Many of our patients seek advice regarding cracked and chafed skin between their toes. Especially in summer, the problem seems to grow. Patients notice small whitish blisters or ragged skin on their own or their children's legs and think it is ringworm.
However, in most cases we can reassure: dermatophytosis is a relatively rare disease in our latitudes, provided hygiene standards are observed. Most often we deal with maceration.
What is maceration?
On hot summer days, almost all the feet sweat. One of the purposes of sweat is to cool the body, and therefore it is completely natural in the summer. Then the whole body, and therefore the feet, cool down. After all, there are over 500 sweat glands on the soles of our feet.
However, too much sweat on the feet can cause maceration, that is, softening of the epidermis. The macerated epidermis loses the features of vital tissue and becomes dead tissue.
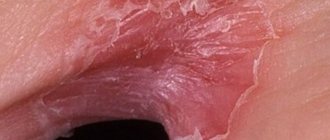
Maceration in the interdigital spaces appears as cracked, uneven whitish epidermis. If this occurs on skin with hyperhidrosis, the skin around the maceration becomes intensely red and noticeably moist.
Creams for flaky skin
To moisturize the skin between your toes that has begun to peel, you need to use a cream that contains nutrients and fat.
Such creams are a universal product for caring for problem skin. Their use helps to increase skin elasticity, soften it and enrich it with nutrients.
It is important to know! A quality cream does not have to be expensive. Its effectiveness and benefits for your skin are determined by the components included in its composition, and not by the cost. A good choice would be a cream containing magnesium and selenium, to which mineral water has been added.
To moisturize the skin between your toes that has begun to peel, you need to use a cream that will contain nutrients and fat.
If the skin is peeling, a cream with extracts of various medicinal herbs (chamomile, yarrow, nettle) is suitable. It is better if the cosmetic product is rich in vitamins A and C, as well as ceramides.
Why does the skin between my toes crack?
In summer, maceration often occurs on normal skin, which usually does not sweat much. The reasons for this are increased air temperature, and, consequently, skin temperature, lack of air circulation between the fingers and accumulation of moisture. The friction of the toes against each other and the pressure of the surface of the skin on the soles of the shoes cause cracking of the thin and delicate epidermis between the toes.
Sometimes the cracks in the transitions from the interdigital surfaces to the sole are deep. We then see whitish, uneven areas of the epidermis surrounding the crack in the skin, which is often painful. Then we are faced with a wound that requires fast and effective treatment, because not only fungi, but also bacteria can penetrate through an open wound.
Maceration can occur on all areas of the foot. Calluses, plantar indentations and the area on the lateral surfaces of the toes can become macerated, that is, softened by sweat and other fluids.
Prevention
An important condition for prevention is the right shoes. It should not be too narrow or wide. Shoes are selected according to the season. In summer, it is better to wear open models that will not lead to excessive sweating of the feet. The best option for any time of year is shoes made from natural materials. Other measures to prevent cracking:
- maintain proper nutrition;
- If your feet are very sweaty, wash them several times a day;
- do not wear someone else's shoes;
- regularly lubricate your feet with a softening cream;
- massage your feet with different essential oils;
- choose socks only from natural materials;
- When visiting the pool and sauna, use your own hygiene products and wear your own slippers.
Hypergranulation and maceration
Maceration is often accompanied by ingrown nails and hypergranulation. The area is always wet, and therefore an infection easily attaches to the wound, which quickly moves from the side to the back, that is, the base of the nail plate. A purulent paronychia forms with pronounced redness and pain.
If timely treatment is not carried out, paronychia can spread to the finger tissue and cause panaritium, inflammation of the lymph nodes.
If maceration can be treated in a podologist’s office, then associated complications require contacting a surgeon.
Therapeutic ointments to relieve skin redness
Every home medicine cabinet should have an ointment containing natural herbal ingredients. This product effectively copes with redness and flaking of the skin, itching and other symptoms of skin diseases. Such gels can be easily purchased at a pharmacy.
Read the new article in the section: Gallstone disease: treatment without surgery and diet
Your attending physician will help you decide on the choice of a specific remedy. Pay attention to ointments that contain a complex of vitamins and essential oils.
This product will quickly cope with skin redness and swelling, increase the protective properties of the skin, relieve you of itching, soften the skin and improve the process of cell renewal.
What is the difference between maceration and mycosis?
In contrast to maceration, mycosis is sometimes caused by Trichophyton rubrum or Trichophyton interdigitale. Mycosis on the feet differs from maceration in both appearance and smell. The smell of mycosis is very characteristic and is easily recognized by an orthopedist.
The appearance of mycosis is distinguished by its yellowish-brown color and the presence of additional, not yet cracked, microscopic bubbles that appear next to the already cracked and jagged ones. The vesicles are filled with liquid containing fungal spores. Often they are so small that only the experienced eye of a podiatrist can see them with a magnifying glass. Deposits of necrotic, fungal epidermis can stick together, becoming a threat to the formation of interdigital ulcers, which are very painful and difficult to remove and heal.
Oil foot wraps
Foot wraps can not only restore a healthy appearance to the skin, but also help remove toxins, enlarge pores and improve blood circulation . With this procedure, you can restore the tone and firm appearance of the skin of your legs in a short time.
Wraps can be carried out not only in a beauty salon, but also at home. The procedure should not last more than 40 minutes. Any medicinal mixture should be applied in a dense layer to prevent its rapid absorption and subsequent irritation of the skin of the feet.
The procedure is carried out on an empty stomach. Immediately before wrapping, the skin of the legs should be well steamed and cleaned of the keratinized layer of epidermal cells.
You might be interested to know about: Quick-acting laxative in tablets
A full course of oil wrap lasts up to 3 weeks. It is recommended to carry out procedures no more often than every other day. In combination with dietary nutrition, regular physical activity and other cosmetic procedures, oil wraps will provide maximum effect for the skin of your feet.
Why is it important to diagnose and treat maceration?
Eliminating maceration is the basis of foot health: eliminating unpleasant odors and the risk of infections.
Recommendations:
- Medical pedicure. Removal of keratinization and affected epithelium using a hardware method.
- Treatment of an ingrown toenail. (If pathology is present). The method is selected individually and depends on the position of the nail and the condition of neighboring tissues.
- Foot hygiene. Regular independent and proper care reduces the risk of infection and maintains the results of a hardware pedicure. Recommendations for care will be given individually by a podiatrist.
- Comfortable shoes. According to season and size, made of natural materials and orthopedic insoles.
If, due to maceration, the interdigital spaces are affected by mycosis, along with a medical pedicure, it is advisable to consult a dermatologist to receive pharmacological treatment.
Cracked heels
Fungus
Iron deficiency
Diabetes
19770 November 18
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Cracked heels: causes of occurrence, what diseases cause them, diagnosis and treatment methods.
Description
Cracks in the heels are linear tears in the skin that occur as a result of loss of elasticity and thickening of individual areas. Most often, cracks form in places where the skin is naturally folded and stretched and can be of varying depths. A person often complains of itching, burning, pain, and discomfort while walking.
For most people, cracked heels are a problem related to the appearance of the feet. However, in some cases they can cause considerable discomfort - they can be painful, lead to bleeding, and as a result there is a risk of infection.
In addition, cracked heels are one of the symptoms of certain diseases.
Types of cracked heels
The following types of heel cracks can be distinguished:
- superficial and deep;
- dry (arising from excessively dry skin) and wet (arising from excessively wet skin - this phenomenon is called maceration);
- uninfected and infected;
- resulting from:
- endogenous causes (dermatological diseases, hormonal disorders, diseases of the gastrointestinal tract; associated with a lack of vitamins, microelements);
- external factors.
Possible causes of cracked heels
The most common causes of cracked heels include conditions associated with local physical effects on the skin of the foot: exposure to the sun, wind and cold, temperature changes, chlorinated water, dry air, poor hygiene, excessive care (frequent peeling - removal of the upper stratum corneum of the skin), use of alkaline soap, improperly selected shoes.
However, in some cases we may be talking about general conditions that affect the skin of the heels: smoking and alcohol abuse, fasting, unbalanced diets, small amounts of fluid to drink, congenital skin characteristics (dryness, sensitivity), pregnancy, menopause, aging of the body.
Pathologies that provoke the appearance of cracked heels include fungal infections, dermatological diseases (psoriasis, ichthyosis), diseases of the gastrointestinal tract, helminthiases, conditions of deficiency of vitamins and microelements (iron deficiency anemia, hypovitaminosis), hormonal disorders (thyroid diseases, diabetes mellitus). diabetes), as well as diseases leading to impaired trophism (nutrition) of the lower extremities (impaired innervation and blood supply).
As a result of negative environmental influences (sun, wind, etc.), the skin loses its elasticity, becomes thinner, and the function of the sebaceous and sweat glands decreases. As a result, growths of thick, rough, dry skin appear on the heels. Against the background of increased pressure on the foot (prolonged standing, wearing tight shoes, obesity), cracks may appear. Failure to comply with the drinking regime and lack of vitamins aggravates the problem.
Cracked skin is not only an aesthetic problem, over time it can cause pain when walking, cracks can bleed and become infected. Poor hygiene and the presence of concomitant diseases complicate the problem.
Insufficient levels of thyroid hormones (hypothyroidism) leads to a decrease in metabolism in the body, blood supply to tissues, and the function of sweat and sebaceous glands. Dry and rough skin on the feet becomes prone to excessive keratinization and cracking.
Psoriasis is a chronic systemic disease affecting the skin, nails, and joints. It is characterized by the appearance of small red spots with scales (psioriatic plaques) rising above the skin, which tend to enlarge, merge, and thicken. Thick and hard skin on the feet itches and cracks. Since psoriasis of the feet is associated with a high risk of trauma to the elements of the rash, they often become infected.
Psoriatic plaques on the skin of the feet Diabetes mellitus is a chronic endocrine disease, which is based on metabolic disorders due to insulin deficiency and the resulting high level of glucose in the blood. The long course of the disease leads to damage to nerves and blood vessels with impaired innervation and blood supply to tissues. If the feet are not properly cared for, ulcers and cracks form on their surface, and patients with diabetes need more time to heal.
Foot fungus can be another cause of cracked heels. The disease is characterized by redness, itching, peeling and thickening of the skin, and the appearance of cracks of varying depths and sizes. An unpleasant odor may be present. Based on the picture of the disease and the patient’s complaints, the doctor suggests a fungal infection of the feet, but to confirm the diagnosis, a laboratory test is necessary to determine the presence of the pathogen in the affected area of the skin.
Foot fungus
Keratoderma is a group of skin diseases characterized by disruption of the keratinization process. With this disease, keratosis of the palms and soles is observed. Keratoderma can be diffuse (continuous lesion of the skin of the palms and soles) and focal (the lesion is located in the form of islands, linearly, pointwise).
Keratoderma of the skin of the feet
In children with Unna-Tost keratoderma (congenital ichthyosis of the palms and soles), excessive keratinization of the skin is observed at 1-2 years of age. The disease begins with mild thickening of the skin of the palms and soles. The horny layers are smooth, yellowish in color. Deep cracks may form.
Acquired ichthyosis develops at a later age and is manifested by dry and rough skin with a large number of scales. The skin is affected not only on the torso and limbs, but also on the palms and soles. Acquired ichthyosis is a sign of other diseases (hypovitaminosis A, malignant neoplasms of internal organs, mycosis fungoides, etc.).
Which doctors should I consult for cracked heels?
If changing tight shoes and performing hygiene procedures do not help get rid of cracked feet, you should consult a podiatrist (a doctor who diagnoses and treats foot diseases).
To exclude diseases that provoke the occurrence of cracked feet, you may need to consult a dermatologist or rheumatologist.
Diagnostics and examinations for cracked heels
To determine the causes of cracked heels, the doctor may prescribe a set of laboratory and instrumental diagnostic methods.
- Tests for fungal infections of the skin of the feet.
Homemade masks for dry skin on feet
Mix freshly squeezed tomato juice in equal proportions with oil. Apply the resulting mixture to your feet and ankles.
Oranges, beaten in a blender with starch and any vegetable oil, can be used as a nourishing base for a moisturizing mask. The mask should be washed off with cool water 30 minutes after applying it to the skin.
A mask of orange and vegetable oil perfectly moisturizes the skin
Conclusions about crack therapy
In conclusion, it is worth recalling that timely medical intervention and vigilance towards developing symptoms can eliminate side effects and complications. For example, without the timely use of pharmaceuticals, the risk of complications of the intertriginous or dyshidrotic form increases. And they are much more difficult to get rid of.
Combine treatment with baths and official medications - ointments, gels, sprays or even tablets for oral use. And don't forget about taking care of your skin. It must be washed regularly and treated with special heel creams like Gewohl.
It is important to prevent fungal diseases and wear comfortable shoes. This will reduce the risk of crack recurrence. And during treatment of existing ones, be sure to listen to the dermatologist’s prescriptions. This is the only way to cure cracks in the little finger in a short time.
Baths for additional effect
The main side method for treating cracks is herbal baths. You can add any herbal components to them that stimulate the restoration of the skin. The best recipe with common ingredients is a bath with medicinal chamomile tincture. It normalizes blood flow in the foot and helps heal even a deep crack.
You can replace chamomile with St. John's wort, celandine, pine needle oil, or even slightly concentrated urea.
To prepare, 150 grams of dry chamomile is poured with a liter of boiling water and infused for at least half an hour. Then the feet are immersed in a basin with this liquid and steamed for no more than 15 minutes. If you increase the procedure time, you can only further injure the dermis.
The same feature applies to wax masks, which are made after steaming your feet.
Sometimes, to enhance the effect, alcohol tincture is poured into the baths. But too much alcohol can lead to peeling, dryness and irritation of the skin near the crack. Only a moderate number of baths can contribute to a speedy recovery. It is important to combine them with traditional approaches to therapy.
The best products to relieve skin irritation
Steam baths help to cope with skin irritation. Boil 1 liter of water in a small container, place the area of problematic skin over it, covering it with a thick towel on top. To ensure that the procedure has an anti-inflammatory and calming effect, you can add finely chopped hops or chamomile to boiling water.
Parsley compress will help relieve skin irritation
Another available remedy for skin irritation is a compress made from parsley decoction. You can apply a piece of gauze soaked in this decoction to the skin, or pour it into ice molds, and after the liquid has completely frozen, massage the ice into the irritated areas of the skin.
How to recognize diaper rash: symptoms and signs
At the initial stage, diaper rash between the fingers does not cause severe discomfort. There is slight redness and irritation of the tissues between the ring and little fingers, thumb and middle fingers. Ignoring the problem will result in even greater damage to the epidermis. Due to the proliferation of fungus and accumulation of moisture, a pungent odor occurs. As diaper rash progresses, the clinical picture is replenished with the following symptoms:
- erythema (redness);
- peeling;
- ulcers;
- pinpoint bleeding;
- putrid smell.
In addition to local manifestations, patients complain of burning, itching, pain when walking, and a feeling of tightness of the skin. The severity of the signs of the disease is determined by the stage of the inflammatory process:
- Easy. Small red spots and areas of peeling appear on the legs. When walking for a long time, painful sensations and itching worsen.
- Average. Diaper rash takes on a bright red hue. The skin swells and small cracks form on it.
- Heavy. In the area of the fingers, pinpoint ulcers appear that bleed from time to time. In some cases, there are suppurations caused by fungi or bacteria.
Diaper rash on the legs is often accompanied by septic inflammation of the tissues. The addition of infection is indicated by:
- elevated temperature;
- increased sweating;
- fever;
- body aches;
- decreased appetite.
At the first manifestations of the disease, contact a dermatologist. After examination, the doctor determines the degree of damage to the legs and prescribes medications suitable for treatment. If bacterial flora is involved, antibiotics are used, and if fungal flora is present, antimycotics are used.