According to statistics, foot skin fungus, or mycosis, affects every fifth inhabitant of our planet. This disease, although not fatal, is accompanied by very unpleasant symptoms: severe itching, peeling of the skin between the fingers, redness and an unpleasant odor. coming from the legs. It is important to start treatment in a timely manner in order to get rid of the disease at the initial stage of development. If this is not done, the disease will go into a chronic stage, and then it will be very difficult to eliminate the symptoms of skin fungus and toes.
- Baths
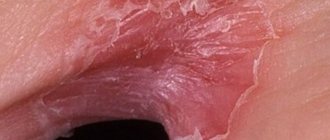
Fungus is itchy and soggy skin between the fingers
Fungal spores penetrate into those areas of the foot where the skin is tender. Under the influence of the parasite, the epidermis becomes wet and destroyed. The fungus destroys proteins in the skin, feeds on them, multiplies and releases toxic products of its metabolism.
Important! Men are more susceptible to fungal foot infections due to constant wearing of closed shoes and increased sweating of the feet.
Among women, dermatomycosis of the legs is more common in athletes. Pedicures pose a certain risk, especially in the absence of sterilization of instruments.
WHAT IS A FUNGUS?
Fungal diseases of the skin and nails belong to a group of human infectious diseases that are caused by pathogenic fungi. Fungal infections (mycoses) are different. There are very severe forms of infections with high mortality. However, not many people suffer from them. Nail mycosis is not one of them and it is impossible to die directly from it. But fungal infections of the skin and nails are one of the most common fungal diseases. This is a contagious disease transmitted from person to person.
WHAT DOES NAIL FUNGUS LOOK LIKE?
Many people do not pay attention to changes in the nail plates, very often considering these changes to be a consequence of injury or age-related characteristics. Fungal nail diseases have many different manifestations. But as a rule, changes in nails due to a fungal disease have three main manifestations: changes in the color of the nail plate, its thickening, crumbling or destruction.
FUNGUS OR NOT FUNGUS?
So, you may notice some changes in the skin or nail plates. It remains to decide whether it is a fungus or not. There are a lot of known non-fungal diseases of the skin and nails - several hundred names. However, according to statistics, every second nail disease is fungal. That is, if your nails are changed, the chance of having nail fungus is 50%, regardless of any manifestations and factors. What about foot skin diseases? They obey the same laws of probability. That is, most lesions on the skin of the feet are fungal. Remember, untreated foot fungus will sooner or later turn into nail fungus. But you can’t get rid of nail fungus so easily. Don't fool yourself. If you suspect you have a skin or nail disease, contact a mycologist! Despite the fact that most nail changes turn out to be a fungus, the other nature of these changes should also be taken into account. Here we need to highlight, first of all, chronic nail injury. Changes in nails can occur with some common skin diseases, internal infectious diseases, damage to the nervous, endocrine, cardiovascular systems, various types of intoxication, as well as dystrophy. Finally, nail changes can be congenital. These changes in the nails look similar to a fungal infection, but they are not. Treatment with antifungal drugs for non-fungal nail diseases, of course, will not be successful. This is another reason to consult a mycologist rather than try to treat yourself if there are any changes in the nails.
IS IT POSSIBLE TO RECOGNIZE A NAIL FUNGUS YOURSELF?
No you can not! And not a single professional doctor, no matter how much experience he has, will undertake the treatment of a fungal disease without confirming the diagnosis in the laboratory, even with the most typical signs of fungus on the legs. Laboratory confirmation is a prerequisite for any fungal disease. To put it simply, if a laboratory finds a fungus in a skin flake or a piece of nail taken for analysis, then this is a fungal disease.
DILEMMA: TO TREAT OR NOT TO TREAT A FUNGUS?
Some people have doubts whether it is worth taking treatment for nail fungus at all. Many people argue as follows: does treating a fungal disease require money? Requires. How long will it take to be treated? Perhaps for a long time. Then, really, why bother being treated for mycosis at all? Does it really matter that the nails have been changed, because they can finally be hidden... Is this game worth the candle? Why do you need treatment for mycosis? Let's try to understand this issue... Once it starts, a fungal infection will not go away until the fungus is destroyed. Fungi are very tenacious and can survive for months in fallen skin scales. What then can you expect from a fungus lurking in your nails? First, fungal cells enter the skin, attach, multiply and spread on it and then, under favorable conditions, penetrate into the nail. Over time, the fungus affects all parts of the nail and spreads to other nails or skin. Nail fungus is a hotbed and source of infection for infecting other parts of the body. Even if all foci of fungus on the skin of the feet or torso are cured, re-infection will occur from the remaining source of infection in the nails. Fungal nail diseases reduce the quality of life. Research conducted by the National Academy of Mycology has shown that the presence of nail fungus or athlete's foot significantly reduces the quality of life - a set of indicators that characterize a person's emotional, mental and social well-being. It turned out that the quality of life with fungal nail disease decreases to an average of 50–55% of the full value characteristic of a healthy person. At the same time, patients noted not only physical inconvenience associated with thickening or destruction of nails, but also experienced various experiences, fears, and negative emotions. It was found that nail fungus greatly limits a person’s activity, interfering with his rest, exercise, and communication with other people. Moreover, feelings of inconvenience and shame about the condition of one’s nails sometimes prevented timely consultation with a doctor. The longer the disease lasted, the more severe the nail fungus became, and the worse the quality of life became. In addition to reducing the quality of life, the fungus leads to certain health problems. The first and main health problem caused by the presence of mycosis of the nails is the fungus itself - a chronic infectious disease that steadily destroys the nails and threatens to spread to the people around them, especially members of the patient’s family. By the way, the presence of a relative with a fungus is noted by at least 1/3 of patients with nail damage. According to medical statistics and epidemiological studies, in Russia the presence of fungal nail disease can be expected in almost every fifth adult. Moreover, the incidence rate has increased 2.5 times over the past 10 years. A further increase in incidence is expected. Moreover, the likelihood of having fungus increases with age: approximately 2 times for every 10 years of life. Untreated mycosis of the nails and mycosis of the feet are considered as entry points for other infectious diseases - for example, bacterial - erysipelas. Fungal infection of the nails significantly complicates the course of diabetes mellitus and can lead to serious complications. Allergization of the human body with a fungal infection is possible - the formation of hypersensitivity to the fungus as an allergen, that is, fungal allergy. The development or worsening of diseases such as bronchial asthma, allergic dermatitis, various skin rashes and reactions is possible. In very rare cases, usually against the background of immunodeficiency, untreated nail fungus led to the development of deep mycosis - germination or penetration of the fungus with blood into the internal organs, which caused death. Fortunately, most modern patients with nail fungus do not experience such outcomes. But even if you completely exclude their possibility, you cannot leave fungal nail disease without treatment. How to treat scabies, pediculosis and other infectious diseases. If you suspect nail fungus, we advise you to consult a doctor as soon as possible. While we were thinking this way, the fungus in someone's nail may have advanced a fraction of a millimeter. This is his job, a small business, so to speak. The fungus does this constantly, day after day. Days turn into weeks, weeks into months, months into years. Over the years, the disease becomes more severe if the fungus is left untreated. One of the latest studies showed that every 5 years the severity of onychomycosis increases by several points on a special scale. This means that new nails are affected by the fungus, and in each of them the affected area and the degree of thickening increase. This means that the negative impact of mycosis on health and quality of life will be stronger. This is a proven fact. But that is not all. The more severe the fungal nail infection, the more difficult it is to treat. While antifungal polish or nail solution may help in the early stages of infection, after a few years antifungal tablets are no longer necessary. The longer the disease lasts, the longer you will have to take them (and buy more). And after ten to twenty years, as a rule, only removal of the nail plate plus these remedies will help. Contact your doctor as soon as possible. With each year of delay that you give to the fungus, you lengthen the required period of treatment and observation, add large doses of medications, and make nail treatment necessary. Don’t make a very big mistake - don’t take systemic medications on your own! If fungal nail diseases did not cause the changes mentioned above, then, in fact, treating fungus would only be a matter of attitude to one’s appearance. Then we would put healthy nails on the same list as white teeth, clear skin and no bad odor. And the question of the cost of treating mycosis would sound like this: Are you ready to give money to get back your uneaten, non-thickened and non-yellow nails? However, this is not the only question. Are you willing to pay to protect your family from athlete's foot? Do you want to regain your previous quality of life? Are you able to stop the spread of infection today? We hope that we have convinced you that fungus is a disease and should be treated. BECAUSE OTHERWISE, YOU WILL GIVE YOURSELF TO THE FUNGUS “TO BE EATEN” AND IT WILL NEGATIVELY AFFECT YOUR LIFE IF YOU DO NOT GET RID OF IT! BECAUSE OTHERWISE YOU WILL INFECT YOUR FAMILY AND FRIENDS, AND THEN REST OF THE PEOPLE!
Forms of fungus: chronic and acute
When a strong immune system suppresses the infection, then the disease occurs in an erased form. A person occasionally feels itching of the skin between the fingers and observes peeling of the epidermis there. Typically, sweating and water procedures lead to increased discomfort.
What fungus looks like on the feet in various forms of chronic disease:
- Erased . Peeling is slight, manifests itself in the space between the last and penultimate fingers of the lower extremities.
- squamous . The affected area is covered with small scales and itches after getting wet and sweating.
- Hyperkeratotic. Peeling, a small number of blisters, plaques resembling calluses, discomfort worsens at night.
- Opreloid . Reddened, swollen, weeping skin between the fingers, the epidermis quickly softens, becomes covered with erosions, cracks, which causes pain.
- Dyshidrotic . Numerous blisters, weeping areas, erosions, under which pink-red skin is visible.
Attention! The inflammatory process and wetting occur more intensely in young and middle age. In older people, the skin is prone to hyperkeratosis and peeling.
The acute form of the disease is accompanied by elevated body temperature, painful erosions, cracks, and crusts between the fingers. Once the skin is contaminated, a bacterial infection occurs and an unpleasant odor is felt.
ethnoscience
Folk wisdom has given rise to a lot of health recipes, each of them, in the author’s opinion, deserves separate consideration, but it is worth focusing on several of the best options that explain how to treat foot fungus.
Salt
The simplest and most proven
method, the salt absorbed into the skin during the bath dries it out, eradicating the moist habitat necessary for the fungus to develop.
Take a bath every day, this will promote recovery, it is better to take sea salt, it softens the nails and skin and helps remove affected areas.
Iodine
Being an excellent antiseptic,
also suitable against fungus:
- you can simply smear the areas infected with the parasite;
- you can make baths.
Due to the aggressiveness of iodine as a reagent, its use has a number of restrictions:
- it causes an allergic reaction;
- in the later stages of development of the parasite, it is also not applicable, because the skin has burst, and iodine can harm the subcutaneous tissues;
- the maximum concentration of iodine in a solution used against fungus is 5%;
- the use of iodine leaves traces because when treating a fungus on the big toe, wearing open-toed shoes will not work.
Soda
One of the most effective
methods of treating fungus invented by traditional healers, the treatment procedure has many variations, requires special attention, and improper treatment leads to even greater problems with the skin.
Despite its disadvantages, soda:
- copes well with fungus between the fingers;
- can lead to long-term remission within a month of a properly maintained course of treatment.
In addition to the above methods, people popularly use:
- Kombucha for fungus;
- onion juice;
- decoctions of oak bark;
- glycerol;
- bromine and much more.
Variety of fungus species
Skin mycoses on the legs are caused by microorganisms belonging to the group of dermatomycetes: Trichophyton, Microsporum, Epidermophyton. They account for 9 out of 10 cases of skin mycoses and onychomycosis (nail fungus). The distribution of microorganisms of the genus Candida is more modest - 9% of all cases.
Treatment of fungus in the folds between the toes is difficult not only because of the variety of types of microorganisms. Pathogens may become resistant to the agents used. Together with constant cases of infection and self-infection, this makes it very difficult to get rid of the infection. Microbial toxins suppress local immunity, the skin is constantly inflamed, because interdigital fungus on the feet weakens its protective properties.
Herbal medicine in the fight against fungus
The fungus can be treated gently and painlessly with herbal remedies. Plants located in the yard or on the nearest roadside, in the form of infusions and decoctions, exhibit an antiseptic, wound-healing and drying effect.
Antifungal plant extracts from herbs and flowers are prepared for external use:
- Celandine.
- Calendula.
- Burdock.
- Mint.
- Nettle.
- St. John's wort.
- Sage.
- Chamomile.
60 milligrams of celandine herb is calculated for 1 liter of water. After boiling, the extract is allowed to steep for 5 minutes. The strained decoction is used for compresses and foot baths, taken for half an hour daily for 21 days. Add 30 ml of vinegar to the cake of boiled stems to use as a compress.
Field and meadow herbs (mint, chamomile and nettle, St. John's wort, sage) are dried, crushed, mixed, and placed in socks for the whole day. The procedure lasts 3 weeks.
Herbal remedies for external treatment
Burdock juice has a detrimental effect on foot fungus. To obtain it, young leaves are collected, beaten with a hammer, and wrapped around the feet at night, securing them with a piece of gauze, a bandage, or a sock. Do the same with rowan leaves, changing them every half day.
To wash between your fingers with calendula infusion, you need to take 250 grams of dried flowers and one glass of boiled water. Infusion time is 30-35 minutes. The effect can be achieved in 30-40 days.
Herbal decoction for internal use
Aqueous extracts of well-known medicinal plants help to destroy the fungus that lives between the toes:
- Common burdock.
- Yarrow.
- Wormwood.
- Plantain.
Herbs must be taken in equal proportions to obtain a healing mixture. A decoction is prepared at the rate of 5 grams of mixed plants per 100 ml of water. The extract is infused for 6 hours, after which it is ready for use in the morning before meals.
Causes of the disease
Fungal infections are transmitted from sick people and pets to healthy people. It must be remembered that germs constantly attack the skin, but not all people get sick. Fungus on the feet and in the spaces between the toes is more common among those who are at risk, are not treated correctly with antibiotics, and do not comply with personal hygiene requirements.
Attention! Fungal spores persist for several weeks in scabs and scales of the epidermis, especially with high humidity on the floor in the bathroom, shower, or around the pool.
Increase your chance of getting a fungal foot infection:
- heavy sweating;
- immune disorders;
- hormonal imbalance;
- thyroid diseases;
- cracks, abrasions of the skin, wounds on the legs;
- deficiency in the body of vitamins A, C, and the microelement zinc;
- metabolic disorders;
- diabetes;
- overweight.
Shoe care and prevention of foot fungus
Foot fungus is an insidious and serious infection. To get rid of it forever and not get infected again, you should follow simple rules:
- It is undesirable to try on someone else's shoes, much less wear them for a long time. If you are invited to visit, then refrain from offering to wear slippers; it is better to stay in socks or take your home shoes with you.
- You need to maintain your immune system in good condition, take vitamins, and maintain a healthy, balanced diet.
- At the workplace in the cold season, it is better to change into replaceable shoes to avoid excessive sweating, which is an excellent “soil” for the appearance of fungus.
- When visiting the sauna or swimming pool, you must bring your own flip-flops and slippers.
- After bathing, you should dry your feet, paying special attention to the areas between the toes.
- You need to change your tights, socks, and stockings every day.
- You should not share personal items such as a washcloth, nail file, nail scissors, etc.
- It is not advisable to try on new store-bought shoes on bare feet, because a person infected with a fungus may have worn them before you. It is better to have a nylon or cotton sock with you.
- Pay attention to your feet, properly caring for them, and the fungus will not be scary.
- How to take vitamin E in capsules and liquid form correctly
- Lose 10 kg in 2 months
- Competitions for a fun company
Symptoms and diagnosis of the disease
In the area of the skin where the fungus develops, a slight itching is initially felt, but many do not attach importance to this symptom. This is followed by swelling, redness and peeling of the skin, small blisters and maceration (wetting of the epidermis) may appear. Cracks and erosions often appear; when skin flakes peel off, a burning sensation is felt and an unpleasant odor appears.
Attention! Signs of a fungal infection are first observed in the space between the fourth and fifth toes of one foot.
When conditions are favorable for the fungus, the primary lesion expands, persistent itching appears, which intensifies in the heat and when the feet sweat. The skin in the affected area is constantly inflamed and irritated, covered with white scales and scabs. After they are cleansed, burning and pain occur.
Diagnosis of the disease is carried out by a dermatologist or mycologist based on an external examination of the patient and laboratory tests to identify a fungal infection.
Diagnostics
To accurately identify the type of fungus that caused the wounds between the fingers, you need to go to a dermatologist. If there are indications, the doctor will refer you for examination to an infectious disease specialist and mycologist. First of all, a visual examination of the affected limb will be carried out, after which a primary diagnosis will be made. The doctor will also take tissue samples for histological examination, which can accurately determine the type of virus. And its resistance to medications. It is very important that a thorough diagnosis be carried out, because wounds between the fingers can be not only fungal, but also the following:
- psoriatic;
- impetigo;
- eczema;
- allergic, including dermatitis;
- keratodermatitis;
- dermatous and so on.
After a microscopic examination, it can be determined that a mixed type of infection is progressing in the body, then the treatment regimen will be radically different from that carried out for a fungal infection.
Local treatment with antiseptic agents
The dark purple crystals of potassium permanganate are shaken with warm water to create a concentrated solution. It is added to water and taken in foot baths, or cotton pads are soaked in the liquid and used as lotions.
Antiseptics and antimicrobial substances will help get rid of fungus:
- Alcohol solution of iodine.
- Sulfur-salicylic ointment.
- Salicylic alcohol.
- Potassium permanganate.
- Boric acid.
- Resorcinol.
- Fukortsin.
Attention! Antiseptics relieve itching of the skin and limit the spread of infection, but these medications cannot completely get rid of the fungus in advanced cases.
Iodine tincture has a strong antimicrobial effect. Before treating the fungus with this remedy, it is necessary to lubricate the healthy skin around the peeling area with Vaseline.
Salicylic ointment is better suited for treating the hyperkeratic form of foot fungus. The active substance in the composition has an antiseptic effect. The product softens scabs, relieves inflammation and pain, and facilitates cleansing the skin of parasite waste products.
Application of traditional methods
Methods for treating fungal infections related to alternative medicine are used in combination with medications. As an independent therapy, traditional methods are effective only at the initial stage of development of the disease, when the area of the affected areas of the skin is small and the symptoms are not pronounced.
To treat mycosis between the toes, various homemade remedies are usually used.
Baths
Effective bath recipes:
| Bath name | Recipe | Features of use |
| Euphorbia |
| Immerse your feet in the bath and wait 40 minutes. Perform procedures once every 3 days |
| Salt-soda | Mix 1 tbsp in 1 liter of warm water. l. table or sea salt and the same amount of baking soda | Dip your feet into the solution and hold for 30 minutes. Do the procedures daily until symptoms disappear |
| Wormwood |
| Keep your feet in the broth for 30 minutes. Do procedures every other day |
| With celandine |
| Immerse your feet in the infusion and hold for at least 15 minutes. Repeat the procedure every other day |
| Soda | Dissolve 2 tbsp in 1 liter of warm water. l. baking soda |
|
| Vinegar | Pour apple or wine vinegar into a wide container |
|
| Coffee shop |
|
|
Lotions
Lotions that effectively help cope with fungal infections:
| Means | Recipe | Features of use |
| Onion juice | Squeeze the juice from 1 onion, after passing it through a meat grinder |
|
| Potassium permangantsovka | Dissolve several crystals of potassium permanganate in warm water so that the solution acquires a faint pink color. |
|
| Apple vinegar | Soak a cotton swab in 9% vinegar |
|
| Vinegar | Soak a cotton swab in wine vinegar |
|
| Tea with vinegar |
| Moisten a cotton swab and apply to the affected area overnight |
Ointments
Effective homemade ointments against interdigital mycosis:
| Name | Recipe | Features of use |
| Garlic ointment |
|
|
| Onion ointment |
|
|
Birch tar
The use of birch tar gives a good result at the initial stage of mycosis development:
- Steam your feet well in hot water.
- Apply a generous layer of birch tar to areas with mycosis.
- Wrap with a towel or other natural fabric.
- Leave for 2 hours.
- Do not wash off for 2 days.
The procedure must be repeated 5 times. At the first signs of illness, this method of treatment allows you to get rid of the infection without resorting to medications.
Local treatment with antifungal drugs
They get rid of fungus at home using pharmaceutical sprays, ointments, gels and creams. In difficult cases, medications in tablets prescribed by a dermatologist are additionally taken orally.
Fungoterbin
This is the name of the line of drugs based on the fungicidal substance Terbinafine. They produce spray, gel and cream Fungoterbin. There is the same drug in tablets. The treatment course for uncomplicated forms of fungus is 1 week.
Lamisil
Antifungal drugs are produced under this trade name in the form of a spray, solution, gel, ointment, cream. The active substance in the composition is Terbinafine.
Bifosin
The active ingredient in the cream, solution and spray is Bifonazole - an effective fungicidal agent. It is recommended to use for treatment and prevention for 3 weeks.
Efficacy of drugs
Antifungal agents in various dosage forms are considered highly effective, since they contain components that have fungicidal and fungistatic effects.
Penetrating into the deep layers of the skin, the active ingredients have a detrimental effect on pathogenic microorganisms and stop their growth. With regular use of antimycotic agents, fungi die, and the skin takes on a healthy appearance.
Systemic therapy
In most cases, only external use of antifungal agents is sufficient. It is recommended to ask your doctor about which drug is best to use. If a fungal infection develops against the background of severe internal diseases, then local and systemic therapy is combined.
It is important! The use of medications and alternative medicine recipes must be combined with proper foot skin care.
Treatment with antifungal drugs taken orally will be required in advanced cases. Additionally, the doctor prescribes immunostimulants and vitamin-mineral complexes. Complete healing takes several months, and only if the chosen remedy corresponds to the form and stage of the disease.
Basic principles of drug treatment
Before starting a therapeutic course using antifungal medications, an infected person needs to become familiar with the basic principles of treating a fungal disease.
In order not to harm your health and speed up recovery, treatment with medications should be carried out in compliance with the following rules:
- Use only those products prescribed by the attending physician after carrying out diagnostic measures and receiving test results.
- Read the instructions carefully, read the list of contraindications and side effects.
- Apply the selected preparation to previously cleansed dry skin regularly, at least 2 times a day.
- Do not stop treatment immediately after the disappearance of visible symptomatic manifestations of mycosis.
- Additionally, treat shoes and socks with special antifungal sprays that destroy the infection.
Important!
If the disease has reached an advanced stage, simultaneously with the use of topical products, you should take antifungal drugs prescribed by a dermatologist in tablet form.
Treatment with folk remedies
At home, they independently use antiseptics and fungicides. Treatment of fungus between the toes with folk remedies helps reduce discomfort in the first week.
Foot baths
A soda solution for the treatment of interdigital fungus on the hands and feet is prepared from 2 liters of water, 2 cups of table salt and 1 tbsp. l. soda
Baths with decoctions of medicinal plants are useful for fungus between the toes: celandine, wormwood, oak bark, birch leaves, willow bark. Brew the raw material and boil over low heat, or preferably in a water bath, for 5–15 minutes. The proportions of grass and water are 1:5.
Sometimes more plant materials are brewed to increase the concentration of biologically active substances in the solution, increasing the impact on the causes of the disease. Baths with plant decoctions or soda solution are done in the evening. Take the procedure for 30 minutes.
Lotions and compresses
Propolis and its tincture are strong folk remedies for fungus on the skin between the toes, having an antimicrobial and healing effect. Use 10 or 20% alcohol tincture for lotions and compresses. You can prepare the product yourself or purchase it at a pharmacy.
Vinegar - table vinegar from the store or homemade from apples and cherries - helps relieve itching and unpleasant odor. The acid changes the pH of the skin, which stops the growth of the fungus. They make lotions with vinegar, calendula tincture, and strong tea leaves.
Symptoms of the disease
The causative agents of mycosis can be:
- mold fungi;
- dermatophytes;
- yeast fungus.
Depending on what kind of fungus provoked the disease, the symptoms of the disease will differ:
- Mold fungus develops mainly in summer, in hot and humid weather, when the skin becomes dry.
- The disease is caused by yeast fungi, it will spread not only to the areas between the fingers, but also to the nail plates.
- The disease, caused by dermatophytes, begins to manifest itself on the little toe or areas near the big toe, and then spreads throughout the foot.
Symptoms of mycosis differ depending on the stage of the disease:
- At the initial stage of the disease, not every patient will suspect a fungal infection. During this period, the disease manifests itself with small cracks, a feeling of itching between the fingers, increased peeling and dryness in the affected areas.
- In the active phase, if untreated, areas of redness form between the fingers, peeling becomes more obvious with the appearance of fluid-filled blisters. There is an inflammatory process, tissue swelling and coarsening of the epidermis.
- The advanced stage is characterized by the appearance of pus, inflammation, redness and swelling. My feet itch unbearably. The skin becomes covered with deep cracks and constantly gets wet. Ulcers and sores look like one continuous wound. The nails begin to peel off from the bed.
Detecting mycosis at home is quite simple. To do this, you need to immerse your feet in a solution of potassium permanganate for a few seconds. Potassium permanganate will color healthy skin a pinkish tint, while areas with fungus between the toes will remain the same color. This reaction is associated with structural changes in the skin.
Prevention
It is necessary to observe the rules of personal hygiene and care for the skin of your feet. Socks should be washed at a temperature not lower than 40°C. It is recommended to treat the inside of shoes with a formaldehyde solution or a special spray. It is advisable to choose shoes made from natural materials; in summer, wear sandals and sandals more often.
If the areas between the toes are wet and very itchy, then use products that do not increase sweating. These are spray, lotion and powder (powder). For the dry form of the fungus, a good option is an ointment or cream. Before applying the product, be sure to clean the affected area of scales and scabs using a warm foot bath.
Signs of interdigital fungus on the feet
The initial stages of the fungus often do not have severe symptoms. Itching between the fingers almost does not bother the patient, there is practically no discomfort. This nuance often leads to the fact that an infected person ignores the mild manifestations of a dangerous disease. As a result, the fungus progresses and develops, affecting not only the skin on the foot, but also the nails. If you experience the slightest discomfort, you need to listen to your body, seek help from a dermatologist and begin immediate treatment for the fungus.
There are several main symptoms of mycosis:
- the skin between the fingers begins to noticeably peel off;
- sweating of the feet increases;
- cracks appear on the skin;
- itches between the toes, itching and pain often occur;
- seals form on the sole;
- large, gray or yellow spots form on the fingers and feet (they increase if the fungus is not cured in time).