- Types of melanoma and risk factors
- Treatment methods
- Surgical removal of melanoma
- Chemotherapy
- Radiation therapy
- Biological therapy
- Targeted therapy
- Consequences of treatment
Skin cancer includes three types of malignant tumors: melanoma, basal cell and squamous cell carcinoma. The most aggressive and difficult to treat skin cancer is melanoma; removal is accompanied by auxiliary therapy methods. This article discusses in detail the features of treatment of skin melanoma.
Wide excision
If a biopsy is diagnosed as melanoma, it must be completely removed.
The surgeon excises the tumor and some healthy tissue around it and underneath it. Normal tissue is captured in order to completely remove all tumor cells. After surgical removal, the skin melanoma is sent to a laboratory for analysis. It is important to check the resection margin - the area of tissue that is located at the incision site. If only healthy tissue is found here, then the resection margin is negative, which means that the tumor has been completely removed. If malignant cells are found at the resection margin, it is called positive. This suggests that the tumor tissue may not have been completely removed. The more healthy tissue the surgeon captures during surgery, the higher the likelihood that the resection margin will be negative. But in some places, for example on the face, the cosmetic effect is important. In such cases, you need to look for a middle ground: try to remove as little surrounding healthy tissue as possible, but so as to completely excise the melanoma and not leave tumor cells in the skin. After surgery, your doctor may prescribe a course of adjuvant chemotherapy. In some cases, if the melanoma is on an arm or leg, amputation is performed. Is it possible to perform laser removal of melanoma? Laser surgery is widely used to remove moles, but it often does not provide any benefit for melanoma. Melanoma is a potentially fatal disease that is a surgical pathology and in most cases must be excised with a scalpel. Most often, the operation is performed under local anesthesia. One of the possible consequences of laser removal of melanoma is that there may simply be no material left for a biopsy; all tumor tissue will be destroyed by the laser. Laser surgery is sometimes used in the early stages of tumors, usually in older people.
Patient reviews
Boris Grachev: For three years now I have been treated with Keytruda for metastatic melanoma. And all these years with Dr. Aronov at Medis. Previously, I had it operated on by a surgeon I knew, but it soon metastasized. If it weren't for this medicine, I would no longer exist. And for this medicine, for the protocol from Professor Schechter, I express my gratitude to all the staff of the clinic. The clinic’s logical and quick actions have always been effective. I am being treated in the only possible way in the world. There is remission. I am staying on these medications.
Anatoly Solntsev: When I realized that I had an abnormal mole, I went to a dermatologist in a private clinic. He said it was melanoma and suggested removing it with a laser. I turned the entire Internet to understand the situation as soon as I found out how deadly this disease is. As a result, I went to Medis and was operated on by a surgeon who did it surgically, removing everything deep down. It certainly cost more, but I didn’t see any other alternative.
Lymph node excision
After the diagnosis of melanoma is confirmed, it is necessary to check the lymph nodes close to the tumor (they are called regional) - perhaps the tumor cells have managed to spread into them. Computed tomography, MRI, PET scan, and fine-needle biopsy of lymph nodes are performed. If they are also affected, they are excised. If, according to the examination, the regional lymph nodes are not affected, a sentinel biopsy, or sentinel lymph node biopsy, can be performed. A radiopharmaceutical or fluorescent dye is injected into the area of the melanoma.
It penetrates the lymphatic vessels and spreads through them to the lymph nodes. The lymph node that receives the dye first is called the sentinel node. It is removed and a biopsy is performed. If malignant cells are found in it, then they most likely have spread to other regional lymph nodes. Sentinel biopsy is especially useful in cases where the melanoma is thicker than 1 mm. It is currently unknown whether a patient can be cured by removing lymph nodes affected by melanoma. At the very least, it helps prolong life and reduce pain and other symptoms.
What should you be wary of?
If you have a large number of moles on your body, be attentive to them and monitor their dynamics. There are five significant signs of melanoma:
- Asymmetrical.
- The edges of dangerous moles become scalloped or jagged (normally they are smooth).
- Uneven coloring or discoloration of a mole.
- Increasing its size (6 mm is already critical).
- Cracks, peeling, bleeding, itching, inflammation.
Even one of the signs listed above should be a reason to immediately consult a doctor.
Palliative surgery for melanoma with metastases
At an early stage, complete removal of melanoma is possible. Even if regional lymph nodes are affected, there is still a chance of remission. If distant metastases are detected, treatment can only be palliative. It aims to relieve symptoms and prolong life, but not to cure. Is there a chance to cure a patient if he only has 1-2 metastases that can be removed surgically? If only one metastasis is found during a CT scan or MRI, most likely there are others, they are just very small and could not be detected. The chances of remission are very low. However, surgical treatment can still help. The surgeon can remove some metastases to improve the functioning of the affected organs, eliminate symptoms, and increase the patient’s life expectancy. In later stages, other, non-surgical treatment methods come to the fore. For example, immunodrugs from the group of checkpoint inhibitors help to greatly increase survival.
Galina, St. Petersburg
Despite the brevity of the text, my gratitude is enormous!
I was in Savonlinna for breast reconstruction surgery. More details Galina, St. Petersburg Tags “Helena Clinic”, Breast reconstruction
Consequences of melanoma removal
Possible consequences of surgical interventions in patients with melanoma:
- Common complications for any surgery: pain, bleeding, risk of infection.
- Relapse is possible. Moreover, melanoma can recur not only in the place where it was before surgery, but also in other organs in the form of metastases.
- After removal of large melanomas, noticeable scars remain. Extensive defects require plastic surgery - transplantation of a skin flap from another part of the body.
- After removal of lymph nodes, some patients experience lymphedema - swelling due to impaired lymph drainage.
How does the procedure work?
No preliminary preparation or equipment is required. The doctor performs an examination and clarifies the diagnosis, after which the patient receives local anesthesia. Treatment lasts no more than five minutes in an outpatient setting.
After using the laser, it is important that no water gets on the wound (at least three weeks). The skin of adults and especially children should be protected from exposure to direct rays of the sun, i.e. Always use sunscreen with a high SPF filter. The results will be visible within a couple of weeks.
Price for melanoma removal in Moscow
The cost depends on many factors: the volume of the operation, studies that the patient may require, the pricing policy of the clinic, experience, qualifications and status of the surgeon, additional treatment methods before and after surgery. We cooperate with the best oncology centers in Moscow, which perform operations to remove melanomas on the back, face and other parts of the body. We will recommend a good clinic where you can get treatment for stage 4 melanoma:
Our doctors
In another case, recognized “Western” experts, including from Israel, will take part in your treatment, specifically on these types of oncological pathologies. Until recently, this level and quality of services were available exclusively abroad, but now you can be treated with the same effect and using the same protocols in Russia. Doctors invited by Dr. Aronov to treat oncodermatology problems at Medis in Moscow:
- Professor Yakov Schechter is the best expert on melanoma in the world, co-author of the drug Keytruda;
- Professor Chaim Gutman is a famous surgeon who periodically comes to Moscow;
- Dr. Alexander Aronov - a famous Israeli doctor in Moscow, diagnostics and immunotherapy;
- Doctors Elmira Gesheva and Marina Biksel are surgeons with “Western” experience in Moscow.
Diagnostics
Doctors use the following diagnostic techniques:
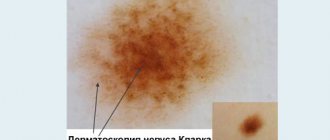
- Dermatoscopy - performed using a special dermatoscope apparatus, allows you to determine changes in the structure of moles at the initial stages;
- Biopsy is the collection of mole tissue for histological examination during radical surgery.
The doctor selects research methods individually after a visual examination, clarification of complaints and history of the development of the disease.
Common process
At this stage, melanoma is difficult to treat. At this time, the tumor has already spread to internal organs and distant lymph nodes. With the 4th degree of spread of the disease, many modern chemotherapy drugs are ineffective; most often, out of hopelessness, dacarbazine and temozolomide are prescribed, using them alone or in combination with other drugs.
If this results in an effect, it usually lasts from 3 to 6 months. After this, the tumor begins to actively grow again. Attempts to increase life expectancy are sometimes achieved through the use of biological vaccines.
For stage 4 melanoma the following is prescribed:
— Temozolid (MTIC) is a derivative of dacarbazine. Its undeniable advantage is the possibility of oral administration, as well as good permeability through the blood-brain barrier. The drug often causes severe side effects.
- drugs based on cytokines . The inclusion of this group of medications, in particular interleukin-2, did not have a significant positive effect on the prognosis of the disease and patient survival. The method of subcutaneous administration of interleukin-2 in small doses does not cause the necessary changes in the immune system, and the use of large doses of the drug provokes a large number of side effects.
- recombinant interferons are usually prescribed as a monotherapy option or in combination with the above medications (dacarbazine, temozolomide, vicristin).
The results of clinical studies in most cases demonstrate the low effectiveness of interferon and even its complete absence. Since advanced pathology is resistant to existing treatment methods, it makes sense to take part in clinical trials of new drugs.
Relapse
Treatment of recurrent pathology depends on the analysis of the tumor gene mutation when it was initially detected, the type of therapy performed, and the location of the relapse. Melanoma usually recurs in the skin near the site of the primary tumor.
Similar to the primary tumor, such local relapses are subjected to surgical therapy. If after the initial treatment the lymph nodes remain unaffected, then in the event of a relapse the disease may affect them. In this case, swelling is noted in the area where they are located. Therapy in such cases consists of lymph node dissection.
Recurrence of melanoma can also develop in all distant organs, most often the brain, lungs, and liver. It is advisable for patients undergoing treatment for relapse to participate in clinical trials of new drugs.
So to whom and when is dermatoscopy indicated?
Let us immediately make a reservation that dermatoscopy is a completely uncomplicated, non-invasive method for the patient, taking a few seconds of time for each neoplasm. There are risk groups in which the likelihood of melanomas is higher and for whom dermatoscopy is indicated necessarily and regularly (usually 1-2 times a year). This:
- Patients who have already had melanoma removed;
- Close blood relatives of people who have been diagnosed with melanoma;
- Patients with multiple (more than 50) clinically atypical nevi, especially if there was a history of histologically confirmed dysplastic nevi.
Patients outside the risk group are advised to have a one-time visit to a dermato-oncologist with an examination of all formations in ALL areas of the skin (including hard-to-reach ones: soles, buttocks, mammary glands, etc.) to assess existing formations. Subsequently, the person independently examines himself at a certain frequency (usually once a month) and turns to a dermato-oncologist only if new or any changes to existing formations appear.