4.3
(27)
Fungal infections can occur in any part of the body. Often mycoses choose the groin area as their habitat. How to eliminate fungus in the groin, medications that are effective in men, inexpensive medications and methods of their use will be described in this article.
How do they get infected?
Transmission of the fungus is possible direct, indirect and indirect:
- direct – from a mycotic carrier or a patient as a result of close contact;
- indirect - through various objects contaminated with skin scales containing a pathogenic microorganism;
- indirect (autoinoculation) – transfer of infection from one part of the body to another: in particular from lesions on the arms and/or legs.
It is worth noting that the most common route of transmission of the fungus is indirect. Contaminated items may include other people's sheets, clothing, towels, beach chairs, toilet seats, surgical and personal instruments.
General information
Fungal diseases, which include inguinal mycosis (synonymous with dermatomycosis inguinal), are infectious.
Fungal infections are caused by various types of fungi that can affect the skin, mucous membranes, nails or hair. Inguinal dermatomycosis is a collective term that unites similar lesions of skin folds caused by various pathogenic fungi. The causative agents of dermatomycosis feed on organic compounds ( keratin of human tissues), are highly contagious and are transmitted from person to person through household items, which requires strict adherence to the rules of personal hygiene. You can become infected by visiting baths, swimming pools, saunas, or using other people's bath accessories, rugs or bedding. The most common pathogens that cause groin fungus are Epidermophyton floccosum, Trichophyton rubrum, Trichophyton mentagrofitis var. Interdigitale. Molds and Candida fungi in rare cases independently lead to the disease, but are found together with dermatophytes. Considering the prevalence of dermatomycosis and its tendency to become chronic, it is important to know everything about this pathology - its prevention and proper treatment in order to achieve stable remission.
Basic principles of treatment
Therapy for fungal infections is carried out in 3 directions and includes, respectively, 3 groups of drugs:
- fungistatics to suppress the growth and reproduction of fungal flora;
- fungicides to eliminate fungus;
- local remedies to relieve symptoms in the form of irritation, itching and burning.
The main stages of treating fungus in the groin
Treatment of dermatophytosis necessarily also includes measures to eliminate the causative factors. It is very important to get rid of the influence of conditions that contribute to the development of the disease and/or that appear during its progression.
The basis of treatment are drugs from the category of imidazoles, triazoles and allylamines. The new generation antimycotic Luliconazole has a very powerful effect - it effectively fights different types of fungus and has a wider spectrum of activity compared to Terbinafine. This still little-known drug is used in the form of a cream, which is applied to the skin once a day for 1-2 weeks.
Prevention of infection
To reduce the risk of contracting ringworm during treatment, the affected family member should follow the following recommendations:
- It is better to get rid of underwear and other synthetic wardrobe items that have been in contact with fungus-infected skin. It will not be possible to clean them 100% of spores, since synthetic fabrics are difficult to heat treat.
- During the treatment period, regularly treat all surfaces in the bathroom with water with the addition of a solution of Chlorhexidine or hydrogen peroxide.
- At the end of the course of treatment, buy new underwear.
Healthy skin with a normal protective barrier effectively copes with attacks from fungi and other pathogens. To maintain normal skin condition, you should balance your diet, drink enough fluids and ensure regular moderate physical activity.
For severe itching and burning - antihistamines
For inguinal fungus, local treatment is usually sufficient, but oral antihistamines may be prescribed to relieve itching and discomfort:
- Loratadine;
- Clemastine;
- Chloropyramine;
- Cetirizine.
Solutions of silver nitrate and resorcinol, ointments with betamethasone and clotrimazole are used as local remedies. Medicines such as Terbinafine and Undecylenic acid show good results.
The course of antimycotic therapy lasts a month and a half and continues even after the symptoms disappear. The affected areas are also lubricated with iodine or Fucarcin.
If the skin becomes very inflamed, then apply lotions with Ichthyol and brilliant green. Ichthyol ointment 5-10% is applied to the area of the inguinal folds 2-3 times a day, Diamond Green - 1-2 times. Inflammatory reactions pass quite quickly, within a maximum of 2 days.
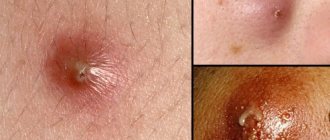
Yellow discharge in women and purulent rash
Purulent rashes may appear on the labia and mucous membranes of the vulva. This is a sign of a bacterial infection. The clinical picture is usually complemented by yellow vaginal discharge. Gradually, acne spreads to the pubic area, causing folliculitis (ulcers on the hair follicles).
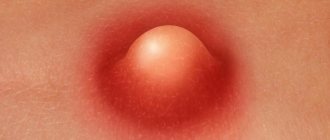
The pathology is easily treated - antibiotics, local antiseptics, drugs for immunity. However, the disease is dangerous because the infection spreads to the deeper layers of the skin. A boil forms at the site of damage to the fatty tissue. The formation is dense and painful. The pain radiates to the abdomen and rectum.
Often the formation of a subcutaneous boil ends in bartholinitis. This is an inflammation of the reproductive gland in the vestibule of the vagina. With bartholinitis, a large formation appears at the vaginal vault, which hurts and interferes with movement. Bartholinitis is treated surgically - the formation is opened, the pus is removed and washed with an antiseptic.
Fungus in the groin: treatment, drugs effective in men, inexpensive
No. 1 – Mikozolon ointment
For inguinal fungus, Mikozolon ointment is applied to the affected areas twice a day for a week. It is an antifungal, antiseptic and anti-inflammatory agent designed specifically to relieve inflammation and itching due to mycotic infections.
Mycozolon inhibits the growth of dermatophytes and other fungi, and also blocks the proliferation of bacterial flora. It has an anti-inflammatory effect and relieves allergic manifestations.
Why is mycosis of the groin area dangerous?
Ignoring inguinal mycosis is dangerous due to infection of healthy areas of the body, penetration of infection into the anus and urethra.
Fungus on the scrotum, penis and anogenital area leads to:
- balanoposthitis - inflammation of the head of the penis and foreskin;
- urethritis and cystitis - damage to the urethra and bladder;
- phimosis – scarring and narrowing of the foreskin;
- prostatitis - inflammation of the prostate.
When bacterial infections are added, it is dangerous for abscesses, chronic inflammation of the prostate, erectile dysfunction and infertility. If left untreated, Candida fungi multiply quickly and penetrate the colon mucosa. This is fraught with fungal proctitis and other complications.
Drugs of systemic – general – action
Tablets are rarely needed, since most patients recover mainly through the use of ointments and creams. General drugs are prescribed in case of extensive lesions and the development of complications.
Fungoterbin tablets are prescribed for common fungal processes, which are accompanied by a bright clinic
The basis of systemic treatment are azoles and allylamines:
- Ketoconazole;
- Itraconazole (1 time per day, 2 weeks);
- Fluconazole;
- Fungoterbin;
- Terbinafine (1 time per day, 2-3 weeks).
Epidermodermal mycoses of the skin in the practice of a dermatologist
Athlete's foot (synonym: "fringed eczema", true epidermophytosis) is a mycosis caused by the fungus Epidermophyton floccosum (flaky epidermophyton). The term "athlete's foot" is justified, in the strict sense, in relation only to this nosology.
The share of this fungus in the spectrum of fungal pathology is currently small - no more than 1.2–1.8%. Men get sick somewhat more often. Most of the primary diagnoses of athlete's foot upon further cultural examination turned out to be rubromycosis and were combined with onychomycosis [1, 4].
Infection with this fungus most often occurs indirectly, through objects that have been used by the patient (in baths, showers, etc.).
Clinic. Typical localization of lesions is the skin of large folds (inguinal, under the mammary glands, intergluteal). The formed lesion may contain spotted, papular, vesicular, pustular elements, i.e., there is a true polymorphism of elements within the lesion, bordered by a continuous, slightly edematous peripheral ridge. The severity of the allergic reaction to the presence of the fungus is characterized by the above sequence of primary elements: from the smallest with a predominance of spots to the maximum with abundant vesiculation, weeping and erosion.
In the center, resolution of the pathological process may begin, while acute phenomena still persist in the periphery. Subjectively, quite intense itching is noted [1, 7].
Diagnostics. In scrapings, as a rule, the mycelium of a pathogenic fungus is easily detected, except for cases when the material is taken from a lesion with a pronounced exudative component and oozing: in this case, difficulties arise in detecting the fungus, as noted by most laboratory technicians. This rule also applies to foot mycoses caused by other fungi [3, 7].
Inguinal athlete's foot should be differentiated primarily from candidiasis of large folds, which develops in obese individuals suffering from diabetes mellitus; In children, inguinal athlete's foot can mimic diaper dermatitis, which is also essentially candidiasis of large folds. Erythrasma rarely produces such pronounced inflammatory phenomena; in the rays of a Wood's lamp one can observe a “beautiful” coral-red glow. Eczema, including seborrheic, when localized in large folds, sometimes forms lesions similar to inguinal epidermophytosis [1, 2, 7]. Rubromycosis differs from inguinal athlete's foot by the presence of an intermittent peripheral ridge (N. S. Potekaev et al., 1972).
Athlete's foot is a chronic fungal disease. The lesions are localized on the skin of the arch and interdigital folds of the feet, and the nail plates are often affected.
The causative agent is Trichophyton mentagrophytes var. interdigitale. Trichophyton interdigitale accounts for 5–10% of all causative agents of foot mycosis in cities and 40–50% in rural areas [10].
Clinical picture. The incubation period has not been precisely established. There are several forms of mycosis: squamous, intertriginous, dyshidrotic, acute (described by O. N. Podvysotskaya in 1937) and onychomycosis. Secondary skin rashes are possible - epidermophytids (mycids), associated with the allergic properties of the fungus [2, 7].
The squamous form is manifested by peeling of the skin of the arch of the feet, sometimes against a hyperemic background. The process can spread to the lateral and flexor surfaces of the toes. With the squamous-hyperkeratotic type of athlete's foot, areas of diffuse thickening of the skin can form, similar to callus, with lamellar peeling. With erased forms, there are no subjective sensations.
The intertriginous form begins with subtle peeling of the skin in the third or fourth interdigital folds of the feet. Then the process takes on the appearance of diaper rash with a crack in the depths of the fold, surrounded by a peeling, whitish stratum corneum of the epidermis, accompanied by itching and sometimes burning. With prolonged walking, cracks can transform into erosions with a wet surface. Due to the addition of pyococcal and yeast flora, hyperemia and swelling of the skin develop, itching intensifies, and pain appears. The course is chronic, exacerbations are observed in the summer season [7].
The dyshidrotic form is characterized by the presence of vesicles with a thick horny covering, transparent or opalescent content (“sago grains”) on the arches, lower lateral surface and on the contacting surfaces of the toes. Bubbles are usually located in groups, prone to merging, forming multi-chamber, sometimes large bubbles with a tense tire. After their opening, erosions are formed, surrounded by a peripheral ridge of exfoliating epidermis. The contents of the vesicles (blisters) may be purulent if a pyococcal infection is associated. Some patients experience lymphangitis, lymphadenitis, accompanied by pain, general malaise, and increased body temperature.
Acute epidermophytosis occurs due to a sharp exacerbation of dyshidrotic and intertriginous forms. It is characterized by the rash of a large number of vesicular-bullous elements against the background of skin edema, sometimes significant; rashes may be accompanied by lymphadenitis, lymphangitis, fever, the addition of pyodermic complications, and disability [2, 7, 8].
Damage to the nails, most often the 1st and 5th toes of both feet, occurs in 20–25% of cases: the nails are thickened, yellow-gray, but, unlike rubromycosis of the nails, their loosening and fragility develop more slowly. In the initial stages of onychomycosis caused by interdigital trichophyton, lesions of the nail plate in the form of ocher-yellow stripes are characteristic.
In more than 2/3 of patients with athlete's foot, the disease occurs with mycids - toxic-allergic rashes in areas both bordering the lesion and distant, which also distinguishes this mycosis from rubromycosis, for which, in general, allergic reactions and the exudative component are much less characteristic. This is obviously explained by the antigenic composition of the cell wall of the interdigital trichophyton, to the presence of which a violent reaction develops.
Children are especially characterized by a condition called eczema by O. N. Podvysotskaya in the literature: after full antifungal treatment and the elimination of exudative manifestations of mycosis, the process suddenly worsens with renewed vigor. In this case, fungal elements are not detected in the lesions. Pyoderma complications quickly appear.
Diagnostics. The leading role in establishing a diagnosis in the acute period belongs to clinical symptoms, since fungi cannot always be detected from exudative foci. After the elimination of inflammation, the diagnosis in some cases is confirmed by the detection of a fungus from dry hyperkeratotic areas.
| Rice. 1. Mycosis of the skin of the chest |
Differential diagnosis. The dishidrotic form of mycosis should be differentiated from rubromycosis (Fig. 1), true epidermophytosis, superficial pyoderma, contact dermatitis; intertriginous form - from candidiasis, diaper rash [3, 5].
Rubromycosis (synonym: rubrophytosis) is mycosis of the skin and nails caused by red trichophyton (Trichophyton rubrum). The mushroom is named red because of its ability to deposit red pigment at the base of the colony when grown on Sabouraud's nutrient medium. This is a fungal disease prone to exacerbations and chronicity with a predominant localization of lesions on the skin of the feet, frequent damage to the nail plates of the toes and hands, large folds, skin of the torso and limbs, less often - the face, neck and scalp [2, 7, 8] .
Only people get sick; the fungus is a true anthropophile [5]. Infection occurs through prolonged contact with a patient with rubrophytia and the use of various things of the patient (loofah, pumice stone, scissors, shoes, etc.; when visiting bathhouses, showers, swimming pools, where infected people can remain for a long time on the floor, rugs, benches, floorings, and in wastewater fungus skin flakes and particles of destroyed nails). Rubrophytosis is often called a familial infection.
In Russia, there are more than 5 million patients with this mycosis (Yu. V. Sergeev, 2008). Onychomycosis accounts for more than 24% of all mycologist visits. The intensive growth rate of onychomycosis is about 5% per year.
The main source of infection is the family!
The incubation period has not been established. The development of mycosis is facilitated by various exogenous (excessive sweating or excessive dryness of the skin of the feet, injury to them by shoes, non-compliance with hygiene rules) and endogenous (endocrinopathies, immunodeficiency state, metabolic disorders, reduction of the body’s natural resistance due to the use of corticosteroids, cytostatics, antibiotics, etc.) factors [9].
Clinic. Men and women get sick with the same frequency [2, 7, 10].
Based on localization, rubromycosis is distinguished between smooth skin, palms and soles, and nails.
| Rice. 2. Mycosis of the skin of the leg |
On smooth skin, the disease exists in two forms - erythematosquamous and follicular-nodular. The erythematosquamous form is characterized by the formation of large lesions on the skin, consisting of spotted, papular and vesicular (rarely pyodermic) elements, as well as scales, crusts, and sometimes excoriations. In the center of long-existing lesions, spontaneous resolution of the process of the appearance of areas of atrophy and telangiectasia is sometimes observed, which gives the lesion a poikilodermic appearance (Fig. 2). Along the periphery there is an intermittent ridge of papules, vesicles and crusts. The appearance of diffuse erythema within the lesions is a clinical sign of long-term treatment with corticosteroid ointments; erythema develops even if these ointments contained an antifungal additive.
The follicular nodular form is essentially a trichophytosis granuloma (gumma Majocchi). This form usually characterizes the prolonged existence of the previous form without treatment. The process develops in the dermis, deep in the hair follicles and resembles zoonotic trichophytosis in the infiltration stage (formally, rubromycosis is the same trichophytosis, as it is caused by fungi of the genus Trichophyton) [5, 9].
| Rice. 3. Mycosis of the skin of the trunk |
Mycosis of the feet and hands can be represented by the following forms: intertriginous - characterized by cracks, maceration of the epidermis, single vesiculations in the interdigital folds of the feet, most often between the 4th and 5th fingers, rarely found on the hands; squamous - most often, as a rule, accompanies onychomycosis, is represented by hyperkeratosis of the palms and soles with a peculiar increase in the skin pattern, deepening of the furrows and “sprinkling” of these furrows with “flour” (floury peeling); when an exudative component is attached, the peeling becomes lamellar in nature; dyshidrotic - reminiscent of those affected by interdigital trichophyton: areas of “dry” mycosis alternate with vesiculations, sometimes with pustules, patients are bothered by severe itching [10].
Differential diagnosis. Other epidermodermal mycoses (athlete's foot inguinal), trichophytosis (Fig. 3), candidiasis of large folds, psoriasis; onychomycosis should be differentiated from damage caused by other fungi (candidal onychia, mold mycosis), Pseudomonas aeruginosa, as well as onychodystrophies of non-infectious etiology (psoriasis, especially pustular, lichen planus, acrodermatitis enteropathic, etc.).
Treatment of superficial mycoses
In this article we will consider only the principles of external therapy of superficial mycoses.
For acute inflammatory phenomena, lotions are prescribed from 1–2% resorcinol solution, 0.1% ethacridine lactate solution, 0.05–0.1% chlorhexidine digluconate solution, potassium permanganate solution 1:6000–1:8000. The cover of the vesicles (bubbles) is pierced with a needle (but not cut off with scissors!) in compliance with the rules of asepsis. To eliminate acute inflammatory phenomena, aerosols containing corticosteroids and antibiotics can be used. Subsequently, solutions of aniline dyes, pastes and ointments with antimycotics (tar 2–3%, sulfur 3–10%, salicylic acid 2–3%, tincture of iodine 2%), patented antimycotic drugs naftifine, terbinafine, oxiconazole, ketoconazole, bifonazole are used etc. It is also necessary to prescribe (especially in the presence of mycids) desensitizing agents and antihistamines, sometimes sedatives. In case of secondary pyococcal infection, short-term courses of broad-spectrum antibiotics are indicated [4–6].
For the erythematosquamous form of mycosis on smooth skin, it is recommended to start treatment with anti-inflammatory drugs (Mikozolon), 2% boron-tar paste, ASD paste. After the acute phenomena have subsided, you can use drugs with a mild disinfectant and non-irritating effect on the skin (Fukortsin). Usually, within a week, acute symptoms disappear, the process is transferred to a “dry” form. At this stage, you can begin to use more active antifungal therapy: 2% iodine in combination with 10% sulfur-3% salicylic ointment [4].
The follicular nodular form responds well to treatment using 2% iodine on the lesions in combination with sulfur-salicylic-tar ointment; It is advisable to prepare the latter on the basis of zinc ointment at the beginning of treatment, and later switch to a vaseline base.
The principles of treatment of dyshidrotic and intertriginous forms of skin lesions of the soles generally coincide with those for smooth skin; salicylic acid in ointments can be used in a 5% concentration. The principle of a step-by-step transition from anti-inflammatory drugs to active antifungal drugs is preserved [4].
In case of squamous-hyperkeratotic form of rubromycosis of the palms and soles, it is recommended to perform detachments of the stratum corneum according to G. K. Andriasyan under the supervision of a specialist dermatologist. After completing a series of detachments, you can prescribe one of the modern creams or Lamisil Uno solution.
Classification of modern antimycotics (means for external and internal use)
- Iodine preparations: potassium iodide - for internal use, iodine solutions - for external use.
- Antifungal antibiotics:
- griseofulvin;
- polyene antibiotics: Amphoglucamine, Amphotericin B, Levoridon, Levorin, Mycoheptin, Nystatin, Pimafucin.
- Azoles: isoconazole, itraconazole, ketoconazole, clotrimazole, metronidazole, miconazole, oxyconazole, fluconazole, econazole.
- Allylamines (from the Latin Allium sativum - garlic, Allium cepa - onion): naftifine, terbinafine.
- Morpholines: amorolfine (Loceryl).
- Flucytosine (Ancotil).
- Cyclopiroxolamine (Batrafen).
- Medicines of various chemical groups (others): preparations of undecylenic acid (Undecin, Zincundan), quinosol, urea; salicylic, lactic, acetic, benzoic acids; Octicyl, Anmarin, Decamine, aniline dyes, Nitrofungin.
- Combined antifungal ointments and creams: Mikozolon, Mikospor - cream in a set, Pimafucort, Travocort, Triderm.
Based on the type of action, antimycotics are divided into fungicidal and fungistatic (although many, such as allylamines, have a combined effect). Based on the method of obtaining these compounds, natural and synthetic ones are distinguished.
There are antimycotics of a narrow (griseofulvin) and broad (itraconazole - Orungal) spectrum of action.
Literature
- Kashkin P. N., Sheklakov N. D. Guide to medical mycology. M., 1978. 328 p.
- Leshchenko V. M. Fungal skin diseases. In the book: Skin and venereal diseases (a guide for doctors). Ed. Yu. K. Skripkina, V. N. Mordovtseva. M., 1999. T. 1. P. 257–311.
- Leshchenko V. M. Laboratory diagnosis of fungal diseases. M., 1982. 142 p.
- Rational pharmacotherapy of skin diseases and sexually transmitted infections: A guide for practitioners. Under general ed. A. A. Kubanova, V. I. Kisina. M.: Litera, 2005. pp. 312–346.
- Rukavishnikova V. M. Mycoses of the feet. M., 2003. 330 p.
- Guide to laboratory diagnosis of onychomycosis. Ed. A. Yu. Sergeeva. M.: GEOTAR Medicine, 2000. 154 p.
- Sergeev A. Yu., Sergeev Yu. V. Fungal infections (a guide for doctors). M., 2003. 185–193.
- Suvorova K. N., Kuklin V. T., Rukavishnikova V. M. Pediatric dermatovenereology: A guide for postgraduate medical students. Kazan, 1996. pp. 192–312.
- Fitzpatrick T., Johnson R., Wolfe K. et al. Dermatology: a reference atlas. M.: Praktika, 1999. pp. 696–740.
- Richardson MD, Warnock DW Fungal infection: Diagnosis and Management. 2nd edit. Blackwell Science Ltd., 1997. 249 p.
A. B. Yakovlev, Candidate of Medical Sciences, Associate Professor
GBOU DPO RMAPO Ministry of Health and Social Development of Russia , Moscow
Contact information about the author for correspondence
Price issue
Inexpensive but effective - how much do anti-fungal drugs actually cost?
| Name | Average price, rub | Volume, g |
| Mycozolon | 77-88 240 | 15 30 |
| Travocort | 830-1030 | 15 |
| Clotrimazole | 94-199 | 20 |
| Terbinafine | 85-88 240 | 15 30 |
| Triderm | 750-852 | 15 |
| Ecodax | 223 RUR | 10 |
Tips on how to get rid of fungus faster
Tip #1
An important condition for the treatment of dermatophytosis is the fight against sweating. You can reduce the negative impact of sweat by daily washing the skin folds with cool water. An alternative option is to wipe the skin with a damp towel and then dry thoroughly.
Tip #2
Dermatologists advise wiping the skin in the folds with one of the products from the following list:
- Salicylic alcohol 2% or tannin alcohol 1%;
- Amikazole;
- Levaril;
- Batrafen;
- Tolmitsen.
After treatment with salicylic or tannin alcohol, sprinkle the skin with boron powder.
Causes
The pathogen Epidermophyton floccosum accounts for 35-40%, Trichophytom mentagrophytes var. interdigitale were caused - up to 25% of cases, and Trichophytom rubrum - 15-20%. Infection with fungi occurs through objects used by the patient - towels, washcloths, sheets in baths and saunas, linen, bedpans (in hospitals, toilet mugs).
The development of inguinal dermatophytosis is promoted by:
- increased sweating ;
- increased air temperature;
- carbohydrate metabolism disorders ( diabetes mellitus , metabolic syndrome );
- the presence of abrasions and cracks in the skin;
- decreased body resistance ( HIV , AIDS, autoimmune diseases, anemia , cancer);
- long-term use of antibiotics and corticosteroids;
- chronic diseases ( bronchial asthma , systemic diseases).
At risk for this disease are persons who, due to their professional activities, are in conditions of high humidity (bathhouse attendants, swimmers, miners, rescuers, workers in hot shops).