November 3, 2020
When the head of the male organ becomes red and swollen, this is an inflammation called balanitis. When the foreskin is also involved in the process, the disease is called balanoposthitis. Redness is accompanied by itching, burning, pain when urinating, and sometimes mucus leaking from the urethra. The disease cannot be neglected; it can spread throughout the genitourinary system, provoke phimosis and lead to necrosis of the head.
Contact dermatitis of the penis
Contact dermatitis is a dermatitis that occurs as a result of contact with a specific substance.
It may itself be irritating or cause hypersensitivity reactions.
Based on the mechanism of development of inflammation, contact dermatitis is distinguished:
- simple - occurs when an irritating substance comes into contact with the skin (in fact, this is a consequence of a chemical burn)
- allergic - develops when a chemical compound comes into contact with the skin of the penis, causing hypersensitivity reactions
Causes and symptoms of contact dermatitis of the penis
Simple contact dermatitis is rare.
This is due to the fact that it occurs as a result of contact with industrial liquids, household chemicals and other substances with which the male penis comes into contact extremely rarely.
Most of the work is done by hand.
Therefore, it is on the hands that this type of dermatitis most often develops.
However, there are sometimes cases where similar phenomena are observed on the penis.
This is possible if a man:
- spilled a liquid that has irritating properties on yourself
- used a liquid hazardous to the skin for self-medication (when trying to remove warts, to fight pubic lice, to disinfect a scratch, etc.)
More often, contact dermatitis of the penis develops in people who practice self-medication.
Including the use of folk remedies that are mistakenly considered safe only because of their natural origin.
Also, a considerable amount of industrial substances can cause a chemical burn.
Among them:
- phenol
- paint solvents
- sodium hydroxide
- acids
- detergents
- kerosene
With a single contact of the skin of the penis with an irritating substance, dermatitis does not last long.
Symptoms usually go away on their own after a few days.
With extensive skin burns, they persist for several weeks.
Repeated contacts lead to a long course of the disease.
It can last for months and even years.
However, when contact dermatitis is localized specifically on the penis, such cases are very rare.
This is due to the fact that even the most avid lover of traditional medicine understands after some time that applying acids, kerosene or herbal tincture to the penis leads to inflammation of the skin.
Therefore, he stops trying to self-medicate.
Simple contact dermatitis can occur in acute, subacute and chronic forms.
In the acute form of the disease, red plaques appear on the skin of the penis.
They have clear boundaries.
Upon examination, local tissue swelling is detected.
There are many small vesicles on the surface of the plaques.
They are small bubbles with transparent contents.
There is no umbilical depression in the center.
Point erosions appear.
A clear liquid is released from them.
After a few days, crusts form at the site of erosion.
If acute dermatitis of the penis develops as a result of one contact with an irritating substance, then repeated contacts with a less aggressive chemical compound leads to subacute dermatitis.
It is characterized by peeling on the surface of the plaques.
There are no vesicles.
But often many small papules appear.
These are cavityless elements of red color, slightly rising above the surface of the skin.
Chronic contact dermatitis on the penis is very rare.
It develops only in people who persist in self-medication.
And also among those who perceive the symptoms that arise not as a consequence of inadequate therapy, but as an exacerbation of a disease requiring further treatment.
It is often not so easy to determine that skin lesions that occur are related to a certain substance.
Because after the first application there is no reaction.
Subsequently, after systematic use, it gradually develops, the intensity of changes increases.
However, after each application there is no sudden deterioration.
Therefore, patients do not always understand that the substance they are using is toxic to the skin.
With constant application of an irritating chemical compound to the head of the penis, foci of lichenification occur.
The epidermis in the affected area thickens.
The skin pattern intensifies.
Transverse stripes or diamonds are formed.
May be present:
- skin redness
- small papules, usually flat
- scratching, as patients often suffer from itchy skin
Over time, the skin becomes pigmented.
It becomes darker than in adjacent areas.
Treatment of dermatitis in the groin
One of the most unpleasant types of skin inflammation is dermatitis on the genitals. It causes itching, soreness and discomfort. Since the skin in the genital area is especially thin and delicate, the manifestations of the disease cannot be ignored.
Inguinal dermatitis: symptoms
Manifestations of the disease depend on its stage.
- Easy. The skin on the genitals becomes red and swollen, and the patient feels discomfort.
- Average. Skin rashes appear, itching and pain are felt.
- Heavy. The bubbles merge into a single conglomerate, and erosion of the affected areas begins. An unpleasant odor, general weakness, and fever may occur.
If dermatitis is not treated, consequences such as, for example, deformation of the penis are possible. Eczema may also occur, which will recur in the future.
Causes and types of dermatitis in the groin
Depending on the etiology, there are several types of skin inflammation in the genital area.
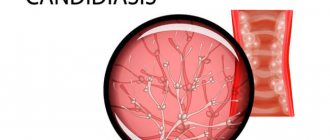
- Candida. The causative agent of the disease is fungi. The cause may be diabetes mellitus, long-term use of antibiotics and oral contraceptives. The rash on the genitals looks like nodules or scales.
- Dermatophytic. It also has a fungal origin, but is transmitted through sexual contact, using other people's towels, and so on. It can begin due to poor personal hygiene or wearing stale underwear.
- Seborrheic. This type of inguinal dermatitis occurs in the area of the labia, penis, and anus as a result of excessive activity of the sebaceous glands. Its characteristic feature is red spots with scales.
- Erythrasma. The causative agents of the disease are bacteria, so treatment requires the use of antibiotics. Red spots and a scaly rash form in the groin area.
- Psoriasis. This type of inguinal dermatitis is incurable; its course consists of stages of remission and exacerbation. Medical care in this case comes down to reducing unpleasant symptoms and discomfort.
The causes of dermatitis on the genitals can be existing diseases - genital herpes, papillomatosis, syphilis, thrush, diabetes, gastrointestinal diseases. Often, skin inflammation occurs due to factors such as:
- heavy sweating;
- wearing synthetic underwear;
- obesity;
- allergic reactions;
- taking medications;
- neglect of hygiene standards.
How is dermatitis in the groin treated?
Dermatologists at the Private Practice clinic prescribe therapy depending on the causes of the disease, its form and severity. If inguinal dermatitis is a consequence of other diseases, treatment is carried out in combination.
In each individual case, our specialists select certain medications - antibacterial, antifungal, antihistamines, prescribe anti-inflammatory and immunomodulating agents. Ointments, lotions, and medicinal baths give a good effect. We provide recommendations for lifestyle adjustments: in particular, it is important to maintain personal hygiene and adhere to dietary rules.
Diagnosis of contact dermatitis of the penis
Contact dermatitis can be defined clinically based on symptoms.
Sometimes there is a need for pathomorphological examination of the skin.
Then a biopsy is taken.
Of no small importance in diagnosis is the differentiation of simple contact dermatitis from allergic one.
The differences are as follows:
- with simple acute contact dermatitis, papules do not appear on the penis, but with allergic dermatitis, they form quite often
- against the background of chronic simple contact dermatitis, cracks form on the penis, but this does not happen with allergic reactions
- with simple dermatitis, the affected area is limited strictly to the area affected by the toxic substance, while with allergic inflammation it spreads to adjacent areas of the skin
- with allergic dermatitis of the penis, general symptoms are possible, but with simple dermatitis there are none
- the severity of the symptoms of simple dermatitis depends on the concentration of the irritating substance applied to the skin of the penis, while with the allergic nature of the inflammation, the amount of the allergen does not matter
If a patient is allergic to a certain substance, then after sensitization has occurred, each subsequent contact with the allergen will be accompanied by symptoms of dermatitis.
Whereas with chronic simple dermatitis of the penis, the reaction does not develop immediately, but after a certain time after regular application of a toxic substance to the penis.
What are the causes of lichen sclerosus?
As mentioned above, the exact cause of LS is not yet known. However, a number of factors have been studied that may be involved in the development of the disease:
- Genetic factors. Familial cases of LS in twins, sisters, mother and daughter have been described. According to research, the development of LS and its severity were associated with the inheritance of a number of genes.
- Autoimmune factors. Some studies have indicated an association between LS and autoimmune diseases (vitiligo, alopecia, thyroid disease, pernicious anemia, diabetes mellitus, cicatricial pemphigoid, polymyalgia rheumatica, psoriasis, primary biliary cirrhosis, systemic lupus erythematosus. However, some manifestations of tissue damage with LS is similar to the characteristic tissue damage associated with autoimmune connective tissue diseases.
- Infectious factors. Some infections, primarily spirochetes, had a probabilistic relationship with the development of LS. Lyme disease is caused by spirochetes of the genus Borellia. Acrodermatitis, which develops in Lyme disease, has similar manifestations to LS. However, attempts to detect the causative agent of Lyme disease (Borellia burdoferi) in patients with LS have not yet yielded convincing results. Viruses have also been studied as possible causes of LS. Thus, human papillomavirus was often detected in the tissues of the foreskin in patients with LS who underwent circumcision.
- Local factors. Sometimes the development of LS is associated with local skin damage. The trigger for the development of LS can be mechanical trauma in the area of old scars, radiation exposure of the skin during radiation therapy, abrasion of the skin, chronic irritation of the skin with urine in patients with diabetes.
- Hormonal factors. Some forms of disturbances in the uptake of male sex hormones into tissues predisposed to the development of LS. Which, in turn, historically led to attempts to treat LS with creams containing the male sex hormone testosterone. Unfortunately, the use of such creams did not produce any noticeable results.
Treatment of contact dermatitis of the penis
The most important thing is to find out the irritant and eliminate it.
Acute simple contact dermatitis of the penis does not require treatment if the reaction occurs after a single contact with the substance.
It is enough not to repeat its application to the penis, and the symptoms will go away over time.
If the clinical manifestations are severe, the help of a doctor may be required.
When large bubbles form, they are punctured.
But the lid of the bubble is not removed.
Subsequently, bandages moistened with antiseptics are used to avoid infection.
To reduce symptoms, weak topical corticosteroids may be used.
In severe cases, systemic glucocorticoid therapy is used.
Allergic dermatitis on the penis
The disease develops as a delayed allergic reaction.
In childhood, this type of dermatitis practically does not occur.
But in adult men this is a very common phenomenon.
Allergic dermatitis is a classic delayed-type reaction mediated by T lymphocytes.
After the first contact, no changes are observed on the skin of the penis.
Because it takes time for sensitization to occur (the body produces antibodies to the allergen).
How long it takes depends on how strong the allergen gets on the skin of the penis.
If it is weak, sensitization may occur only after several months or even years.
Strong allergens cause rapid sensitization, so with repeated contact with them, signs of dermatitis on the penis may appear within a few days or weeks.
The main subjective symptom is itching.
Less commonly observed general symptoms:
- hyperthermia
- weakness
- headache
- chills
It is important for the doctor to find out what substance the reaction occurred to in order to prevent further contact with it.
Common causes of contact dermatitis include:
- antibiotic neomycin
- paraphenylenediamine, which may be contained in fabric dyes (if it is present in underwear, then dermatitis will occur not only on the penis)
- creams with sulfonamides
- procaine, benzocaine (local anesthetics)
- formaldehyde, mercury - can be part of antiseptics
Allergens are often included in lubricants, spermicides, cosmetic creams and preparations.
If the drugs are not used by a man, it is worth checking whether the woman is using them intravaginally.
If the patient's partner uses them, it is possible that it is to the components of these drugs that a reaction occurs after sexual intercourse.
Some men are allergic to latex.
This is a natural substance from which condoms are made.
What treatments are there for lichen sclerosus?
The extent of treatment depends on the extent of the spread of the LS process.
- Stage I SL. Only the foreskin is involved in the process. Uncircumcised men have a whitish sclerotic ring on the foreskin. There are no lesions on the skin of the head of the penis or the external opening of the urethra. Treatment: performing the operation of circumcision of the foreskin (circumcision) and further observation.
- Stage II SL. At this stage, the foreskin is affected and damage to the skin of the glans penis appears in the form of whitish sclerotic “bridges” of the transition of the LS process from the foreskin to the coronal sulcus and the skin of the glans penis. This stage of LS can often be found in circumcised men. At this stage, narrowing (stricture) of the external opening of the urethra and difficulty urinating may appear. Treatment: surgical removal of the affected tissue, if necessary, surgery to expand the external opening of the urethra (meatotomy), long-term local treatment with glucocorticoid anti-inflammatory cream Dermovate 0.05% (clobetasol) or Diprospan, Akriderm, Celestoderm 0.1% (betamethasone) 2 times a day daily in courses of 2 - 3 months.
- Stage III SL. The process involves the foreskin, the head of the penis, and the external opening of the urethra. The aesthetic appearance of the penis is significantly changed. This stage can often be observed in patients previously treated for LS, who have already undergone plastic surgery of narrowings (strictures) of both the external opening and the urethra itself. Urethrography often shows extensive narrowing (stricture) of the urethra. Treatment: complex plastic surgery to eliminate strictures of the urethra, wide excision of scar tissue, long-term local treatment with glucocorticoid anti-inflammatory cream.
- Stage IV. Penile tissue lesions may resemble precancerous conditions and penile cancer. Treatment involves surgical excision of scar tissue. However, in preparation for treatment, as a rule, a biopsy of tissue of the penis and urethra is required to exclude malignant degeneration (cancer).
It is important to note that circumcision (circular excision of the foreskin in LS has its own characteristics. The main task of circumcision in LS is the complete excision of the affected tissue. However, too much of the foreskin should not be removed, as it may be needed in the future for plastic surgery reconstruction of narrowings (strictures) of the urethra (primarily the scaphoid fossa), which can be caused by LS. The following figures show the stages of treatment of LS of the penis stage I-II (the appearance before surgery is shown in Fig. 3).
Rice. 5. Circumcision for LS using the double-incision technique. The skin incision is marked in such a way as to excise the affected part of the foreskin of the penis, which is clearly visible.
Rice. 6. Condition of the penis after surgery. The affected skin is excised, but it is sufficient for possible subsequent reconstructive operations.
Symptoms of allergic dermatitis of the penis
Clinical manifestations are generally the same as for simple contact dermatitis.
However, there are some differences.
In acute allergic dermatitis, the skin rash goes through the following stages:
- redness
- formation of papules (a characteristic difference from simple contact dermatitis of the penis)
- appearance of bubbles
- after opening them, erosions (superficial skin defects) form in their place.
- crusts form after drying
- Peeling is observed during healing
Chronic allergic dermatitis occurs in the same way as simple dermatitis.
The differences are as follows:
- no cracks appear
- symptoms worsen or appear almost immediately after contact with the allergen (if by this time the immune system has already become “acquainted” with this substance)
Against the background of existing allergic dermatitis, contact urticaria may occur.
It is characterized by the appearance of blisters.
Diagnosis of allergic dermatitis of the penis
Typically, a doctor diagnoses allergic dermatitis of the penis based on symptoms and medical history (contact with certain substances).
They also help him distinguish this type of skin inflammation from other types of the disease:
- blood test for allergies
- pathological examination of the skin
- tests with a potential allergen
The doctor asks the patient what exactly he has been putting on his penis lately.
Applying this substance to any area of the skin will cause the same reaction.
This test is called a patch test.
It can only be carried out on those substances that are used by the patient.
In addition, there are kits of allergens that can be tested for in the clinic.
Application or other skin tests are prescribed no earlier than 2 weeks after the elimination of the main symptoms of dermatitis.
Actions for redness of the glans in men: how to treat
The most dangerous tactic is to try to use any ointments or other medications yourself before consulting a doctor. In 90% of cases, this does not help, distorts test results, and makes them false negative. Until the causes are clarified and cured, you need to stop having sex.
When inflammation on the head of the penis does not go away after careful hygiene, changing linen or detergents, contact our clinic. At the Clinic Dr. AkNer you will receive all the necessary tests and expert advice.
Urologist, andrologist Akopyan Nerses Grigorievich.
Back to list of articles
Treatment of allergic dermatitis of the penis
The most important thing is to eliminate the allergen.
As long as contact with him continues, dermatitis on the penis will recur again and again.
And no drugs will help get rid of rashes once and for all.
To eliminate symptoms, ointments with corticosteroids are mainly used.
In severe cases, they are taken orally.
Taking antihistamines and other antiallergic drugs for contact allergic dermatitis of the penis usually has low effectiveness.
Seborrheic dermatitis on the penis
There are quite a few sebaceous glands on the penis.
Therefore, this organ can be affected by seborrheic dermatitis.
It is characterized by redness and peeling of the skin.
This type of dermatitis occurs mainly during puberty or in young men with high testosterone levels.
Seborrheic dermatitis develops against the background of increased sebum secretion.
Risk factors:
- heredity
- young age
- oily skin type
- immunodeficiencies, including HIV infection (with weak immunity, there is excessive growth of microflora that feeds on sebum)
Causes
The cause of inflammation of the head of the penis can be infectious or non-infectious. One of the main non-infectious causes is poor hygiene of the genital organs, as a result of which secretions begin to accumulate under the foreskin, which causes an inflammatory process. Other causes of inflammation of the head of the penis include:
- infectious and inflammatory diseases of the genitourinary system (urethritis, cystitis);
- skin diseases (psoriasis, dermatitis);
- narrowing of the foreskin (phimosis);
- trauma to the skin of the penis (burns, scratches);
- allergic reactions to hygiene products, underwear or contraceptives.
A common cause of inflammation of the glans penis in a child is uncomfortable underwear. It causes discomfort, rubs and injures the skin, causing balanitis in boys.
Symptoms of seborrheic dermatitis on the penis
Often seborrheic dermatitis develops simultaneously in several areas of the body.
The scalp, folds, and face also become inflamed.
On the penis, lesions of seborrheic dermatitis look like yellowish crusts.
Plaques often form that mimic psoriasis.
There are also cases when psoriasis is combined with seborrheic dermatitis.
There is even a separate medical term for this condition: sebopsoriasis.
Diagnosis of seborrheic dermatitis on the penis
In most cases, a clinical picture is sufficient to establish a diagnosis.
Not only the appearance of the skin is taken into account, but also the excess secretion of sebum.
Patients often experience excessive sweating.
In controversial diagnostic cases, the diagnosis can be confirmed using a skin biopsy.
A rash similar to seborrheic dermatitis occurs when:
- zinc deficiency
- vitamin deficiency RR (practically not found in civilized countries, achieved only experimentally)
- Parkinson's disease
Treatment of seborrheic dermatitis on the penis
Most men experience seborrheic dermatitis in one form or another.
And there is nothing wrong with inflammation of the skin of the penis.
In summer there is usually an improvement, in winter the disease can worsen.
The disease is chronic.
Therefore, it requires constant maintenance therapy and certain lifestyle changes.
Many patients benefit from ultraviolet radiation.
For ethical reasons, natural sunbathing is not possible for most patients.
But the problem is solved by a solarium or special ultraviolet lamps.
To reduce sweating, it is advisable to shave the hair in the intimate area.
In severe cases (with severe symptoms), topical corticosteroids can be used.
They help well, but the possibilities of such therapy are limited.
The problem is that the disease is chronic.
But corticosteroids are not suitable for long-term use because they cause skin atrophy.
To suppress lipophilic fungal flora, creams with ketoconazole are used.
For maintenance therapy, exfoliants are used (usually salicylic acid 2%).
Scleroderma is a fairly common chronic skin disease in the practice of a dermatologist. Recently, there has been an increase in the number of patients with this dermatosis, while the number of patients with both plaque and linear forms of the disease, as well as lichen sclerosus, is increasing. However, it is necessary to focus the attention of specialists on the group of patients with rashes on the skin of the penis for a number of reasons. Firstly, the number of such patients has recently increased. Secondly, this contingent has become “younger”. So, previously men aged 40-50 years old came to us, but now this problem also occurs in men 20-30 years old. Thirdly, it is patients with limited scleroderma who complain of unpleasant sensations. Such complaints include difficulty exposing the head of the penis, pain during intercourse, and the appearance of cracks after intercourse. Moreover, all patients who contacted us were sexually active. Fourthly, all patients came to us at the stage of atrophy development, while patients with the plaque form of scleroderma come mainly at the stage of hyperemia and induration. Also noteworthy is the fact that all patients in this group did not immediately turn to a dermatologist, but were treated for some time by other specialists (urologists). In addition, this group of patients is also ignored in the specialized literature. The main attention is paid only to the presence of erectile dysfunction in patients suffering from systemic scleroderma [1-3]. However, other problems of patients with limited scleroderma with rashes on the skin of the penis are not considered in the specialized literature.
Currently, there are two forms of scleroderma: limited, in which the skin is affected, and systemic, in which the pathological process affects the skin and internal organs. In turn, limited scleroderma is divided into plaque form, linear form, and lichen sclerosus. The linear form of scleroderma includes strip-shaped, saber-shaped and ring-shaped forms.
The clinical picture of limited scleroderma is represented on the skin of the penis by a ring-shaped focus of hyperemia, which subsequently becomes denser, and then atrophy develops over time. However, most patients at this stage do not pay attention to the change in skin color in the penis area. Over time, the skin in the area of the lesion acquires a whitish tint, becomes thinner and causes a narrowing in the area of the shaft of the penis or foreskin. When the lesion is localized in the area of the foreskin, the narrowing can cause difficulties in exposing the head of the penis, tears in the skin and cracks in the area of the foreskin, and pain during sexual intercourse. The development of a limited form of scleroderma in the penile area may lead to the need for circumcision.
This disease must be differentiated from keloid-like nevus, penile leukoplakia, linear keloid, stripe-like skin atrophy and penile candidiasis.
Keloid-like nevus is characterized by the appearance in the first weeks of life, the absence of dynamics of the process and atrophy.
Leukoplakia of the penis is characterized by a delicate clouding of the mucous membrane or skin, reminiscent of a grayish film that does not come off when scraped. Subsequently, the lesion begins to rise above the unchanged skin, its surface is uneven, there may be outgrowths and foci of keratinization, as well as cracks and ulcerations. However, leukoplakia does not lead to atrophy.
Stripe-like skin atrophy is characterized by symmetrical foci of atrophy in areas of increased skin stretching and has the appearance of narrow stripes of varying lengths located below the level of unchanged skin. At the initial stage, the lesions have a pinkish-bluish color, which changes to whitish over time. The surface of the lesions is smooth and shiny or wrinkled and folded.
Linear keloid is a lesion protruding above the surface of unchanged skin, dense on palpation without atrophy.
Candidiasis is characterized by the formation of a whitish coating and superficial erosions on the glans penis or the inner layer of the foreskin. Patients complain of itching, burning and soreness.
During the period from January to October 2016, 88 patients (65 women and 23 men) suffering from limited scleroderma applied to the Warsaw branch of the Moscow Scientific and Practical Center of Dermatovenereology and Cosmetology of the Moscow Department of Health. Of the 23 men, 13 patients were diagnosed with limited scleroderma, a plaque form on the skin of the trunk and limbs, 10 patients had a ring-shaped form of limited scleroderma in the penile area, and in 1 patient the focus of limited scleroderma was located on the skin of the scrotum with transition to the shaft of the penis. Thus, patients with rashes on the skin of the penis accounted for 43% of all male patients suffering from limited scleroderma who contacted our branch during the described period. Patients paid attention to the presence of subjective sensations: difficulty exposing the head of the penis, tears in the skin and cracks in the foreskin, pain during sexual intercourse. Patients were aged from 22 to 58 years (Fig. 1) with disease duration from 3 months to 3 years (Fig. 2).
Rice. 1. Age of patients.
Rice. 2. Duration of the disease.
It is noteworthy that all patients with rashes on the skin of the penis came to us no earlier than 3 months after the appearance of the first symptoms. Moreover, four patients had been treated by urologists for 1-2 months before contacting us.
Objectively, on the skin of the penis there were ring-shaped foci of a pinkish-lilac color with induration (Fig. 3, a) or whitish foci of atrophy (see Fig. 3, b).
Rice. 3. Limited scleroderma on the skin of the penis. a - ring-shaped lesions of a pinkish-lilac color with induration; b — foci of atrophy are whitish in color.
During examination, difficulty was noted in exposing the glans penis; four patients had skin tears in the area of the foreskin. Upon admission, patients were prescribed penicillin drugs, and then prednisilone at a dosage of 30 mg/day with gradual withdrawal of the drug over 1.5-2 months. It should be noted that during the therapy, 9 patients showed improvement, and there was no need for circumcision (Fig. 4, a, b).
Rice. 4. Limited scleroderma on the skin of the penis. a - before treatment; b - after treatment.
Thus, I would like to draw the attention of colleagues to the fact that treatment of this group of patients requires the prescription of glucocorticosteroids due to the fact that the narrowing will intensify, which may lead to the need for circumcision. However, this operation does not always give a positive result, since sclerosis may, in turn, develop at the site of the scar, which will cause further narrowing and dysfunction of the organ. It also seems to us that interdisciplinary cooperation with urologists is necessary in view of the fact that the primary treatment of patients with this disease is often faced by doctors of this related specialty.
Korsunskaya I.M. — https://orcid.org/0000−0002−6583−0318
The authors declare no conflict of interest.