Almost every second inhabitant of the earth suffers from diseases of the veins of the lower extremities - just not everyone knows about it, and some simply do not attach due importance to swelling and heaviness in the legs. The blue network of veins that stands out under the skin is also often mistaken for a “normal variant.”
And the person does not even suspect that with his negligent attitude towards his own health he is simply “triggering” varicose veins. “Grows” complications, including acute or chronic thrombosis, thrombophlebitis, blockage of pulmonary vessels by detached blood clots, CVI, which is fraught with disability, and, of course, trophic ulcers
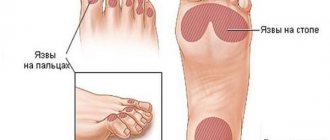
A trophic ulcer looks extremely unpleasant: a non-healing inflamed wound with pus on purple skin. And trophic ulcers ooze bloody-lymphoid discharge mixed with pus - and in general they have a very specific smell of rotting meat. We hope we scared you just enough so that you see the need to be more attentive to your health - and do not tolerate pain in your legs, but immediately make an appointment with a doctor.
How does a trophic ulcer appear: prerequisites and mechanism of development
The main factor in the development of a non-healing ulcer is a serious violation of tissue nutrition. As you understand, with varicose veins , characterized by impaired venous outflow, this is exactly what happens.
Non-functioning venous valves cause blood to flow back (reflux). That is, blood no longer circulates from top to bottom, as in normal conditions. These hemodynamic features are both a consequence and a cause of varicose veins.
Due to the fact that blood stagnates in the tissues of the lower extremities, tissue nutrition deteriorates. The pathology of the venous system progresses, but the ulcer does not develop immediately. First, the skin of the lower leg (most often varicose ulcers occur in the lower third of the lower leg) becomes denser and acquires a characteristic glossy shine. Patients complain of increased swelling in the calf muscle, heaviness and a feeling of fullness.
The affected area begins to itch, small drops of lymphoid fluid appear on the surface of the skin (this occurs due to the development of local lymphostasis).
Then the patient notices increased hyperpigmentation of the skin. After a while, a “harbinger of a future ulcer” develops in the affected area - a whitish area of atrophied tissue. As soon as a person even slightly damages the area of atrophy (for example, touching it with the fabric of trousers), an ulcer appears in this place.
At first, the ulcer looks like a superficial wound with a crust, but as the pathological process progresses, it deepens into the soft tissues of the leg. In addition, its area is expanding.
Usually at this stage a person tries to heal the ulcer on his own using the usual methods (for example, regenerating ointments) - but he will fail. The wound surface becomes infected, begins to fester and ulcerate.
The contents of the separated biological fluid depend on the presence and number of attached bacteria. As a rule, at first the wound oozes bloody-lymphoid discharge, then the ichor becomes more cloudy, and finally acquires a characteristic rotting smell.
In some cases (for example, when the patient’s immunity is weakened), not only a bacterial, but also a fungal infection may occur. This fact further aggravates the person’s condition and somewhat worsens the prognosis.
Causes of development and symptoms
The main reason why furunculosis develops on the legs
, is in most cases Staphylococcus aureus. It is worth noting that staphylococci are microorganisms that are always present on the surface of the skin. However, normally 90% of them are harmless strains that are not capable of causing purulent processes.
Furunculosis develops with a strong change in the ratio of safe and pathogenic strains. This can happen under the influence of various factors. For example, when, if the integrity of the skin is damaged, the leg will not be treated with antiseptic agents.
Predisposing factors also include:
- work or frequent stay in rooms with dusty, polluted air;
- weakened immunity due to vitamin deficiency, stress, vitamin deficiency, diets;
- metabolic disorders and diabetes mellitus;
- hypothermia of the body, drafts;
- chronic diseases of internal organs.
You need to visit the clinic or make a home call from a surgeon
, at the first manifestations of furunculosis. After all, without treatment, there is a high risk of developing various complications, including blood poisoning. Also, without treatment, pus from boils can infect nearby tissues.
The appearance of each boil occurs in stages. After infection of the hair follicle, skin itching occurs in this area, followed by swelling and redness.
Next, a painful dense cone-shaped node of a purplish-red color appears, and after 3-5 days a greenish-yellow rod forms in its center. The patient may also experience chills and high body temperature, increased fatigue and pulsation in the affected area. Subsequently, the boils open, and pus is released from them and the rod is rejected.
Useful information on the topic:
- Diagnosis of surgical diseases
- Treatment of surgical diseases
- How is a consultation with a surgeon carried out?
- Examination by a surgeon
- Surgery - the science of internal medicine
- How is a surgeon's appointment carried out?
- Pediatric surgeon
- Removal of skin tumors
- Paid surgeon
Why you won’t be able to heal a trophic ulcer on your own
The reason that the ulcer does not heal for a long time is the same as the reason for its initial occurrence: insufficient tissue nutrition. In the affected area, the ability to regenerate tissue is sharply reduced - which leads not only to the spread of pathology, but also to life-threatening complications. This is why it is so important to see a doctor on time.
Moreover, treatment of the trophic ulcer itself will be unsuccessful until you eliminate the main cause of its occurrence. And, as medical practice shows, no one has yet been cured of varicose veins and, especially, its complications at home.
Why attempts to self-medicate a trophic ulcer are life-threatening
Firstly, because in this way you will not only delay a timely visit to the doctor - and the wound will not only not shrink, but will also grow deeper into the tissue. And the purulent-necrotic process can spread all the way to bone tissue (in this case, trophism can cause the development of osteomyelitis ).
In addition, the lack of adequate medical care for trophic ulcers is fraught with complications such as:
- Malignant degeneration of a trophic ulcer
- Reduced mobility of the ankle joint (pronounced limitation of capacity - and, as a consequence, disability)
- Phlegmon or sepsis
Often, small trophic ulcers on the surface of the lower leg merge into one wound space. The patient may develop inguinal lymphadenitis, purulent thrombophlebitis or erysipelas of soft tissues.
Reception is strictly by appointment only!!!
Doctor Plus LLC License No. LO-77-01-004801
Registration at the clinic by phone
Make an appointment at the clinic
- +7 (495) 125-49-50
- Addresses of clinics in Moscow
- Daily
- call me back
Abscess of the leg
occurs when a purulent bacterium enters the soft tissue. This could be Staphylococcus aureus, Streptococcus and other bacteria. Treatment is possible at home.
But unqualified treatment can provoke a chronic form of the disease and lead to undesirable consequences. In this regard, the best option when an abscess appears is to visit our clinic, where the patient can be treated by an experienced doctor.
You can make an appointment with a surgeon from our consultants by calling +7 (495) 125-49-50
Prices for services Addresses of clinics Consultation with a gastroenterologist Hirudotherapist Ultrasound of the abdominal cavity Call a surgeon to your home
Diagnosis of trophic ulcers and pathologies that became the root cause of its development
- The following features indicate that the patient’s leg is not just an infected wound, but a trophic ulcer:
- The typical localization of a trophic ulcer is the lower third of the leg
- The skin around the wound surface is usually thickened
- The skin in the immediate vicinity of the wound has pronounced pigmentation
- With intense palpation, characteristic “pits” form in the soft tissues
- The wound surface itself and nearby tissues show signs of inflammation (redness, swelling)
- The wound oozes, the ejected contents have an admixture of pus and a specific smell of rotting
If a person has pronounced manifestations of vascular pathologies (for example, dilated tortuous veins resembling bunches of grapes), then it makes sense to talk not just about the vascular cause of trophic development, but about an advanced stage of varicose veins.
Often patients with trophic ulcers are admitted to the hospital after suffering thrombophlebitis.
By the way, sometimes a person does not even realize that he has suffered thrombosis - because the pathology proceeded without pronounced signs. However, with increased blood clotting, episodes of surgical interventions, or prolonged immobility of the patient, it makes sense to talk about a high probability of thrombosis.
To assess the condition of the venous system of the lower extremities, doctors at the ANTIREFLUX Center use high-precision innovative technologies: the “gold standard” for diagnosing venous diseases - ultrasound angioscanning, as well as spiral computed tomography, which provides images in three-dimensional implementation. This research method allows us to identify even hidden vascular pathologies.
Furunculosis on the legs: diagnosis and treatment features
At the initial appointment, the doctor examines the lesion on the legs, and to determine the pathogen, a bacteriological culture of the discharge from the boils is performed. In addition, for furunculosis, additional tests may also be prescribed, for example, clinical blood and urine tests, a blood sugar test.
Treatment of furunculosis localized on the legs can be therapeutic and consist of local drugs and antibiotics. Immunity boosters, vitamins and physical therapy improve the effectiveness of treatment. However, in many cases the surgeon
may prescribe surgical treatment.
Causes and diagnosis
As mentioned above, leg abscess
begins when bacteria enter a favorable environment. The following factors can provoke such an environment:
- Damage to the skin on the leg;
- Hypothermia;
- Weakened immunity due to previous diseases;
- Failure to comply with hygiene rules.
People with diabetes and alcohol abuse are also at risk. Feignment of the leg can form in the soft tissues or in the bone tissue. When diagnosing an inflammatory process, it is very important to correctly determine the location of the inflammation.
In our clinic this can be done using high-precision medical equipment. Among the elements of instrumental diagnostics, X-ray and computed tomography are used. The sooner a patient contacts our clinic for help, the more effective the treatment will be.
A signal to visit a doctor may be the detection of the following symptoms of inflammation:
- Redness and swelling of the skin.
- There is a thickening of the inflamed area.
- Leg mobility decreases due to pain.
- The skin at the site of inflammation has a higher temperature compared to other areas of the skin.
In addition to instrumental diagnostic methods, our clinic widely uses laboratory tests. A general and biochemical analysis of the patient’s blood helps not only to detect the inflammatory process in the human body, but to determine its degree and nature of its course.
What is a leg abscess
An abscess is an inflammation that can occur in the human body. The peculiarity of this type of inflammation is that purulent bacteria located in the human body, when placed in favorable conditions, begin to actively multiply. This forms abundant purulent masses, around which a capsule is formed. It has a protective function, preventing pus from entering healthy areas.
After some time, the head of the capsule matures and breaks through. This process must be controlled by a surgeon. At best, the abscess breaks out, but the capsule may empty into the tissue, which will cause unwanted complications.