat shoes to destroy fungal infections. It is called Samarovka.
It is enough to use special ointments and hygiene rules so that the pathology gradually ends. Tablets are taken only in extreme cases, when a serious fungal infection has developed.
The use of folk remedies
Among traditional methods, several techniques are especially popular, which are easy to make and apply to any patient. They are listed in the table.
| Name | Carrying out the procedure |
| Brew 1 mug of strong tea, add a small concentration of table vinegar. Cotton is moistened in the resulting liquid, treating areas of skin with fungus. The procedure is performed 2-3 times a day until symptoms disappear completely. | |
| Squeeze out fresh aloe and mix with celandine solution. Add 1 tablespoon of vinegar. The affected feet are treated with the liquid daily. You can make baths to increase efficiency | |
| Prepare a container and pour a small bottle of glycerin into it. Add vinegar 70%. Mix everything thoroughly and treat the affected skin to eliminate peeling and itching. | |
| Pour a small amount of salt into your socks when you put them on before going to bed. You can first make baths consisting of water, salt and soda. This will enhance the disinfecting effect. All components destroy fungus | |
| Washing your feet with anti-dandruff shampoo. It contains clotrimazole, which has a fungicidal effect. You can first apply a thin layer of shampoo to the skin and nails and leave for 5-10 minutes. With such baths you can sleep at night wearing socks. The antifungal effect will be enhanced |
All traditional methods can be used in turn and over a long course. Allergic history must be taken into account.
Treatment
Particular attention should be paid to careful treatment of lesions.
The patient should take daily warm foot baths with potassium permanganate. In this case, it is necessary to remove the crusts, open the blisters, cut off the fringe along the edges of the erosions, as well as the covers of the festering blisters. After the bath, wet-dry bandages or lotions are applied with an aqueous solution of copper (0.1%) and zinc sulfates (0.4%) or with a 1% aqueous solution of resorcinol. After the weeping stops, dermozolon, mycozolon are used, and then alcohol fungicidal solutions, Castellani paint, and finally, if necessary, fungicidal pastes and ointments.
The effectiveness of treatment depends not so much on the choice of pharmacological drug, but on their correct, consistent use in accordance with the nature of the inflammatory reaction.
Fungicidal treatment is carried out until the fungal test results are negative.
Anti-relapse treatment carried out within a month after the elimination of lesions is extremely important - wiping the skin of the feet with 2% salicylic or 1% thymol alcohol and dusting with 10% boron powder. For the same purpose, it is necessary to thoroughly wipe the inner surface of the shoes with a solution of formaldehyde, wrap them in an airtight fabric for 2 days, then ventilate and dry them, and socks and stockings for 10 minutes. boil.
When athlete's foot is complicated by pyococcal infection, antibiotics are prescribed - methicillin, cephaloridine, oleandomycin, metacycline, erythromycin. The patient must remain in bed.
Preventative techniques
To prevent a fungal infection or its recurrence, it is recommended to use preventative methods.
- Using quality shoes
. It should be made from genuine leather, suede, nubuck and other natural components. It is important to prevent your feet from sweating or developing calluses. - Use of antifungal ointments
. They can be used in a short course for the purpose of prevention. - Disinfecting shoes
. To do this, use a spray previously purchased at the store. It is not recommended to use someone else's shoes and socks. - If the patient visits the bathhouse
, after it it is necessary to thoroughly wipe the feet with a towel. The pores are open, and infection easily spreads into them. - Immunostimulation
. To do this, eat foods high in vitamins, trace elements and minerals. Hardening procedures are carried out. They take multivitamins and go for walks often.
Fungal infections are easy to treat at the initial stage, so you need to pay attention to peeling, itching, layering and changes in the color of the nails. If you use fungicidal drugs in time, recovery will come much faster.
What ointments are used to heal cracks?
There are different ways to heal cracks - the use of creams, gels, lotions, special patches and compresses, various baths. The best option is to alternate between two or three products of different types. If the skin is cracked and hurts, and the cause is external factors or systemic diseases, with the exception of a fungal infection, then you need to buy a pharmaceutical foot cream designed to heal cracks.
There are many such creams - for example, Gehwol, Ambulance, 5D and others.
It is necessary to read the composition of the drug. The best effect is achieved by ointments containing urea. Despite the presence of this ingredient, they smell neutral, and the epidermis heals quite quickly. Creams are applied to all problem areas, including under the little finger.
If the problem is only dry skin, then you can even use regular Vaseline or Shostakovsky ointment (vinyline).
Some people who are not afraid to use unconventional methods treat cracks with creams from a veterinary pharmacy, for example, Zorka. Such products were originally intended to heal cracks in the cow's udder. The concentration of the active substance in them is quite high, hence the quick result - the epidermis heals in a few days. But this remedy is not suitable for everyone. Firstly, allergic reactions cannot be ruled out. Secondly, the smell of this ointment is not the most pleasant, and the texture is too thick and greasy, which can cause discomfort.
For diabetes mellitus, you can use not only the universal ointments listed above for the treatment of cracks, but also series specially designed for this. For example, there is the SixtuMed line. It includes bath oil and balm with natural herbal ingredients.
Such products heal cracks well and prevent the penetration of secondary fungal or bacterial infections. Use them as follows: 1 tsp. oil per 1 liter of warm water. After the bath, your feet should dry, but do not dry them with a towel so as not to injure the skin. Then a balm from the same series is applied to areas with cracks.
What is maceration?
On hot summer days, almost all the feet sweat. One of the purposes of sweat is to cool the body, and therefore it is completely natural in the summer. Then the whole body, and therefore the feet, cool down. After all, there are over 500 sweat glands on the soles of our feet.
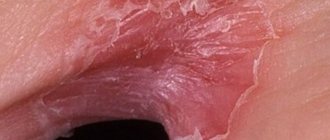
However, too much sweat on the feet can cause maceration, that is, softening of the epidermis. The macerated epidermis loses the features of vital tissue and becomes dead tissue.
Maceration in the interdigital spaces appears as cracked, uneven whitish epidermis. If this occurs on skin with hyperhidrosis, the skin around the maceration becomes intensely red and noticeably moist.
Prevention
In order to avoid cracks in your legs, it is important to follow the rules of hygiene. Under no circumstances should you wear someone else’s shoes or take care items that are not your own, such as a pumice stone or a nail file. After visiting the gym or swimming pool, it is recommended to treat the skin with a solution of salicylic alcohol.
Foot massage using essential oils of coniferous trees (spruce, fir, cedar) is also a good preventive measure. You need to monitor your diet, include vegetable oils, pumpkin seeds, egg yolk, carrots and other foods containing vitamins A and E.
What is the difference between maceration and mycosis?
In contrast to maceration, mycosis is sometimes caused by Trichophyton rubrum or Trichophyton interdigitale. Mycosis on the feet differs from maceration in both appearance and smell. The smell of mycosis is very characteristic and is easily recognized by an orthopedist.
The appearance of mycosis is distinguished by its yellowish-brown color and the presence of additional, not yet cracked, microscopic bubbles that appear next to the already cracked and jagged ones. The vesicles are filled with liquid containing fungal spores. Often they are so small that only the experienced eye of a podiatrist can see them with a magnifying glass. Deposits of necrotic, fungal epidermis can stick together, becoming a threat to the formation of interdigital ulcers, which are very painful and difficult to remove and heal.