Recipes for eye masks against milia
Masks are an affordable and effective cosmetic product against milia.
Their task is to help exfoliate dead cells, which often cause unpleasant formations to appear. To prepare masks, you can use products that you always have on hand in the kitchen.
Gelatin film mask
- Mix one tablespoon of gelatin and milk.
- Place the mixture in the microwave and heat for 10 seconds until the gelatin dissolves.
- Apply the mask with a brush to problem areas of the face.
- When the film hardens, remove it and repeat the procedure again.
- Wipe the skin with lotion or apply cream with tea tree oil.
Tomato mask
This mask is rich in vitamin C and not only helps fight milia, but also returns a healthy complexion to the skin. The product acts as a chemical peeling and softens skin cells that do not allow the contents to come out.
Leave the tomato pulp for 7-8 minutes, then rinse with warm water and apply moisturizer. This mask can be done once a week.
Milk mask
- Mix three tablespoons of milk, a tablespoon of lemon juice and a packet of dry yeast.
- Mix well and apply to the skin in a circular motion, leave for 15 minutes. Wash off the mask with warm water and apply cream.
Homemade scrubs
To make homemade scrubs you will need inexpensive and readily available products.
Oatmeal scrub
This is one of the most effective in cleansing the skin in general and in the fight against milia in particular. We prepare it as follows:
- Grind the oatmeal finely, but not into dust.
- Add honey and sugar to them. All components must be in equal quantities.
- Mix the ingredients and massage into the skin for a couple of minutes.
- Then we wash with cool water and apply facial care products.
Soda scrub
If you have oily skin and are not allergic to baking soda, use it to make a scrub. Before use, do a test on your wrist and only then can you use it on your face. This scrubbing method is not suitable for the upper eyelids.
- We foam the baby soap and distribute the foam on the face.
- We take a cotton pad and apply a little soda on it, use this disc to gently massage the face, no longer than three minutes.
- Rinse off the scrub with cool water and apply a moisturizer to the skin. There may be some redness on the skin, but it will disappear soon.
Is there an alternative - effective removal of milia?
Not everyone can solve the problem with home remedies. In this case, you will have to seek help from a dermatologist or cosmetologist. Experts today offer several methods for eliminating milia.
Medical procedures
Among the medical procedures performed by doctors, the most effective are:
- Electrocoagulation of milia. Used to remove formations on the eyelids and face. During the procedure, the doctor uses an alternating high-frequency current, which cauterizes the milia papules. After electrocoagulation, a crust forms at the site of exposure; it goes away within a few days. To speed up healing, it is recommended to treat the area with an antiseptic and not wet it with water.
- Removal of milia with laser. Laser removal of milia is performed under local anesthesia. A small scar remains at the treatment site, which quickly disappears. The use of a laser minimizes the risk of infection and tissue injury. This is the optimal solution for large lesions.
Salon treatments
In beauty salons and beauty salons, specialists can offer the following procedures:
- Peels. Depending on the characteristics of the skin, the cosmetologist selects suitable products for exfoliating the epithelium. Peeling can be superficial, medium and deep. The specialist applies fruit acids or more powerful drugs, such as trichloroacetic acid, to the skin. During the procedure, dead skin cells are removed, making room for the contents of the milia to exit.
- Mechanical facial cleansing. During this procedure, the specialist punctures the papule with a special sharp needle. After this, he pushes out the contents with a special spoon. A small crust at the puncture site disappears within a day.
After removal of the formation, it is worth taking care of prevention.
VIDEO DESCRIPTION» alt=»»>
To prevent the problem from returning again:
- Remember hygiene - take care of your skin every day, buy high-quality cleansers.
- Include fresh fruits and vegetables in your diet and drink more water.
- Visit a cosmetologist at least once a month.
- Avoid oil-based makeup.
- Don't get carried away with tanning in summer and solarium in winter.
If you take good care of yourself and your health, milia will definitely recede!
Wen, millet or white dots at the site of the scar: causes of appearance, treatment
It happens that a person does not have such problems as long as after a burn, blow or operation there is a scar on which a wen appears over time. Such a wen, millet or milia is closely associated with a skin disease or possible inflammation, abrasion, burn and scar. This occurs only in those parts of the body where the skin has previously been damaged as a result of illness or injury. If dead skin cells get trapped under the top layer of skin during this injury, they can encapsulate there and leave a single wen.
That is, this is again an abundant work of the sebaceous glands. Such milia are considered secondary - they arise precisely in places of damage. Primary clearings form spontaneously and disappear just as unexpectedly. For example, on the skin of a baby as a result of contact with a new environment, or on an adult after contact with ultraviolet radiation.
Other possible reasons for the appearance of milia at the site of a scar after surgery are:
- due to strong skin tension
- or as a result of their incorrect connection/fusion
- tissue regeneration and individual predisposition
- possible inflammation, which is often accompanied by itching and pain
In this case, there is no need to panic; in most cases, it resolves on its own. But it wouldn't hurt to consult a dermatologist. If milia bothers you or causes discomfort, then you should visit a surgeon for timely removal. Most often, such a wen is removed mechanically.
They may also prescribe ointments for resorption of scars and these same milia:
- Contractubex
- Dermatix
- Heparin ointment
- Hydrocortisone
- Vishnevsky ointment
And even more so, it is forbidden to open them with a needle at home!
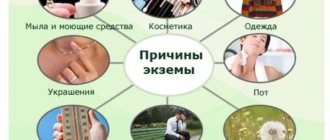
Causes
Millet can be primary or secondary, depending on the etiological factors.
Primary occurs on the skin of the eyelids in people with a hereditary predisposition. Secondary develops against the background of a disease or injury - accidental household or during cosmetic procedures.
Possible reasons for the appearance of millet:
- autoimmune diseases;
- metabolic disorders;
- incorrectly selected eyelid cosmetics;
- disorders of the gastrointestinal tract;
- endocrine system disorders;
- damage to the eyelids;
- seasonal hypovitaminosis;
- oily skin type;
- burns or excessive sun exposure.
The appearance of millet, whiteheads on the skin of the lower or upper eyelid depends on the functioning of the sebaceous glands. They are most affected by the endocrine system and the effects of cosmetics.
Features of milia treatment
Rashes are often eliminated using cosmetic preparations with an exfoliating effect. For this purpose, creams and ointments that contain urea and salicylic acid can be used. When they are used, miliary cysts spontaneously emerge on the surface of the skin.
However, often such therapy does not bring a positive result and it is necessary to resort to more radical measures. It is possible to remove the white wen in the eye area in the office of a specialist who, after an examination, will select the most effective treatment.
Mechanical removal
To remove rashes in the eye area, a treatment method such as a mechanical method can be used. The essence of the technique lies in the fact that the skin is initially pre-cleaned. After this, the epidermis is disinfected, and then the milia are removed. Using a sterile needle, the skin is punctured under the desired node. As a result, it is possible to slightly undermine the epidermis and remove the body of the acne formation.
This procedure is considered quite painful and causes severe discomfort to the patient. In addition, a wound may form in the area where the needle is inserted under the skin, which requires careful care. Proper wound care can speed up the complete healing of the epidermis.
Electrocoagulation
Electrocoagulation
One of the effective ways to combat rashes on the dermis is electrocoagulation. During the procedure, damaged areas of the dermis are exposed to high-frequency electric current. After coagulation, a crust forms on the surface of the epidermis, which cannot be removed independently. After a while, it disappears and leaves no trace behind.
The duration of the procedure depends on the area being treated and usually does not exceed 15-30 minutes. If the procedure is carried out correctly, there is no need for re-therapy. In some cases, a person develops too many rashes on his face, so a month later, repeated electrocoagulation is required.
Compared to treating formations mechanically, electrocoagulation has many advantages. This procedure allows for a limited effect on individual rashes and does not harm nearby tissues. In addition, electrocoagulation makes it possible to remove milia, which are localized deep in the dermis.
Laser removal
Laser
Laser coagulation is considered one of the most effective methods for removing large clusters of acne. With the help of the procedure, it is possible to quickly remove formations and avoid trauma to nearby tissues. After the procedure, the risk of scarring is minimal, and the recovery process is painless and quick.
It is not allowed to remove milia using a laser in the following cases:
- oncological tumors;
- herpes in the acute stage;
- autoimmune pathologies;
- pregnancy;
- lactation period;
- rise in body temperature;
- hypertension.
Immediately after completion of the procedure, you are allowed to go home. Minor swelling and redness of the treated areas may remain on the patient's skin for two weeks.
Cryotherapy
Cryotherapy
During cryotherapy, controlled destruction of milia is observed. Problem areas of the skin are exposed to low temperatures, and liquid nitrogen is used to remove milia.
During this treatment, acne formations are removed due to the formation of ice in the affected cell. The lower the temperature of liquid nitrogen, the faster the process of cell destruction occurs. Cryotherapy is performed in cycles of freezing, followed by thawing of the milia.
The advantage of cryotherapy with liquid nitrogen is the low risk of infection of damaged tissues. The treatment is carried out without the use of local anesthesia, and there is no scarring after it. In addition, no special wound care is required after cryotherapy.
However, minor bleeding may occur with this treatment method. In addition, blisters, scars and increased hyperpigmentation may form in the area of the removed acne.
Problems of the elderly. Eyelid diseases: diagnosis and treatment
| Figure 1. Entropion of the upper eyelid with cicatricial pemphigus |
What are the most effective methods to control the development of blepharitis? When to operate on patients with entropion and ectropion? What signs of eyelid tumors indicate their malignancy?
The main function of the eyelids is to protect the cornea from external influences. The eyelids also maintain a constant environment for the eye, including protecting the tear film necessary for the functioning of the cornea.
For adequate functioning of the eyelids, it is necessary to have eyelashes of a certain length and shape, normal tone of the eyelid muscles, and intact blink reflexes. If at least one of these components is impaired, the ability of the eyelids to perform their functions is also impaired, which leads to serious visual impairment and, possibly, blindness. The most common diseases of the eyelids in old age are caused by involutional changes associated with aging, the development of tumors (both benign and malignant) and systemic diseases.
- Blepharitis
Blepharitis, inflammation of the eyelids, is a very common disease that can only be controlled, but not cured. Patients usually complain of irritation, burning, and a sensation of a foreign body in the eyes. Symptoms are severe in the morning and decrease during the day. Clinically, blepharitis is distinguished between anterior (involving the edges of the eyelids) and posterior (mainly affecting the meibomian glands), although a combination of both is usually observed.
| Figure 2. With entropion, eyelashes scratch the cornea |
Anterior blepharitis requires eyelid care and topical antibiotics. Eyelashes are cleaned with diluted baby shampoo or soda (a quarter spoon of soda per cup of cool boiled water; only a freshly prepared solution is used). Eyelid toileting should be done regularly. Antibiotics are applied to the edge of the eyelid for a short time, immediately after the hygiene procedure.
Posterior blepharitis is corrected with hot compresses and eyelid massage (to facilitate the outflow of stagnant meibomian gland secretions).
The course of systemic antibiotics, such as tetracycline, doxycycline and erythromycin, for meibomitis ranges from 6 weeks to 6 months. Their mechanism of action is unknown; they are thought to stabilize lipid secretion.
- Entropion
This is a violation of the position of the eyelid, in which the edge of the eyelid is turned inward towards the eyeball. Recognizing the condition is important because rolled up eyelids and eyelashes can damage the cornea, leading to ulceration and secondary infection.
Table 1. Diseases of the eyelids in old age
| Bacterial infections, inflammation | |
| Barley | Infection of Zeiss glands |
| Chalazion | Meibomian gland infection/inflammation |
| Meibomite | Induration/inflammation of the meibomian glands |
| Blepharitis | Inflammation of the edge of the eyelid |
| Viral infections | |
| Herpes simplex | Vesicular rash |
| Herpes zoster | Rash and blisters along the trigeminal nerve |
| Viral warts | Thread-like damage |
| Molluscum contagiosum | Umbilical lesions |
| Trichiasis | Eyelashes point backward, usually due to scarring on the eyelids |
| Blepharoptosis (ptosis) | Weakening of the eyelids |
| Dermatochalasion | Excess eyelid skin |
| Blepharospasm | Involuntary tonic and spastic closure of both eyelids |
| Entropion | Turning up the edge of the eyelid |
| Ectropion | Everting of the eyelid edge |
| Benign tumors | |
| Papillomas | Warts, seborrheic keratosis, actinokeratosis |
| Keratoxanthoma | Ulcer filled with keratin surrounded by rapidly growing hyperplastic tissue |
| Xantellasma | Yellowish lipid plaques in the medial area of the eye |
| Nevi | Pigmented formations |
| Malignant tumors | |
| Basal cell carcinoma | Firm, raised granular nodules with central ulcerations |
| Squamous cell carcinoma | Tumors with an uneven surface, newly formed or arising in areas of sunburn |
| Sebaceous carcinoma | Extremely malignant tumor masquerading as a chalazion, chronic blepharitis, or basal cell carcinoma |
Involutional (senile) entropion is caused by degenerative changes in the structure of the eyelid. These include horizontal weakness of the eyelid and/or canthus tendons, weakening of the eyelid retractors and orbital muscles, and atrophy of orbital tissue. Senile entropion usually affects the lower eyelids. The patient complains of irritation and soreness of the eyes; they may become red and inflamed. Sometimes clouding occurs in those places of the cornea that are damaged by eyelashes.
Treatment is carried out only in the presence of clinical symptoms and is most often surgical. It is aimed at restoring the function of weakened muscles that contract the eyelid. Temporarily, while awaiting surgical intervention, they resort to lubricating the cornea, as well as attaching adhesive tape under the lower edge of the eyelid (to prevent it from turning in).
Cicatricial entropion is associated with shortening and curvature of the posterior plate of the eyelid. The reason for this may be various autoimmune disorders (cicatricial pemphigus), inflammatory disorders, infections (trachoma, herpes), surgical interventions (enucleation), injuries (thermal, chemical, thermal).
It is more difficult to treat cicatricial entropion than involutional entropion. The goal is to eliminate chronic irritation of the eye through local lubrication, removal of eyelashes and keratinized areas, treatment of the underlying disease, surgical rotation of the eyelid along with the mucous membrane, and transplantation of other tissues (to replace damaged scar tissue of cartilage and conjunctiva).
- Ectropion
Ectropion is an abnormal position of the eyelid in which the edge of the eyelid turns outward from the eyeball. The lower eyelid is affected much more often than the upper eyelid. This condition can lead to keratopathies, conjunctival hypertrophy and lacrimation.
| Figure 3. Blepharitis is very common; it cannot be cured, but its development can be controlled |
Involutional ectropion, the most common cause of watery eyes, is caused by weakening of the muscles that contract the lower eyelid and the tendon of the corner of the eye. Treatment includes horizontal shortening of the eyelid size and tightening of the tendons; carried out when lacrimation or keratopathy develops.
Cicatricial ectropion is caused by scarring combined with stretching of the skin. Damage around the eyes and subsequent scarring can contribute to the formation of ectropion. To avoid this, it is necessary to place the scars parallel, and not perpendicular to the edge of the eyelid. Treatment consists of relaxing operations and tissue transplants.
Table 2. Types of blepharitis and their clinical manifestations
| Staphylococcal | Seborrheic | Meibomian | |
| Symptoms | Burning and itching | Burning and itching | Burning and irritation |
| Scales | Hard, brittle | Greasy | Greasy |
| Meibomian glands | Not changed | Changed (viscous plugs and swollen orifices) | Changed |
| Ulceration | Eat | No | No |
| Keratitis | Marginal superficial punctate keratopathy (MSP) | PTK | PTK |
| Hordeola | Styes often occur | Rarely | Chalazions are common |
| Conjunctivitis | Always | Occasionally | Always |
| Treatment | Eyelid hygiene, topical antibiotics | Eyelid hygiene, dermatitis treatment | Eyelid hygiene, hot compresses, systemic antibiotics |
| Note: PTC - superficial punctate keratopathy | |||
Paralytic ectropion develops as a result of damage to the seventh pair of cranial nerves, which leads to weakening of the lower eyelid, incomplete closure of the eyelids and infrequent blinking. The cornea becomes irritated and dry.
For treatment, ointments are applied topically and the temporal part of the lower eyelid is temporarily immobilized. To permanently immobilize the lower eyelid, surgery is performed - lateral tarsorrhaphy - or a loop is formed to support the lower eyelid.
In trichiasis, the eyelashes are usually directed towards the surface of the eye, which is often accompanied by chronic blepharoconjunctivitis or cicatricial conjunctivitis. Treatment includes mechanical epilation, electrolysis and cryotherapy to break up and remove the offending eyelashes, or surgery to retract the eyelashes away from the eyeball.
- Tumors of the eyelids
The first thing to do when a tumor of the eyelid is detected is to find out whether it is malignant. All excess tissue, except clearly inflamed tissue, is subject to histological examination. Malignancy is indicated by ulceration, induration, uneven surface, painless local telangiectasia, and irregular margins.
| Figure 4. Meibomite: eyelids look inflamed, red and thickened, there are few scales on the eyelashes |
Basal cell carcinomas (BCCs) account for more than 90% of malignant eyelid tumors. They usually affect the sun-exposed lower eyelids and the medial corner of the eye. Classic BCC is a nodule with an uneven surface, telangioecasias and a rounded edge, with a central ulceration.
Treatment is complete removal of the tumor, confirmed histologically. Radiotherapy and cryotherapy remain alternative methods, but the high relapse rate limits their use.
Squamous cell carcinoma (SCC) is much less common than BCC but is significantly more malignant. It can occur spontaneously or in areas of sunburn and radiation keratosis. The tumor is amenable to cryotherapy and radiation, but the method of choice remains surgery with histological control of the tissue around the tumor. In case of recurrent PCI, more traumatic operations are required - with complete removal of the orbital contents.
Sebaceous adenocarcinoma is very rare and requires careful diagnosis. This is an extremely malignant tumor, usually fatal, arising from the meibomian glands on the cartilage of the eyelid or from the glands of Zeiss.
These tumors can “masquerade” as benign conditions, such as chronic blepharitis and chalazion. Any atypical manifestations or resistance to treatment should suggest a malignant process. Diagnosis is usually made by biopsy of a full-thickness section of the eyelid.
References
1.
Woog JJ, Jakobiec FA Principles and Practice of ophthalmology - clinical practice.
WB Saunders Co. Vol. 3 8: 1685-1859. 2.
Arffa, RC Grayson's diseases of the cornea.
Mosby Year Book Inc, 1991 13: 295-309. 3.
Tasman W., Jaeger E. A. Duanes' clinical ophthalmology. Vol. 6 118, 123
Note!
- Anterior blepharitis can be controlled with eyelid hygiene—cleaning the eyelid margins with diluted baby shampoo or sodium bicarbonate solution—and applying topical antibiotics to the eyelid margin after cleaning
- For posterior blepharitis, hot compresses and eyelid massage are used (to facilitate the passage of stagnant meibomian gland secretions) and systemic antibiotics are prescribed, such as tetracycline, doxycycline and erythromycin
- With entropion, a rolled-up eyelid can damage the cornea, causing ulceration and secondary infection. Treatment is usually surgical, aimed at restoring elasticity and reducing laxity of the eyelid.
- The first step in treating eyelid tumors is to determine their malignancy. Signs of malignancy: ulceration, induration, uneven surface, painless local telagioectasia and granular margins
Milia: a small educational program
Milia look like small formations rising above the surface of the skin, which are characterized by a white color and clear boundaries. They are easily identified visually, especially noticeable on dark skin. If there are many such formations and they are located close to each other, then the skin in these places becomes rough and grooves appear on it.
Sometimes such a cosmetic defect disappears on its own after a few weeks or months, but often it is corrected by cosmetologists.
What is millet
Prosyanka is the second name for milia, “folk”, more understandable to every person. They are small “grains” (hence the popular name) with yellowish contents. Their size does not exceed 3 mm, but more often ranges from 0.5-2 mm. They do not pose any threat to human health or life; doctors classify them as cosmetic defects.
Most often, millet is localized on the eyelids, temples, nose and area around the eyes. They can be single or form large groups.
Structure of milia on the face
The structure of milimums is fundamentally different from that inherent in comedones - it is a cyst capsule, the bottom and walls of which are lined with epithelial cells. Sometimes the secretion of the sebaceous glands is mixed into this mass, but in very small quantities - the millet does not have the effect of squeezing out and removing the contents. Milia on the face are located separately from the sebaceous, sweat glands and hair follicles.
It is extremely rare that when milia are pierced, a drop of a whitish, thick and viscous substance comes out. Since they are located in the superficial layer of the dermis, they can only be removed by specific cosmetic procedures.
Acne characteristics
The description of the “pimples” in question boils down to the following:
- formations of small sizes;
- extremely rarely become inflamed;
- protrude above the surface of the skin.
Milia remain in their original size for a long time; they cannot be squeezed out or disguised with foundation - the protruding tubercle will still be noticeable to others.
Why did they appear on the face of a newborn?
Milia often appear on the face of a newborn, and the reason for this is the transitional period of adaptation of the baby’s body to the environment against the background of imperfections in the immune system and metabolism. The baby's millet disappears on its own; no therapeutic measures are taken.
Most often, milia in newborns are localized on the forehead, in the area of the bridge of the nose and “wings” of the nose, around the mouth. They are almost never isolated.
Reasons for the appearance of milia on the face in adults, on the back
Reasons for the formation of milia on the face in adults:
- hormonal imbalance - occurs with diseases of the endocrine system, during menopause, adolescence, with pathologies of the adrenal glands or thyroid gland;
- problems in metabolic processes - they proceed too slowly;
- lack of vitamin A - can occur against the background of progressive diseases of the digestive system, with improper/poor nutrition;
- hereditary predisposition.
In fact, the listed conditions cannot be called the true causes of the appearance of millet in an adult, because they have not been fully elucidated. But these are provoking factors, you can add to them excessive tanning, constant exposure to direct rays of the sun (they serve as a “push” for the formation of milia on the back), and the use of low-quality or inappropriate cosmetics for the type of dermis in facial skin care.
Why can they be found on the labia?
Milia form on the labia only due to hormonal imbalance. The risk group among women is pregnant women in menopause. Milia in the intimate area can be single or form in groups. They are not dangerous, rarely open, and therefore the risk of infection is almost zero.
Symptoms of presence on the eyelid, under the eyes, on the forehead, lips
Diagnosis of milia on the eyelid, under the eyes, on the forehead and lips begins with an examination of the rash by a dermatologist or cosmetologist; the main symptoms of the formations are:
- the size of the “pimple” is small;
- there is no redness, swelling or other signs of inflammation around it;
- palpation reveals a dense structure of the millet.
Milia are painless, slightly raised above the general surface of the skin, and do not lend themselves to mechanical extrusion.
Since it is necessary to differentiate harmless milia from fibroma, syringoma, trichodiscoma and xanthelasma, the doctor will extract the contents of the formation and send it for histological examination to the laboratory.
Barley
This is an acute disease that involves the development of inflammation in the hair follicles near the eyelashes and the sebaceous glands in the corners of the eyelids. The main cause of barley is an infection, most often caused by Staphylococcus aureus. Pathology can be caused by:
- sore throat;
- ARVI;
- weakened immunity due to taking hormonal or antibacterial drugs;
- hypothermia;
- improper hygiene;
- diabetes mellitus
Symptoms of stye:
- first, a swelling appears on the eyelid, it grows quickly and causes pain;
- then a dense pimple forms in the inflamed area;
- then the pimple on the eyelid bursts, purulent contents come out of it, and the person feels the pain subside.
Inflammation does not allow the glands located in the eye to function normally: protection from UV radiation, high and low temperatures, and dry air is impaired. The patient may experience fever, headache, and weakness.
The doctor most often prescribes local therapy (antiseptic ointments, antibacterial drops), less often - systemic antibiotics. It is impossible to pierce the stye, as it can cause blood poisoning and the development of an infection in the eye.
Milia on the face: how to get rid of milia?
It should be noted that the only way to treat milia on the face is to go to a beauty salon; as part of this, effective measures are taken to remove nodules on the skin. Moreover, consultation with a professional cosmetologist is necessary, since most often no treatment will be required, since milia themselves disappear over time. As for therapeutic treatment, it can be performed by several methods, which are described in more detail below.
https://youtube.com/watch?v=nkQKP5KaX8s
Getting rid of milia with laser
The most effective way to remove milia on the face and eyelids is laser coagulation of the skin. As a rule, a specific approach is used in case of multiple appearance of dermal cysts and during their group presence on the face. To implement a certain cosmetological process, a carbon dioxide laser or CO2 laser is used. In some cases, another liquefied gas may be used to achieve the desired effect, for example:
- nitrogen;
- helium;
- hydrogen;
- xenon.
With their help, you can get rid of emerging formations on the skin as efficiently and safely as possible, since this approach allows you to remove the affected areas layer by layer without damaging the skin. The laser beam can provide the most positive cosmetic effect, and due to the bactericidal properties of the beam, infection is not allowed. With this effect there is no bleeding, since coagulation of blood vessels is performed.
Curettage or mechanical removal
The main method of mechanically getting rid of white nodules on the skin of the face is curettage.
As part of this approach, the cosmetologist pierces the cyst vesicle using a special instrument and squeezes out the capsule. The procedure itself is performed using a special spoon called a curette. The spoon is a steel knitting needle with a loop at the end where the knot is placed, then the contents of the formation are removed. This method is most relevant during single lesions, which are not difficult to squeeze out mechanically. This is not the best method, since after the procedure the cyst may reappear, but at the same time, curettage is considered one of the most frequently performed and popular cosmetic procedures.
Chalazion
This is a chronic disease involving inflammation of the edge of the eyelid. The reason for the formation of a pimple of this type on the eyelid may be a blockage of the meibomian gland, which makes it difficult for the secretion produced by it to escape.
A chalazion is a dense pimple on the eyelid that causes pain. The formation is light red in color with a gray center. It can fester and lead to limited activity of the eye. The patient feels pain when blinking and has difficulty looking at bright colors. The doctor may prescribe hormonal medications and ointments. If suppuration occurs, surgical intervention may be necessary.
Prevention
If white spots form on your face from time to time, then use the following recommendations to prevent their reoccurrence:
- Exfoliating treatments. We are talking about the use of scrubs that help activate skin regeneration processes and open clogged pores. It is not recommended to use scrubs more than 2 times a week for people with oily and normal skin types. And if your skin type is dry, then it is characterized by increased sensitivity - it is enough to carry out an exfoliating procedure once a week.
- Proper nutrition. You shouldn’t torture yourself with diets, but you need to review your own menu. The diet should include cereals, vegetables, fruits and herbs - these products contain a large amount of fiber, which has a beneficial effect on intestinal function. It is necessary to limit the consumption of carbohydrate foods - baked goods, sweets, and also too fatty foods.
- Use of creams. This is where you need to be extremely careful - cosmetologists call choosing a truly suitable cream a science. You need to focus on the following indicators: the cream should not leave a greasy film on the face, cause irritation or create an impenetrable film on the skin surface.
- Application of tonics. This is not prohibited, but even recommended - tonics moisturize the skin, help close pores, and nourish the epidermis.
- Regular cleansing. You cannot ignore the recommendation of cosmetologists and dermatologists regarding cleansing your face - you need to do this 2 times a day using specific products. Various gels, milks, soaps and lotions should be selected only individually and taking into account your skin type.
- Boosting immunity. It is worth thinking about lifestyle modifications and taking immunomodulators. With a strong immune system, pathogenic microflora are simply not able to multiply and spread - there will definitely be no grass on the face.
Before you settle on a specific method for eliminating milia, try to find out the true cause of their appearance. It is possible that in this way the body gives a signal about the onset of a serious illness.
More about the disease
Millet is a whitehead that appears on any part of the body. Cannot be squeezed out or removed. Have a closed form. It is a cyst located on the skin that is white in color. It is not dangerous until it grows. Starting to increase in size, it brings discomfort. Often occurs on the face and eyelids. There is a logical question: how to get rid of it if there is grass on the eyelid.
There are many medications available to help cure any disease. Millet can be removed with the help of preventive measures and the use of medications. Some use traditional medicine. It is worth remembering that for a quick, accurate effect, you should not go through treatment methods. In this case, prevention and medication will be the best way to eliminate the unpleasant formation in the facial area.
Causes
There are several reasons for the formation of whiteheads on the eyelid:
- hormonal disbalance;
- dysfunction of the digestive system;
- dysfunction of internal secretion organs;
- skin type.
Hormones are an important part of any human body. Hormonal levels indicate good health. An increased or decreased amount causes illness and dysfunction in the body. Having done the tests, the results can tell you a lot. It is possible to identify a premonitory disease. Hormonal disruptions often occur in adolescents during puberty and pregnant women. In both cases, the body is preparing for restructuring. In the case of adolescence, a person matures, preparing physically and mentally for adult life and the birth of children. To fully mature, the body undergoes a certain transformation. The appearance of formations on the face is not a surprising phenomenon. Do not touch the bulges on the eyelid; wait until puberty is over; the pimple may go away on its own
The digestive system, the smooth functioning of the gastrointestinal tract, is a clear sign of good health. Poor nutrition can bear fruit at the most unpredictable moments in life. The worst thing is that the disease progresses without symptoms or obvious signs. The disease may be noticeable when it appears on the face. Various rashes, jaundice, wen, boils are not a complete list of possible diseases that arise when the functions of the gastrointestinal tract are disrupted. By eliminating the problem with the stomach, you will remove formations on the face. Proper nutrition, a healthy lifestyle, and regular intake of vitamins will help. Maintaining natural microflora is the key to health.
Formations can be provoked by the pancreas and thyroid gland. Organs that control the general condition of the body and the production of hormones. Dysfunction of these organs provokes many diseases associated with the production of hormones. They are stabilizers. It is almost impossible to feel a problem with the above organs. Appears only in advanced cases. Symptoms appear only as the disease progresses. It begins to appear on the face and body.
Much depends on your skin type. Having a dry type of dermis is unlikely to occur. It occurs in people with oily skin. There is a large production of sebum. The bulges sometimes have a yellowish or white color. Explained by the presence of sebum. It is more often observed in women than in men. This phenomenon is not observed in the stronger sex. The weaker sex suffers from millet at the ages of forty to sixty years. In adolescence, acne goes away quickly, leaving no memories. It is worth remembering that white formations do not pose any danger.
The phenomenon is cosmetic in nature. It is removed only at the request of the patient. A dermatologist will help you eliminate it. No special treatment is required. There is no need to be afraid. There is no need to be nervous or worry when you see white pimples. Correct your skin type with washes and special products. You can replace washing with warm, hot water with cold. Dries the epidermis, stops sebum production. It’s worth remembering that you shouldn’t overdo it either. Drying out the dermis can lead to the appearance of dry spots and flaking of the skin. Alternate the washing temperature. By following the rules, you can restore your dermis to the desired state and prevent the appearance of white pimples.
Diagnostics
Determining the type of appearance is quite easy. There is no need to take a large number of tests, take many x-rays, or undergo numerous examinations. It is enough to take a mirror with magnification and carefully examine the white pimples. To be more convincing, you can contact a qualified specialist. The doctor will be able to confirm his own diagnosis.
Whiteheads differ from regular pimples in the absence of a self-removal method. Being deep under the skin, it is impossible to squeeze it out on your own. Has a small size. The base is made of ordinary epidermis. The top has a white, yellowish color. A small white pimple does not cause pain or particular discomfort. It may interfere, appearing on the eyelids and nose. The resulting millet on the eyelids is more noticeable. Feels it the most. When blinking, a person will feel the presence of a foreign body.
Traditional methods
According to reviews, eliminating millet using folk methods is painless, but very time-consuming. Until the rash gets rid of completely, you should be patient and regularly carry out the recommended procedures. However, there are also advantages to folk remedies for milia:
- absence of injuries and scars;
- no hardware irradiation;
- availability;
- Possibility of use at home;
As a rule, all folk recipes are based on mechanical cleansing of the skin from dead cells. The use of natural abrasives ensures the softness of the procedure and their positive effect on the condition of the skin as a whole. When using peels, avoid rubbing the skin excessively. All movements should be light and gentle. Otherwise, the number of milia will not decrease, but increase. Recommended procedures are described below.
The general scheme of action of traditional methods is to gradually eliminate the milia coating, after which it can easily be removed from the skin on its own. In addition, most natural remedies heal the epidermis, preventing new rashes.
Soda
- Baby soap is foamed on the palms.
- Pour a tablespoon of soda onto the surface of the foam.
- Use gentle movements to treat facial skin.
- The composition is washed off immediately and the usual care is applied.
Paraffin
- Paraffin (70 g) is melted in a water bath.
- The skin is wiped with alcohol.
- Paraffin is applied to the entire face in several layers. A new layer is applied only after the previous one has hardened.
- The mask is removed from the face after the paraffin has completely cooled.
Salt
- Those with sensitive and dry skin conditions mix fine-crystalline sea salt with olive oil. Those with oily skin combine salt with sour cream.
- The thick mass is collected with a cotton pad.
- They also gently massage areas where white dots accumulate.
- After the procedure, the composition is washed off and a moisturizer is applied to the skin.
Pumpkin
- Grind raw pumpkin on a fine grater.
- The sour cream puree is diluted to a homogeneous but thick consistency.
- The product is applied to the entire face for a quarter of an hour.
Kalina
- Frozen viburnum berries are ground through a sieve or in a blender.
- Excess juice is squeezed out of the puree.
- To form a viscous mass, add a little rice or oatmeal to the viburnum. Apply the thick mixture to the rash for a third of an hour.
- After the specified time, wash off with warm water.
Yeast
- A dessert spoon of raw yeast is mixed with peroxide, lemon juice and liquid honey, taken one tablespoon at a time.
- The thoroughly mixed substance is left warm for ten minutes.
- Apply the product to the skin and leave for 20 minutes.
- After drying, wash off with warm water, without a sponge.
Recipes using fruits and various juices work like acid peeling
In this case, it is important to follow the recipe for preparing the cleaning composition and use it regularly every day.
To eliminate millet at home, it is forbidden to use iodine, pure peroxide, or 96% alcohol. This will only worsen the situation, provoking the activation of the protective functions of the skin and increased division of its cells.
Millet on the face is a cosmetic defect for which it is better to seek the help of a specialist. Especially if the formations are multiple or have an impressive depth
To quickly and effectively solve the problem, it is important to determine the exact structure and nature of the rash and make sure that it is definitely milia
Treatment prognosis and possible complications
Milia are not dangerous to life or health. This is a cosmetic defect that signals problems with sebaceous regulation. Folk home methods do not guarantee the disappearance of grass under the eyes; they are more helpful in prevention or recovery after hardware removal.
Prevention:
- use of non-comedogenic skincare products;
- regular skin cleansing morning and evening;
- acid peelings in cosmetic clinics and salons;
- vacuum, ultrasonic, mechanical cleaning;
- quitting smoking, alcohol;
- minimizing oily foundation, BB, CC creams;
- laser resurfacing;
- diet with restrictions on fried, sweet, fatty, smoked foods;
- use of cosmetics with sun protection factors;
- treatment of diseases that cause milia.
Laser, electric and radio wave coagulation do not guarantee a lasting effect the first time. If the formation has not been completely cleared, it may quickly reappear. You cannot remove more than ten manifestations of millet in one procedure. This unnecessarily traumatizes the skin, which can disrupt the functioning of the sebaceous glands.
Complications occur rarely and manifest themselves as an inflammatory reaction, ulcers, acne near the eyes.
Milium is a common skin problem. It is not dangerous; removal is indicated for aesthetic discomfort. Do not try to eliminate the formations yourself - you need to consult a doctor so as not to cause undesirable consequences.
The article has been reviewed by the site editors
HOW THE PROCEDURE IS CARRIED OUT
Laser removal of milia is a simple and quick procedure. Before performing it, the patient is recommended to have a preliminary consultation with a specialist, during which an examination is carried out, possible contraindications to the use of the method are clarified, and the optimal laser wavelength is selected.
Directly to remove the grass, the patient is placed on the couch. Aseptic treatment of the skin is carried out. The doctor and client then put on special safety glasses. A specialist uses a laser device to irradiate the pathological focus and remove the skin defect. At the end of the procedure, the skin is again treated with an antiseptic.
The duration of the manipulation is 7-10 minutes. It may increase slightly if it is necessary to get rid of a large number of grasses at the same time. One session is enough to eliminate white pimples.
Wen, millet: what could be the danger?
- Milium, wen, and millet can appear on both the body of an adult and a child. When education appears, your well-being will not change in any way. But still, you shouldn’t put off visiting a dermatologist. Unlike blackheads, white wen cannot and cannot be squeezed out on your own at home. And if such a thought occurs to you, then immediately put it aside. Because this can be dangerous due to infection and inflammation!
- And since the cause may not be a cosmetic problem, but a metabolic disorder, it is worth understanding the malfunctions of the body in order to prevent further recurrence of the occurrence of wen throughout the body.
- Lipoma most often affects the outer layers of the skin. But there are cases when a wen also appears on internal organs, which also have a fatty layer. If there is not one lipoma on the body, but several formations at once, this condition is called lipomatosis.
- Very rarely, but there are still cases of degeneration of this benign formation into a malignant one - liposarcoma. It is impossible to establish this diagnosis at home! The main signal is the dimensions and the speed of increase in size
. Therefore, it is better to consult a doctor immediately when a wen is discovered. In case of suspicion, the doctor will prescribe a puncture, and based on the results of the analysis, treatment.
This is already a pathological degeneration of lipoma
CONTRAINDICATIONS
LASER REMOVAL OF MILLS IS NOT CARRIED OUT IF THE CLIENT HAS THE FOLLOWING CONDITIONS:
- Benign and malignant tumors of any location
- Diabetes
- Pregnancy
- Hypertonic disease
- Hormonal disorders, endocrine diseases
- Exacerbation of infections, including herpes
- Chronic pathologies in the stage of decompensation
- Mental disorders