The prevalence of allergic reactions is constantly increasing. More and more people are becoming sensitive to different protein structures. Very often, people are concerned about allergies to insect bites, which can lead to various adverse consequences. The disease, depending on the severity of sensitivity (sensitization), manifests itself both as local symptoms and systemically. Timely intervention allows you to avoid dangerous conditions. Therefore, people with such allergies should always be careful and have emergency supplies with them.
Why does an allergy to stings occur?
An allergic reaction is an increased immune response to foreign proteins that enter the human body. An insect bite can act in several ways:
- Getting poison into the blood;
- Ingestion of toxic saliva;
- Ingestion of particles from wings and other elements of the body (usually not through a bite, but through inhalation).
An allergic reaction to an insect bite depends on the type of organism and the amount of protein that enters the person. Many insects, such as mosquitoes, cause a local inflammatory response in every person. And hymenoptera such as bumblebees, wasps or bees can cause serious swelling and even shock.
Our doctors
Orlova Tatyana Vladimirovna
Doctor - allergist-immunologist, pulmonologist, doctor of the highest category
Experience 38 years
Make an appointment
Shundeva Oksana Veniaminovna
Allergist, doctor of the highest category
Experience 39 years
Make an appointment
Symptoms of an allergy to insect bites
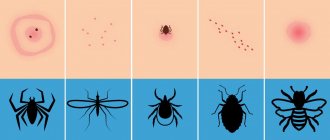
An allergic reaction to insects is an immediate type of reaction, therefore it appears a few minutes after the bite1. Allergy symptoms can be divided into local and systemic. The first ones are less dangerous and do not always require taking medications. A systemic response from the body indicates a severe allergy and can be dangerous.
Local manifestations include:
- Redness at the site of contact with the allergen;
- Swelling of various sizes (from small swelling around the wound to pronounced swelling of a large area);
- Itching in the area of contact with the allergen;
- Burning in the red area.
Local manifestations cause discomfort, but do not pose a danger and do not require emergency injections. However, if there is confirmed sensitization, it is recommended to take an antihistamine to prevent the development of complications. Cetrin is suitable for such purposes.
Systemic reactions are characterized by a violation of the general condition of a person and are an unfavorable sign1. These include:
- The appearance of rashes in the form of papules throughout the body (urticaria);
- Generalized skin itching;
- Dizziness;
- Marked weakness;
- Sudden development of shortness of breath, difficulty breathing;
- The appearance of chest pain.
This clinical picture requires immediate administration of hormonal drugs, otherwise a sharp drop in blood pressure and the development of anaphylactic shock are possible1.
Insect allergy and features of its therapy
Insect allergens can cause the development of sensitization when they enter the body in several ways: with poison - when stung by Hymenoptera (bees, wasps, etc.); with saliva - when bitten by insects of the order Diptera (gnats, mosquitoes, etc.); inhalation and contact methods - with scales, larvae of butterflies, crickets, beetles, etc. [1].
An allergy to insect bites occurs in the form of an immediate or delayed reaction at the site of the bite. Typically, the bite of blood-sucking insects (mosquitoes, mosquitoes, fleas) causes local manifestations in the form of swelling, redness and polymorphic rash (papular, urticarial, hemorrhagic, bullous, necrotic forms) and, extremely rarely, serious allergic reactions. Sometimes an erysipelas-like reaction in the form of acute erythema may occur to midge bites, occurring without an increase in temperature and enlargement of regional lymph nodes. Mosquito saliva allergens can also cause the development of an itchy nodular rash (phlebotoderma). Rare cases of generalized urticarial rash following the bite of even one blood-sucking insect have been described [1, 2].
The greatest danger is the sting of hymenoptera insects, which can cause serious allergic reactions, including anaphylactic shock. The most common allergen that causes the development of allergies is the venom of wasps and bees; bumblebees sting very rarely [2]. Moreover, bumblebees and bees sting only in cases when they are provoked.
Insect allergies are more common in summer and autumn. Insects sting when carrying out gardening work, in picnic areas; they are also attracted to yard garbage cans and compost pits; Don’t forget about wasp nests, which are usually located under eaves and in attics. A single exposure to large doses of insect venom through a sting is comparable to the annual dose of inhaled pollen allergens. The development of such high-dose sensitization explains why the prevalence of atopy among patients with IgE sensitization to poisons is the same as in the normal population [3].
A normal reaction to insect stings usually involves mild localized redness and swelling, while a severe localized reaction typically involves erythema and severe swelling that may progress over 24 to 48 hours and may persist for more than 10 days. At the same time, the patient may experience weakness, malaise, and nausea. In rare cases, infection and inflammation of the subcutaneous fat occur [2].
Local reactions are treated by applying a cold compress to the bite site, external therapy with topical antipruritic drugs (Fenistil gel, Psilobalzam) is also used, the patient is given a new generation antihistamine (loratadine, cetirizine, etc.). In case of a severe local reaction, topical non-fluorinated corticosteroids (methylprednisolone aciponate, mometasone furoate, etc.) are prescribed. In the most severe cases of local reaction, a 2-3-day course of prednisolone at a dose of 30-40 mg/day is justified.
In approximately 5% of patients with a history of severe local reaction, a repeated insect sting may develop a generalized systemic reaction with a life-threatening condition - anaphylactic shock. Most often, such reactions are caused by stings of wasps, bees, and less commonly, bumblebees and hornets; in 30% of cases, patients cannot name the type of insect that stung them.
In the United States, about 50 people die each year from insect sting allergies. Anaphylactic shock to a sting is also considered one of the causes of unexplained sudden death. The majority of deaths in 1998 in this country were observed in people aged 40–60 years, most often in men (28%), extremely rarely in children (1 case among children aged 0–9 years) [4]. In Kazan, according to prof. R. S. Fassakhova and co-authors, from 1993 to 1998, 55 patients with an allergy to insect stings aged from 16 to 70 years were admitted to the allergy department [5]. In 44% of cases, the reactions were caused by the sting of wasps, in 31% of cases - by bees, and by a hornet - in 1 case. In a population study, we did not identify a single case of systemic allergy to insect bites during a survey of 2147 Moscow schoolchildren (2003) [6].
Reactions to the sting of hymenoptera insects are divided into allergic, toxic and pseudo-allergic. Hypersensitivity to insect venom or saliva is triggered by immunological mechanisms of the immediate type with the inclusion of allergen-specific IgE antibodies. Toxic reactions occur when a large number of insects sting simultaneously and are induced by the action of a number of mediators contained in their venom. Based on the clinical picture, it is sometimes quite difficult to distinguish a toxic reaction from an allergic reaction. In some patients, 2–7 days after a sting, reactions resembling serum sickness may occur (arthralgia, urticarial rash, malaise, fever). Such patients, if stung again, have a high risk of developing anaphylactic shock [2].
We have already talked about local reactions to insect bites. Systemic reactions occur much more often than local ones (up to 70% of all cases of insect stings) and, according to some authors, can vary in severity [2, 4]. However, the clinical symptoms of anaphylactic shock caused by an insect sting, although they can vary in manifestations and severity, are no different from anaphylactic shock of any etiology [4].
In patients with anaphylactic shock, hemodynamic disturbances occur in 100% of cases: decreased blood pressure, weakness, dizziness. Other typical clinical symptoms of anaphylactic shock are diffuse erythema, rash, urticaria and/or angioedema; bronchospasm; laryngoedema and/or cardiac arrhythmia. The patient may also experience symptoms such as nausea, vomiting, headache, loss of consciousness; in 5–8% of cases - headache, convulsions, chest pain.
Generalized urticaria or angioedema is the most common clinical manifestation of anaphylaxis (92%) and is observed both in isolation as a single symptom and against the background of severe anaphylaxis [7]. However, skin symptoms may appear later or be absent if anaphylaxis progresses rapidly. The next most common symptoms are respiratory (angioedema of the larynx, acute bronchospasm), abdominal and gastrointestinal symptoms (abdominal pain, nausea, diarrhea) are less common.
Most often, symptoms of anaphylactic shock appear within the first 15 minutes after a sting, and early onset is almost always associated with a more severe course and, accordingly, severe symptoms of the disease. Children have a lower risk of developing recurrent anaphylaxis, especially if their allergy to the sting manifested itself in the form of skin symptoms (urticaria, rash, angioedema). However, in patients of any age with a history of primary severe anaphylactic shock, repeated insect stings can result in relapse of anaphylaxis in 70% of cases [2].
Since the life-threatening symptoms of anaphylaxis can recur, patients should be observed within the first 24 hours after the first manifestations of the disease (in 20% of cases, anaphylactic shock can recur 8-12 hours after the first episode) [7]. Researchers note a biphasic course of anaphylaxis, which is not clinically different from each other, but requires the use of significantly higher doses of adrenaline.
Factors that increase the severity of anaphylactic shock or affect its treatment include the presence of bronchial asthma in the patient, concomitant diseases of the cardiovascular system, drug therapy with β-blockers (Anaprilin, Atenolol, Metoprolol, etc.), inhibitors of angiotensin-converting enzyme and monoamine oxidase. In such cases, on the one hand, the reaction of the respiratory tract to the inflammatory mediators released during anaphylaxis increases, and on the other, the influence of adrenaline decreases: along with severe anaphylaxis, paradoxical bradycardia, hypotension, and severe bronchospasm appear [7]. It has been experimentally proven that in such cases, to relieve bronchospasm and restore β-adrenergic sensitivity in a patient taking β-blockers, the dose of the non-selective β-agonist terbutaline must be increased 80 times [8]. The use of angiotensin-converting enzyme inhibitors (Capoten, Enap) in a number of patients causes coughing, swelling of the larynx or tongue, followed by the development of asphyxia. Monoamine oxidase inhibitors (moclobemide, nialamide, etc.) slow down the rate of breakdown of adrenaline, increasing its side effects [2, 8].
The largest number of deaths from insect allergies, recorded in the group of older people, is associated with the presence of concomitant cardiovascular diseases, taking medications and the presence of other age-related pathological changes in the body [8].
Treatment and prevention
Anaphylactic shock requires emergency treatment: the patient’s cardiac and respiratory activity is immediately assessed, and the adequacy of behavior is checked. The drug of choice for anaphylactic shock is adrenaline hydrochloride.
Adrenaline has the following properties:
- has a direct stimulating effect on β- and α-adrenergic receptors. The predominance of the effect of excitation of certain adrenergic receptors depends on the dose of the drug and the level of regional blood flow;
- can cause severe spasm of peripheral vessels, especially in diseases of the kidneys and other internal organs;
- in case of immediate type allergies, it prevents the release of histamine, serotonin, bradykinin and other inflammatory mediators from mast cells and basophils;
- stimulates metabolism, increasing oxygen consumption, causes the development of acidosis due to the accumulation of lactic acid, enhances lipolysis and contributes to the occurrence of hyperglycemia as a result of stimulation of glycogenolysis;
Depending on the range of doses used, it may have effects: - vasoconstrictor (on the kidneys, at an injection rate of 1 mcg/min);
- cardiac stimulant (activation of β-adrenergic receptors of the heart): at an injection rate of 1–4 mcg/min;
- increasing α-adrenergic stimulating agent: at an administration rate of 5 to 20 mcg/min;
- predominant α-adrenergic stimulant: at an injection rate > 20 mcg/min [8].
Adrenaline hydrochloride is produced in the form of a 0.1% solution in 1 ml ampoules (at a dilution of 1: 1000 or 1 mg/ml); for intravenous administration, 1 ml of a 0.1% solution of adrenaline is diluted in 9 ml of physiological solution. Adrenaline cannot be diluted in a solution of glucose or sodium bicarbonate. It is important to remember that the activity of adrenaline is also affected by the storage conditions of the drug.
The recommended dosages for intravenous administration are as follows. If anaphylactic reactions develop: 0.1–0.3 ml of adrenaline (at a dilution of 1: 1000) is diluted in 9 ml of sodium chloride solution (from 1: 100,000 to 1: 33,000) followed by infusion for several minutes; repeated administration is possible in case of lack of sensitivity, as well as in case of persistent arterial hypotension.
In case of a severe terminal condition of the patient, a 0.1% solution of adrenaline in a dose of 0.1 ml is diluted in 0.9 ml of the patient’s venous blood (aspirated directly from a vein or catheter) or sodium chloride solution (to obtain a dilution of 1: 10,000), administered intravenously over several minutes; repeatedly - according to indications until systolic blood pressure is maintained above 100 mm Hg. Art. in adults and 50 mm Hg. Art. in children.
As a side effect, adrenaline can cause acute myocardial infarction, severe arrhythmias and metabolic acidosis; small (less than 1 mcg/min) doses of adrenaline can cause the development of acute renal failure.
The likelihood of developing such serious complications is the main reason for the recommendation to refrain from extensive use of epinephrine by patients themselves. However, timely administration of adrenaline is crucial for a favorable outcome of anaphylactic shock. Abroad, this problem has been solved: patients with any history of anaphylactic shock are provided with a special pen syringe - epinephrine in the form of an auto-injector (Epi-Pen, Ana-Kit). Studies are published annually in the scientific literature analyzing the use of epinephrine autoinjectors in patients with insect allergies, as well as a history of food, latex and idiopathic anaphylaxis. There are also studies that highlight the role of training programs for school nurses and school resource officers to promptly administer epinephrine to children with severe allergies and anaphylaxis, which is greatly facilitated by the use of an autoinjector.
Each patient who has suffered anaphylactic shock must be hospitalized in the intensive care unit, where infusion therapy with prednisolone 1–2 mg/kg every 6 hours, saline, and glucose is carried out at the rate of 5–10 ml/kg of the patient’s weight; antihistamines are administered intravenously. For resistant hypotension, dopamine (400 mg in 500 ml saline, injection rate 2–20 mcg/kg/min) is prescribed under blood pressure control (> 90 mmHg) or glucagon (1–5 mg bolus every 5 min). , then dropwise 5–15 mcg/min) until blood pressure normalizes. After 1–2 days, the patient is transferred from the intensive care unit to the allergy or therapeutic department, where he continues hormonal therapy with prednisolone orally at a dose of 10–15 mg for 10 days; prescribe second generation antihistamines (loratadine, cetirizine, etc.), antibiotics (according to indications), monitor kidney, liver, heart function, ECG, and consult a neurologist.
The diagnosis of IgE hypersensitivity to insects must be confirmed by skin or serological tests. To make a correct diagnosis and prescribe allergen-specific therapy, it is important to determine the type of insect that caused the reaction. A local reaction without systemic manifestations (anaphylactic shock) does not require an allergy examination. On the contrary, skin tests for insect allergens are mandatory if a patient of any age has a history of systemic reactions of a life-threatening nature, as well as non-life-threatening systemic manifestations in adults and children (under 16 years of age). Testing is also possible if the patient has a history of local and toxic reactions [4]. In vitro tests have been developed to determine specific IgE antibodies, for example: to the venom of the honey bee, wasp, hornet, horsefly, common mosquito, miller moth, barn weevil, pigeon mite, clothes moth (Allergopharma).
For patients with an allergy to insect stings, allergen-specific therapy is prescribed only in two cases: with a systemic life-threatening reaction and a systemic, non-life-threatening reaction in adults with positive skin tests. Children under 16 years of age with non-life-threatening skin manifestations (for example, generalized urticaria) do not need allergen-specific immunotherapy, even if there are positive specific IgE antibodies in the blood. The duration of specific immunotherapy is at least 5 years [2, 5].
Treatment of patients with allergies to insect stings is a multi-step process, much more complex than doctors and patients themselves sometimes assume. The problem is also that in Russia tests for diagnosing insect allergies are still not produced, and most importantly, there are no domestic or foreign allergen vaccines necessary for carrying out allergen-specific immunotherapy for those patients who need this method of treatment for health reasons. The “rescue” drug adrenaline in the appropriate release form and required dosage is also not available in Russia for patients with severe allergies and a history of anaphylactic shock.
The relevant medical authorities need to consider ways to overcome all these adverse situations. Part of the way to achieve a breakthrough in this direction is to teach patients simple preventive measures, which are often decisive in saving their lives. Patients must follow certain rules, in particular not to attract insects and avoid their bites, for which:
- do not wear perfume or wear bright clothes;
- do not eat ripe fruits on the street, do not go close to garbage cans and compost pits, which attract insects;
- Do not open the car windows while driving.
Parents, teachers and schoolchildren should be made aware of the need to ensure a safe environment for a child at high risk of anaphylactic reactions to insect bites. Each patient with an allergy to insect stings should have a tag or bracelet with information about their diagnosis and written recommendations for emergency measures in the event of a sting [1–5].
For questions regarding literature, please contact the editor.
D. Sh. Macharadze , Doctor of Medical Sciences, Professor of RUDN University, Moscow
Treatment
An allergic reaction is a very unpleasant problem that cannot be predicted, even if you know about it. A person should avoid contact as much as possible with those organisms whose poison causes a reaction, but it is very difficult to completely eliminate interaction.
People with insect allergies should be extremely careful and attentive. It is difficult to prevent a bite, but you can reduce its manifestations and eliminate the risk of adverse consequences.
The reaction to an insect bite that causes an allergy should be immediate. Depending on the symptoms that arise, local, systemic or combined treatment should be carried out.
Causes
Urticaria is a group of pathologies of an allergic nature, the basis of the pathogenesis (mechanism of development) of which is an immediate hypersensitivity reaction. The leading symptom is the presence of rapidly emerging and severely itchy blisters that disappear without a trace within up to 24 hours without secondary skin changes. There are several main reasons for the development of urticaria:
- Food products (citrus fruits, fish, nuts, peanuts).
- Medicines (antibiotics, vitamins, non-steroidal anti-inflammatory drugs).
- Insect bites (wasps, bees, hornets).
- Infectious agents (viruses, bacteria, fungi, helminths).
- Autoimmune pathologies (systemic lupus erythematosus, rheumatoid arthritis).
- Physical triggers (low and high temperature, vibration, sunlight, pressure, humidity).
Factors that contribute to the development of urticaria include:
- hereditary predisposition;
- diseases of the digestive tract, endocrine and nervous systems;
- infections and neoplasms.
Stress plays a part. It has been proven that nervous tension (including due to a change of place of residence, climatic conditions) affects the immune system and can lead to malfunctions in its functioning, which sometimes results in allergic sensitivity.
General recommendations
Each insect bite causes a local response of varying severity. People who don't have allergies just wait for it to go away. To alleviate your condition, you can take certain measures:
- Applying ice to the bite site;
- Applying a vinegar solution to the affected area;
- Rinsing the wound under cold water (in case of stings from wasps, bumblebees, bees, etc.)2.
You should not get carried away with folk remedies, especially herbal decoctions or alcohol tinctures, which can aggravate the situation. It is recommended to avoid any foreign protein structures at the site of the allergen.
Symptoms in children
Patients belonging to the younger age group often experience urticaria associated with food or drugs, as well as other triggers. Allergies in a child are characterized by the following symptoms:
- swelling and itching of the skin;
- the appearance of a rash in the form of blisters;
- increase in body temperature.
Fever can be observed even in infants and often causes misdiagnosis of infection, as it can reach high numbers. Children can suffer a systemic or generalized form of urticaria, which is combined with angioedema and is considered a life-threatening condition. But even with a mild reaction, the need to itch can lead to skin defects (wounds, ulcers) and infection.
Systemic drugs
When a person is bitten by an insect that causes an allergic reaction, it is recommended, regardless of symptoms, to take an antihistamine tablet to prevent the risk of systemic reactions.3 People with allergies are advised to carry Cetrin, which causes fewer side effects and is more potent than first-generation drugs.
Instead of antihistamines or in case of a pronounced response of the body to poison or saliva, Prednisolone tablets can be used in addition to them. It is not recommended to drink them in courses without medical supervision, but they are suitable as a one-time emergency aid3.
In case of severe systemic reactions or increasing swelling of the larynx, or any other disturbances in the general condition, it is recommended to call an ambulance. Cetrin tablet, if taken immediately after an insect bite, reduces the risk of developing severe symptoms.
Bibliography:
- Vertkin, A. JI. Acute allergic diseases: social consequences of the epidemic Text. / A.JI. Vertkin, A.V. Dadykina, K.K. Turlu-bekov // Remedium. 2004. - No. 4. - P. 22-28.
- Gushchin I. S., Chitaeva V. G. Allergy to insects - M.: Farmarus Print, 2003. - pp. 68–85, 120–210.
- Shvets S. M. Allergic reactions to the venom of stinging insects. Russian allergological journal, 2004, N3, p. 9–18.
Symptoms in adults
Urticaria is classified as:
- acute (episodes of rash observed over a period of time lasting less than 6 weeks);
- chronic (repeated for more than 2 months);
- localized (rash occurs in separate areas of the skin);
- systemic (blisters cover the entire body).
Urticaria is a disease in which not only the skin is involved in the pathological process. There are likely additional signs that determine the severity of the sensitivity reaction.
Dermatological manifestations
The dominant group of symptoms, characterized by damage to the skin. Observed:
Blisters due to urticaria can be localized on absolutely any part of the body. Location on the scalp, palms and soles is not excluded. They itch very much.
If the rash occurs on the face, it practically does not rise above the skin level. The elements start out pink and soon become porcelain. This occurs due to compression of blood vessels as a result of increasing edema. Then, as the swelling decreases, the blisters turn red again and then disappear from the surface of the skin.
Quincke's edema
This form of reaction can be classified as a dermatological manifestation, but it is worth considering it separately. According to statistics, more than half of the episodes of urticaria are accompanied by angioedema; it is a dense swelling affecting the subcutaneous tissue. There is no intense itching. Changes can be localized in areas such as:
- face (lips, cheeks, eyelids, ears);
- external genitalia;
- oral cavity, nasopharynx;
- mucous membranes of the digestive and urinary organs.
The most dangerous is Quincke's edema in the larynx - it causes a narrowing of the airway and can lead to asphyxia (suffocation).
Additional manifestations
Allergies that look like mosquito bites can be characterized by the following symptoms:
- General weakness.
- Increased body temperature.
- Runny nose.
- Watery eyes, swelling of the eyelids.
- Pain in muscles and joints without specific localization.
Sometimes patients are bothered by a cough; symptoms of damage to the digestive tract are likely - lack of appetite, nausea and vomiting, as well as diarrhea in combination with flatulence and abdominal pain. These signs can be associated either directly with urticaria or with Quincke's edema.
An allergy sufferer may complain of fatigue, poor sleep, becomes irritable due to itching, and is unable to concentrate on everyday tasks.
What to do if bitten by a fly?
You can quickly eliminate pain, redness, inflammation and itching using a variety of means. Scratching the wound is fraught with infection and other unpleasant complications. To treat a fly bite you must:
- Treat the affected area with hydrogen peroxide - you can use any disinfectant;
- Eliminate itching - special ointments, creams or gels will help with this;
- Taking an antihistamine is necessary to prevent allergic reactions in time.
The danger of a fly bite cannot be underestimated. If the affected area is very swollen or festering, with severe pain or a strong increase in temperature, you should consult a doctor. Timely diagnosis by a specialist will help determine or refute the presence of an infectious disease.
Fly bites are especially unpleasant in children. Kids lead active lifestyles and often neglect protective measures against insects (for example, staying away from landfills, garbage cans, or certain pets). Children's skin is very thin, so flies can bite even through clothing. The most important thing when detecting a bite in a child is to eliminate the itching. The baby can scratch the wound too much and cause an infection. Medical products intended for children will help cope with this problem.
You can protect yourself from insects using a number of effective measures. The simplest and most common are fumigators and mosquito nets. When planning a picnic in nature, do not forget about repellents. Special sprays or ointments for adults and children guarantee reliable protection against various insects.
A wide range of protective products against flies is available on our website. With us you can choose the ideal substance that will take care of your health.
Repellents
A repellent is a substance that repels insects and thereby prevents their attack. That is, repellents are remedies for mosquito bites for children. They differ in their mode of action and the substances included in their composition.
The repellent repels insects and thereby prevents their attack.
Available in the form of creams, ointments, aerosols and other devices. On the shelves of shops and pharmacies you can find the most popular of them:
- Levrana . Available in spray form. Suitable for use in young children. It is a natural mosquito repellent.
- Off Kids . It can also be used in young children.
- Special mosquito repellent bracelets. As a rule, they are made of hypoallergenic material and also provide protection from mosquitoes.
- Spray Picnic . It lies quite comfortably on the skin and allows you to protect your baby from harmful insects.
There are stronger repellents that may have age restrictions. As a rule, they contain not natural, but chemical substances in varying concentrations. The most popular chemical is diethyltoluamide (DEET). Among the powerful remedies it is worth noting:
- Aerosol DEET.
- Aerosol Mosquitall.
- Raptor.
- Komaroff.
- Off extreme.
- Picnic super.
- Gardex extreme is super.
Characteristics of mosquitoes
The common mosquito is a blood-sucking insect that is distributed everywhere, mainly near water bodies. Their sizes vary from 4 to 8 mm. The life cycle of a mosquito is a series of specific sequential stages, during which mature mosquitoes - adults - are formed from eggs.
For the purpose of reproduction, the female mosquito lays eggs in warm, stagnant water. The role of such reservoirs is mainly ponds, stakes, wetlands, rivers and many others. The development of a mosquito in water takes up to seven to eight days. It all depends on the temperature of the water in which the eggs are located.
Contact with mosquito saliva leads to the development of allergic reactions.
When considering the topic of mosquitoes, it is very important to understand the diet of mosquitoes. The feeding of mosquitoes will allow us to understand how and for what purpose this type of insect often disturbs people so much. Only female mosquitoes bite people. At the site of the bite, the female injects her saliva, which to some extent helps to numb the area. It is contact with mosquito saliva that leads to the development of allergic reactions. It is worth noting that in addition to allergies, mosquito damage can lead to the development of various infections. Human blood is necessary for the development of eggs; the rest of their needs are provided by sugars, which they receive from the juices of various plants.
Prevention and useful tips
To avoid recurrence of urticaria, you must:
- Avoid contact with triggers.
- Stick to a hypoallergenic diet.
- Take a course of treatment.
People who are aware of a tendency to sensitivity reactions should carry antihistamine tablets (for example, Cetrin). You should choose drugs without a sedative (calming) effect - otherwise drowsiness and decreased ability to concentrate are possible.
If a child suffers from urticaria, you need to warn the adults around him about the diagnosis. These are older relatives (grandparents, etc.), a kindergarten teacher, a school teacher, and a teacher in a club or sports section. It is better if your son or daughter always has with him the medications recommended by the doctor to relieve the symptoms of urticaria, as well as a card indicating the diagnosis and the contact number of the family.
- Spring Fever: Let's Say Yes! healthy lifestyle
- Fitness from the cradle: introducing your child to a healthy lifestyle
- Healthy eating pyramid
- Cold allergy: what you need to know
- What you need to know about allergies
Healthy lifestyle © 2022 Attention! The information published on the site is for informational purposes only and does not constitute a recommendation for use. Be sure to consult with your doctor!
How to help a child with mosquito bites
- The first thing you need to do is wash the bite area on your baby with cold running water and soap.
- After washing, it is recommended to treat the affected area with an antiseptic. A 3% solution of hydrogen peroxide can be used as such an antiseptic. Other alcohol-containing antiseptics are also suitable.
- Then mosquito bite remedies for children are applied to the affected area.
Parents of children often ask the following questions: “What to apply to a child’s mosquito bite? What helps against mosquito bites for children? How to treat mosquito bites for a child? How to treat mosquito bites in a child? Next, we will consider the rating of the best remedies against mosquito bites, which allow you to achieve a reduction in inflammation, itching, redness and swelling at the site of the lesion in the shortest possible time. Consideration of this issue will allow you to quickly understand what is best to use after a mosquito bite for children.
Diagnostics
There are several main clinical criteria in favor of urticaria:
- Sudden onset of itching and blisters.
- The presence of a connection with the allergen (most often, contact with it occurs 30–60 minutes before signs of a reaction appear).
- The fleeting nature of the rash (that is, rapid disappearance without secondary elements).
In addition, anamnesis is important - information about past episodes of pathology, the presence of allergies (not necessarily urticaria) in close relatives. Additional methods are used to clarify the diagnosis.
Laboratory tests
May include different types of tests - from basic general clinical ones (determining the level of hemoglobin, red blood cells, counting leukocytes, examining urine and feces) to complex special ones:
- enzyme-linked immunosorbent assay (ELISA) to detect antibodies to reaction provocateurs - food products, insect venom, etc.;
- determination of markers of infections (in particular, viral hepatitis);
- serum tryptase level test;
- assessment of thyroid function indicators (hormonal panel).
It is also important to identify signs of helminthiasis, for which stool is examined for worm eggs and the use of ELISA to detect antibodies to parasites (giardia, opisthorchid, toxocara).
Skin tests
These are provocative tests to check for sensitivity. They involve applying a potential trigger to the forearm or back and waiting within a specific time period (minutes, hours).
For example, if the patient reacts to cold, a piece of ice in a moisture-proof wrapper is applied to the skin (to prevent contact with water, which can also cause urticaria). In case of intolerance to drugs or food, use special media that contain the suspected allergen. If signs of a reaction (redness, swelling, itching, blister) occur during the observation period, sensitivity is considered proven.
Why are fly bites dangerous?
Many people believe that a fly bite is practically harmless and will not cause any trouble other than a little pain and itching. But we must not forget that this insect is a carrier of dangerous infectious diseases. Their pathogens enter the body along with poison from the proboscis. A fly bite can cause the following ailments:
- Typhoid fever;
- Polio;
- Dysentery;
- Cholera;
- Sepsis.
The insect can also spread other diseases - tuberculosis, anthrax, tularemia, tryposonosis. All these diseases are very dangerous for humans, especially for children, the elderly and pregnant women. Consequently, the appearance of a burner fly in a house can cause irreparable consequences. You need to get rid of them as soon as possible, because all infectious diseases caused by them are very difficult and take a long time to treat, and can lead to death.
Some subspecies of flies can use warm-blooded organisms as a substrate for reproduction, laying their eggs in it. Most often this happens to pets. In this case, the consequences of a fly bite are very sad, because over time, larvae hatch from the eggs. They cause severe dehydration, vomiting, diarrhea, and cramping pain in the abdominal area. Sometimes, due to damage to the intestinal walls, internal bleeding occurs.
Such patients are necessarily hospitalized in the infectious diseases department. Often, measures to replenish fluid lost by the body are sufficient for treatment. Sometimes measures are required to remove the larvae.
Ordinary house flies that do not bite are also dangerous. They love to scavenge in garbage, feces and other places filled with bacteria and infections. On their legs, insects carry various diseases, and can become pathogens of hepatitis, salmonellosis, brucellosis, and worms.