Quite often, antibiotics become the cause of drug allergies. The leading position is occupied by the penicillin group, because these antibiotics are the first means that humanity came up with to fight microbes. Most often, an allergy to antibiotics does not occur immediately, but only with repeated use. In addition, it is known that other reactions are possible to antibiotics - toxic ones, which can be very reminiscent of an allergy.
Causes of allergies to antibiotics
Scientists have not yet found any specific cause of allergies to antibacterial drugs. It is known that the risk of allergies increases in people suffering from food allergies and hay fever. Concomitant diseases (viral infection, autoimmune diseases, etc.) and the presence of drug allergies in blood relatives are important.
Antibiotic therapy support
Particularly important for patients with allergies.
During treatment, it is recommended to take probiotics as part of complex therapy orally and, if indicated, locally from the first day of treatment and during the recovery period after treatment. It is recommended to increase the daily dose of probiotics by 2 times relative to age. The minimum interval between taking the probiotic and the drug is 2-3 hours.
The order, duration and frequency of administration, the amount of daily and single doses of a probiotic for a particular patient are determined by the attending physician and may differ from the recommended regimen. For example, according to the decision of the attending physician, it is possible to take only one or two of the three drugs of the complex.
Probiotics when taking antibiotics
Probiotics Bifidum BAG and Trilact are indicated for use from the first to the last day of taking the antibiotic in double dosage with a spread of time for taking the probiotic and antibiotic at 2-3 hours. After a course of antibiotics to restore your own microflora, a probiotic course is 3-4 weeks in age-specific dosages.
Broad-spectrum antibiotics eliminate both the causative agent of infection (staphylococcus, streptococcus, Klebsiella, Proteus and many other bacteria) and beneficial microflora. Bifidobacteria and lactobacilli are among the main ones in the functioning of the body's immune system. Without them, the immune system does not work.
Short course of antibacterial therapy (5 - 10 days)
Taking increased doses of probiotics orally and locally as indicated from the 1st day of treatment.
The interval between taking an antimicrobial drug and a probiotic is 3 hours.
According to the decision of the attending physician, Ecoflor from 2 to 3 packs can be added to Bifidum BAG and/or Trilact. per day for the entire period of therapy to prevent toxic damage to the liver and other organs.
Recovery period after treatment (rehabilitation) - recommended after completion of any treatment that requires medication. Necessary for consolidating the results of treatment and obtaining a longer and more lasting result, achieving long-term remission, reducing the number of relapses of the disease and improving the patient’s quality of life
After completing the treatment course, it is recommended to conduct a restorative course of taking probiotics - 40 days (see)
Recommended regimen for use of Bifidum BAG/ Trilact/ Ecoflor for the correction of intestinal flora after antibiotic therapy, children over 12 years of age and adults.
Course duration 40 days
| Stages of treatment | Duration | Time and dosage of medications |
| Preliminary stage | 1-15 day | In the morning – Ecoflor 1 pack During the day – Ecoflor 1 pack In the evening – Bifidum BAG 6 ml |
| 1st stage | 16-40 day | In the morning – Trilact 6 ml In the evening – Bifidum BAG 6 ml |
View all articles in the “Microbiocenosis” section
Allergy to antibiotics: symptoms
As a rule, an allergy to antibiotics in a child or adult manifests itself with local and general symptoms. Let's get to know them better...
Common symptoms of antibiotic allergies
- Anaphylaxis. This formidable complication develops immediately after taking or administering an antibiotic, and is accompanied by a decrease in blood pressure, suffocation, and skin rashes;
- Increase in body temperature up to 40°C;
- Steven-Johnson syndrome and Lyell's syndrome are extremely rare. These severe conditions are accompanied by skin inflammation, fever and general intoxication.
Local symptoms of allergy to AB
- Skin rashes resembling nettle burns. Doctors call such local manifestations “urticaria.” The rash is accompanied by itching and increased skin temperature.
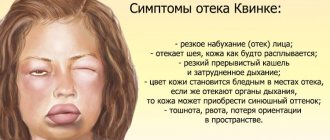
- Quincke's edema is swelling of the face, neck, scrotum, and larynx. There are complaints of shortness of breath, suffocation, and a feeling of fullness.
- Increased sensitivity to sunlight - photosensitivity. Redness, blistering, and itching occur on exposed areas of the body.
Allergy to antibiotics: treatment
First of all, the antibiotic that caused the allergy is canceled and replaced with another antibacterial drug. The doctor prescribes antihistamines to reduce allergy symptoms.
- Allergy gel Enterosgel is considered to be a fairly effective treatment for treatment; it quickly, effectively and safely removes toxins and allergens from the body;
- For anaphylaxis, adrenaline is prescribed;
- In severe conditions, hormonal drugs are used.
Interesting Facts
Scientists have found that antibiotics in tablets are less likely to cause allergies, unlike drugs injected into a vein or into a muscle.
It is undesirable to use ointments with cephalosporins and penicillins, since there is a possible risk of sensitization of the body and allergies when these antibiotics are prescribed in injections or tablets.
Some antibiotics have a similar structure and can cause cross-allergy. For example, the use of a cephalosporin may cause an allergy with the subsequent use of penicillin and vice versa.
Preventing allergies to antibiotics
The main principle of preventing an allergy to an antibiotic is clear and simple - do not self-medicate and limit the uncontrolled use of antibiotics to the maximum!
You should also not forget about a hereditary predisposition to allergic reactions and promptly inform your doctor about this fact.
If after taking the medicine you have signs of an allergy, take Enterosgel and consult your doctor.
Study: connection between antibiotics and allergies in children
Almost everything in the world has two sides, and medications, alas, are no exception. All of them, even the most seemingly harmless and “natural” ones, exhibit side effects. The words of Paracelsus, spoken by him four hundred years before Fleming’s accidental discovery of penicillin, “All poison, all medicine,” reflect the real situation in pharmacology of the 21st century. This does not mean that we need to give up medications, but it is important to be aware of their side effects. And just recently, data has appeared indicating that one of the most popular groups of drugs that allow us to survive in the world of bacteria - antibiotics - has one significant drawback.
Scientists say
Information that has already alarmed both the scientific world and practitioners was published at the end of December 2022 in the major scientific journal Jama Pediatrics (1). The researchers conducted a large-scale analytical work: they studied 798,426 medical records of children born in 2001–2013. The subject of their attention was the prescription of antibacterial drugs of five classes, which are most often used in pediatrics - penicillins, penicillins in combination with β-lactamase inhibitors (clavulanic acid), cephalosporins, sulfonamides and macrolides. The researchers recorded all prescriptions of these classes of antimicrobial agents to infants from birth to six months of age, and then carefully reviewed the medical records of these children.
The results of the analysis showed that 16.7% of infants received antibacterial drugs: penicillins were most often prescribed, then in descending order: macrolides, cephalosporins, protected penicillins, and least often - in 3.8% of cases - sulfonamides.
Moreover, antibacterial drugs of all these groups were associated with allergic diseases in later life.
These include food allergies, asthma, atopic dermatitis, allergic rhinitis, allergic conjunctivitis, and contact dermatitis. In addition, an increase in the likelihood of an extremely dangerous allergic reaction, which is fatal in 10–20% of cases, has been recorded - anaphylaxis, or anaphylactic shock. The risk of developing allergies is highest after taking penicillins and least after taking sulfonamides. It has not yet been possible to accurately establish the cause-and-effect relationship between antibiotic therapy and allergic diseases. But scientists were able to describe the possible mechanism of the adverse reaction.
Alleged reasons
One of the factors that likely contributes to the increased risk of allergic diseases several years after the use of antibiotics and sulfonamides may be their negative impact on the microflora. It is known that antibacterial drugs do not work selectively, showing an effect against both pathogenic bacteria and beneficial microorganisms necessary for our immune system to protect against allergic or autoimmune diseases.
We are talking about both the “famous” intestinal microflora and the microbiome as a whole - after all, bacteria live not only in the digestive tract, but also on the skin, mucous membranes, biliary tract, genitourinary organs, lungs and other organs and systems. The death of beneficial bacteria during antibiotic therapy may start a pathological chain, disrupting important natural defense mechanisms against allergies.
It should be emphasized that this is a possible reason, not an obvious one. To more accurately determine why exactly the risk of allergies increases after the use of antibacterial agents, more than one research work will be needed. But regardless of the results of further research, the fact of another adverse reaction of this class of drugs is already obvious. The scale of the analysis is so large that its results cannot be doubted: unfortunately, infants under six months of age who received antimicrobial drugs belonging to one of the five pharmacological groups described are at increased risk for developing allergic diseases in later childhood and adolescence .
Possible consequences
Of course, the connection between antibiotic therapy and allergies is bad news. However, it should in no way be taken as a ban on the use of antibacterial agents for infants. Drugs in this group still remain the only effective protection against pathogenic microorganisms. They should be prescribed if there are indications for it.
The risk of not taking antibiotics and synthetic antimicrobial drugs can be much more significant for the health and even life of a child than the hypothetical probability of developing allergies in the future.
Information about the results of the study is important primarily for pediatricians prescribing antibacterial drugs. Physicians deciding whether to treat infants with antibiotics should weigh the risk/benefit ratio particularly carefully.
What remains for parents?
Trust the doctor and, if indicated, be sure to give the child the prescribed medications. If absolutely necessary, check the conclusion with the help of other doctors. But the main thing is to never self-medicate your child with antibiotics! Do not “prescribe” them to your baby yourself based on the results of reading various online articles and do not try to purchase them without a prescription. Take care of your health and the health of your family! Sources:
- Zven SE et al. Association Between Use of Multiple Classes of Antibiotics in Infancy and Allergic Disease in Childhood // JAMA pediatrics. — 2020; 174(2):199–200.
Marina Pozdeeva, pharmacist, medical journalist Photo depositphotos.com The author’s opinion may not coincide with the opinion of the editors
What else is important to remember?
In the development of allergies, the key factor is the contact of the allergen (any substance in the air, food, clothing, etc.) with the body. Accordingly, minimizing or eliminating such contact prevents the development of the reaction, which explains the effectiveness of Enterosgel.
It is known that the intestines play a critical role in the functioning of the immune system. Enterosgel removes allergens from the gastrointestinal tract. In addition, Enterosgel removes bacterial endotoxin, promotes the regeneration of damaged mucosa and normalizes intestinal microflora. The latter is extremely important because antibiotics kill bacteria indiscriminately, and this contributes to the release of large amounts of bacterial toxins into the intestines.
Thus, the functioning of the intestines and immune system is restored, and allergic manifestations are reduced. At the first signs of a possible allergy, you can take Enterosgel in a standard dose. Then use the drug according to the instructions for 1-2 weeks.
The harm of antibiotics to the intestines
The term intestinal dysbiosis refers to all diseases in the small intestine that occur due to microflora disturbances. They are accompanied by loss of intestinal cells and an increase in their permeability. The influence of antibiotics on this process is undeniable. Even one dose of an antibiotic can significantly affect the microflora.
In medicine, relatively recently, they began to realize the negative consequences that antibiotics cause, the side effects of which must be minimized immediately. Any antibiotics can change the intestinal flora, but some of them - penicillins, cephalosporins, fluoroquinolones, clindamycin - are a direct cause of antibiotic-associated and pseudomembranous colitis. The first develops under the influence of antibiotics, the second is caused by clostridia bacteria, which rapidly multiply against the background of damaged microflora.
Think about your immune system in time. If antibiotics are essential for you, talk to your doctor about which medications you should take at the same time as antibiotics to restore your levels of beneficial bacteria. This will help minimize the effects of taking antibiotics, and intestinal treatment will not be so long and expensive.
If you are prescribed antibiotic treatment, you need to take preventive measures and undergo a course of probiotic therapy to restore beneficial bacteria that were destroyed during therapy. The most optimal preparations after antibiotics are liquid concentrates of bifidobacteria and lactobacilli Bifidum Bagh and Trilact. In addition to the fact that beneficial bacteria cover the intestines with a continuous protective biofilm, leaving no chance for fungi, they also normalize metabolism and digestion, which reduces bloating, the body quickly cleanses itself of toxins, and improves immunity. To achieve this effect, the number of probiotic bacteria must reach a certain titer. It is generally accepted that a probiotic should contain 10 million colony forming units per gram. For comparison: the liquid probiotic Bifidum Bag contains 10 to 12 power (1000 billion) bacteria, that is, this figure is higher than other probiotic preparations that are prescribed after antibiotics.
At the same time, intestinal dysbiosis is corrected with a diet high in soluble and insoluble fiber and low in saturated fat and animal protein. These reduce the concentration of bacteroids and increase the concentration of bacteria that produce lactic acid: bifidobacteria, lactobacilli and lactic acid streptococci.
Adding fiber to the diet can have different effects on the treatment of dysbiosis. Insoluble fibers reduce the concentration of bacteria and their activity. Soluble fiber, on the other hand, increases bacterial concentrations and enzymatic activity while increasing levels of beneficial short-chain fatty acids. In most cases, you can successfully eliminate mild symptoms of irritable bowel syndrome by learning to manage stress and making diet and lifestyle changes.