Which doctor should I go to for help with candidiasis in the groin?
Often patients are interested, if they still could not avoid the development of pathology, which doctor should be consulted first.
Only a doctor specializing in venereology can fully assess the characteristics of the rash, the severity of the lesion and other symptoms of candidiasis.
He is the one who treats and diagnoses STIs, which include candidiasis.
However, there are alternatives to a venereologist.
For example, you can seek help from a mycologist.
A doctor, unlike a venereologist or infectious disease specialist, has a narrower specialty, dealing with diseases caused by various pathogenic fungi.
Since candida is a fungus, a mycologist can help a patient with symptoms of candidiasis.
Another option for men is a urologist, and for women a gynecologist.
These professionals, by virtue of their profession, are familiar with STIs and their symptoms, including candidiasis.
Moreover, urologists and gynecologists are often so familiar with such diseases that they can recommend treatment on a par with venereologists.
This is explained by the fact that the genitals are often affected by STDs.
Doctors specializing in diseases of these organs should be able to diagnose such pathologies and refer patients to the appropriate doctor, if possible.
Candidiasis in the groin: methods of diagnosis
Before starting treatment for groin candidiasis, it is necessary to confirm the diagnosis.
This is not always easy, especially if the patient may have pathologies that resemble a candida infection in their symptoms.
First of all, an inspection is carried out.
Based on the results, the doctor evaluates the rash, the severity of swelling and other symptoms.
After this, the question of how to differentiate candidiasis using laboratory methods is resolved.
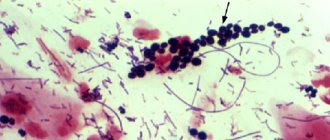
First of all, the patient is recommended to undergo a smear test.
In women, a smear is taken quite easily.
Men will have to endure several unpleasant minutes.
However, the effectiveness of collecting material in terms of diagnostics is high, and therefore you should not refuse.
The resulting smear can be examined in several different ways.
Most often, in addition to microscopy, sensitivity culture is performed.
Thanks to him, the doctor receives information about what medications can be used to treat the disease, and also confirms the diagnosis.
Additionally, PCR tests and scrapings are often done.
Additional research is especially important in doubtful cases.
When a patient, for example, also has symptoms of inguinal athlete's foot or an allergic reaction, and it is necessary to differentiate the diseases from each other.
In children, it is especially important to pay attention to analysis.
Diaper rash and allergies in the groin area are similar to candidiasis.
Causes of inguinal mycosis
The disease occurs due to a combination of several reasons: the action of a pathogenic or opportunistic pathogen, the characteristics of the body and unfavorable external conditions. Inguinal mycosis of the skin in 40% of cases is caused by Epidermophyton floccosum, in 25% by Trichophytom mentagrophytes var. interdigitale and in 20% - Trichophytom rubrum. In other patients, the disease is caused by fungi of the genus Candida, mold microorganisms, or their combination with dermatomycetes.
- E. floccosum and T. rubrum often lead to the development of a chronic form of the disease, and T. Mentagrophytes causes an acute inflammatory process.
Damage to the inguinal folds is often combined with atopic dermatitis and mycosis of the feet.
Inguinal ringworm is easily transmitted from person to person by using the same towels. In addition, the fungus can be transferred independently from the area of the sole with mycosis of the foot.
Fungi thrive in warm, moist places. They secrete enzymes that destroy the surface layer of the skin. This allows them to gain a good foothold in the groin areas. There are conditions that increase the risk of contracting this mycosis:
- male gender;
- obesity;
- excessive sweating;
- immunodeficiency;
- dermatitis in the groin area;
- diabetes;
- use of tight underwear;
- frequent exposure to wet clothes or a bathing suit;
- living in a tropical climate.
Candidiasis in the groin: treatment
Treatment of candidiasis in the groin in men and women should be prescribed by the attending physician, based on the symptoms of the disease and its characteristics.
The question of what to anoint rashes with is, of course, relevant.
However, no competent doctor can simply name the drugs, especially if the diagnosis is not confirmed by a number of tests.
After the diagnosis is confirmed using laboratory techniques, medications are prescribed to correct the condition.
Most often, the doctor prescribes ointments.
For example, Nystatin, Miconazole, Ketoconazole.
The optimal ointment is selected based on the results of culture and sensitivity determination.
In some cases, the patient's condition is so advanced that systemic treatment is required in addition to local therapy.
It is recommended to use Fluconazole as an oral (tablet) drug taken orally.
The drug is taken in the dosage recommended by the doctor.
It is important to consider the possible development of treatment complications and side effects of drugs.
If a person develops signs indicating poor tolerance to the medication, he is advised to inform his doctor.
The doctor will select an alternative, replacing a drug that is poorly tolerated.
Symptoms: rash, burning and itching
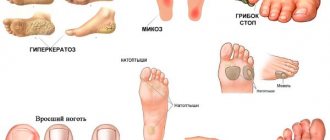
Inguinal athlete's foot in men has pronounced clinical symptoms. Red, scaly spots appear in the groin folds or on the inner thighs. In the center they are almost no different from healthy skin, but at the edges they are red or red-pink. This is how the initial stage of the disease manifests itself.
Gradually the number of spots increases, they merge with each other. The meeting point of the spots is called the focus. It is in the foci that scales (which, falling off, are visualized as peeling), blisters and pustules are localized. All this causes burning and itching.
The contour of epidermophytosis is characterized by wavy edges (in dermatology they are called the beautiful word “scalloped”) and an elevation above healthy skin. In appearance, the roller-shaped outline resembles a red worm curled into a ring at the site of the pathology. In medicine, this symptom is called a more euphonious phrase - “cord symptom.”
Treatment of candidiasis in the groin with folk remedies
The regimen and duration of treatment for candidiasis in the genital tract may be reduced.
In the event that the patient uses traditional methods in addition to medications.
Traditional medicine, of course, cannot cope with the disease when used in isolation.
However, they can speed up the effect of medications and alleviate the symptoms of the disease during the main treatment.
Naturally, the use of traditional medicine recommendations is possible only after the doctor’s approval has been received.
The patient may be recommended, for example, lotions with chamomile infusion or chamomile baths.
Herbs that have an antibacterial effect have a good effect.
They also prevent the development of secondary infectious processes.
All patients, regardless of the duration of treatment and the regimen used, are recommended to undergo follow-up tests after treatment.
With their help, it will be possible to confirm that the therapy was successful.
Based on the results of control tests, the patient is also deregistered from the skin and venereal disease clinic, if he was there.
Why are fungal infections dangerous?
Mycoses have a variety of symptoms. Almost always there is severe itching, an unpleasant odor, and possible pain.
However, the main danger is that fungi quickly spread throughout the body and affect new areas. A systemic infection cannot be ruled out when pathogens penetrate deeply into tissues and organs. The patient experiences weakness, pain, suffers from digestive disorders, toxicosis, and skin rashes.
Without the help of a specialist, the disease worsens and becomes chronic with frequent exacerbations. In the most severe cases, sepsis and death cannot be ruled out. The sooner you see a doctor, the easier it will be to get rid of pathogenic flora.
Home remedies cannot cure the infection. At best, it will go into “sleep” mode. The patient is not able to independently identify the pathogen and, accordingly, choose the correct treatment method.
Recommendations for the prevention of candidiasis in the groin
Genital candidiasis is one of those diseases whose development is much easier to prevent.
What then to do with long and rather expensive treatment, as well as get rid of side effects.
To prevent infection, people should follow the following recommendations:
- When having sex, follow basic safety rules, without refusing to use condoms, especially if you are not completely confident in your partner’s health
- Always remember personal hygiene by not using other people's items from this area
- When visiting public swimming pools and baths, rinse thoroughly in the shower after sessions
- When taking glucocorticosteroids, antibiotics and immunosuppressants, carefully observe the dosage and duration of therapy as recommended by the attending physician
- promptly treat identified diseases of the genital organs, not only infectious, but also of other origins
- devote time to hardening the body so that the immune system does not weaken under the influence of stress and other negative environmental factors
- treat diseases of the endocrine system in a timely manner; if you have diabetes, make efforts to take the disease under control
Unfortunately, doctors note, even following these simple recommendations cannot protect against candidiasis 100%.
However, if you follow these recommendations, the likelihood of encountering the disease during your life will be significantly reduced.
Is sex acceptable during candidiasis treatment?
Often men and women who have received a diagnosis from a doctor wonder whether sex is possible during treatment.
Doctors draw the attention of their patients to the fact that sex will have to be excluded for the entire period of therapy.
This is due to several factors.
Firstly, it is recommended to undergo therapy not only for the first one of the couple to seek help, but also for his sexual partner.
Secondly, if you do not refuse sexual contact, re-infection will occur as soon as the therapy is completed.
It would seem that a condom should provide protection from the transmission of infection.
This is actually true, but it is important to remember that candidiasis can affect not only the genitals, but also the skin around them.
And the skin is often not covered with a contraceptive, which means there is no protection in this area.
We also must not forget that the condom may break or be initially incorrectly selected.
Then the degree of protection against infection decreases even more.
How to cure a fungal genital infection?
Dermatovenerologists at the Polyklnika+1 clinic are fluent in the specialty of mycology. That is why you will receive qualified diagnostics and treatment from us.
Doctors of the first category V. A. Malashenko and R. A. Guseinov use modern methods to detect mycosis at an early stage, even if it is disguised as a bacterial STI. We carry out research:
- an imprint from the glans penis, labia, foreskin, as well as scraping of scales from skin rashes using microscopy;
- smear from the vagina, urethra, cervical canal;
- Fungal DNA in mucosal scrapings (PCR method).
The results of these tests are ready in half an hour or the next day. In addition, within seven days you will receive a response to sowing the biomaterial on nutrient media. Such a study allows us to determine the type of pathogen, its quantity and the degree of sensitivity to drugs.
Guided by the results of the research, specialists at the Tretyakovskaya clinic are drawing up a comprehensive treatment regimen for fungal infections of the genital organs. They take into account factors such as:
- severity of inflammation;
- damage to the mucosa;
- presence of edema.
In accordance with this, the patient is prescribed antifungal, antibacterial, hormonal, wound-healing drugs - in the form of tablets, ointments, intravenous injections. If necessary, immunomodulators and probiotics are prescribed.
The treatment process takes from a week to several months, depending on the severity of the disease. Thanks to the experience and knowledge of our doctors, therapy gives excellent results and minimizes the possibility of relapse.