Reasons for the development of bumps on the body
Swellings on the human body can appear for no apparent reason. But basically their occurrence can be associated with processes taking place in the body. The main causes of itchy bumps on the skin are:
- allergic reaction;
- insect bites;
- infection;
- swollen lymph nodes;
- lipomas;
- atheromas;
- folliculitis;
- acne;
- hemangioma;
- precancerous conditions.
The location of the bumps on the body varies and depends on the factor that caused the neoplasm. If the formation causes discomfort, changes color or grows, you should immediately consult a doctor. Treatment is prescribed only after a diagnosis has been established.
Allergy
Bumps often appear on the skin as a result of an allergic reaction to household chemicals, medicines and cosmetics, as well as food. Formations are limited to a certain area of distribution or are of a generalized nature.
An allergy is an inflammatory response of the body to an external aggressive factor. The reaction occurs due to blood cells. The cause of an allergy can always be determined.
The main thing is to avoid repeated contact of a person with the allergen. Each new exacerbation worsens the course of the allergic reaction. Over time, this can lead to swelling of the larynx and difficulty breathing.
Insect bites
In their manifestations, insect bites are similar to skin diseases. Their main symptom is itching. The rashes are single, slightly rising above the surface of the body. But there are also multiple, confluent bumps that envelop the skin.
Most often, a person is bitten by the following insects:
- mosquitoes;
- linen bugs;
- ants;
- flies;
- bees;
- lice;
- ticks.
When the insect bites, it injects poison into the affected area. In small doses, the venom of a blood-sucking insect does not cause physical illness, but acts as a strong allergen. Protecting itself from an aggressive factor, the human body becomes more active and reacts like an allergic response. Red bumps on the skin are a reaction to the toxic factor.
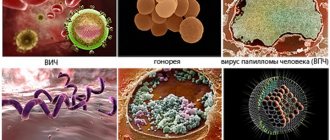
Infection
Bumps and swelling on the skin may be a consequence of an infectious process occurring in the body. Most often the disease is caused by streptococci and staphylococci. It is observed in persons with reduced immunity.
Infectious lumps spread over the entire surface of the body. The formations are soft or elastic to the touch, fused with the surrounding tissues.
The lymph nodes
Enlarged and inflamed lymph nodes are called lymphadenitis. The lymph nodes are the first to respond to the appearance of an infectious factor in the body. They filter the blood plasma, retaining the inflammatory agent. During movement, the lymph nodes can cause discomfort, pain and itching.
It is highly not recommended to treat enlarged lymph nodes with ointments and compresses. This may make the condition worse.
Lipoma
Lipoma is a benign tumor consisting of fat cells, which is separated from healthy tissue by a capsule. Most often, lipomas are of a multiple nature. They cover the body wherever there is adipose tissue.
New growths may be small and not cause any inconvenience. But when inflamed, such a lump itches, and pain occurs when pressed.
Atheroma
When the sebaceous gland is blocked, a brush forms on the skin, which is called atheroma. As the sebaceous secretion accumulates, the cyst grows. The neoplasm is of elastic consistency, mobile, spherical. Suppuration of atheroma leads to independent opening of the contents and a local inflammatory process.
Atheroma can appear anywhere where there is hair. Long-term progression of education leads to transition to a chronic form. Atheroma acquires a bluish tint, thickens, and periodically causes itching and burning.
Folliculitis
Folliculitis is an inflammation of the hair follicle. Most often, single inflammatory foci are observed, but multiple folliculitis also occurs. With multiple lesions, inflammation spreads to the entire skin of a particular part of the body.
The appearance of folliculitis is associated with insufficient personal hygiene. The bump looks like a small elevation above the surface of the skin containing white contents. Chronic folliculitis entails cicatricial deformation of the skin.
Acne
in this gallery In medical practice, acne is called acne. Chronic folliculitis, skin infections, and multiple atheromas lead to the appearance of acne on the skin. Acne appears on the body when immunity decreases and coccal flora activates.
Hormonal levels play a major role in the development of acne. An increase in testosterone levels in the blood leads to increased work of the sebaceous glands and increased secretion. Sebum becomes infected with bacteria found on the surface of the body. As a result of this process, an inflammatory reaction is observed. You can see what acne looks like in this gallery.
Favorite places for acne to appear are the face, back and chest. In severe cases, the rash is confluent in nature. With exacerbation, inflammation, itching and new lesions appear. Chronic inflammation causes scarring on the skin.
Hemangioma
One of the reasons for the development of a red bump on the skin is hemangioma. The neoplasm occurs in 80% of cases in children in the first days of life, but can be observed at any age.
Hemangioma is a benign neoplasm consisting of vascular tissue. This condition occurs due to disruption of vascular development during intrauterine anlage.
From the moment of its development, hemangioma is characterized by rapid growth and germination into the underlying tissue. Then growth stops and stabilization occurs. Subsequently, tumor reduction is observed until it disappears. In rare cases, formation requires additional treatment.
Precancer
It happens that the appearance of bumps on the body becomes the first sign of a malignant neoplasm. Initially, the tumor-like structure does not cause symptoms. With prolonged exposure to the body, the structure of the cells changes. There is a transition from a benign form to a transitional one, the so-called precancer.
Precancer is a congenital or acquired change in healthy tissue, which can subsequently lead to the development of malignancy. Transitional forms of neoplasms first manifest themselves as a change in color to a darker color, as well as ulceration and itching. The longer the altered tissue exists on the body, the greater the likelihood of a malignant process.
Causes and methods of treating bumps between the phalanges of the fingers
The appearance of bumps on the fingers and subsequent deformation of the terminal phalanx of the finger is a consequence of diseases of the musculoskeletal system. In each specific case, the doctor makes an accurate diagnosis, but in most cases there are two main reasons for the formation of lumps.
For what reason does the disease develop?
The first reason is arthrosis of the joint, which causes inflammation in it. It is inherited and develops due to disruption of metabolic processes in the body, decreased immunity, and hypothermia. The second reason is arthritis. It causes damage to the cartilage in the joint. Healthy cartilage is always smooth, bones slide over it easily without causing pain. If for some reason a metabolic disorder occurs in the body, a joint injury occurs and an infection occurs, autoimmune diseases arise, then this can cause wear and tear of the cartilage, in other words, the development of arthritis. It is worth understanding that a bone growth on the finger is just a side effect of the diseases mentioned. That is, with arthritis or arthrosis, the appearance of cones is possible, but not necessary. There are other reasons why formations appear on the phalanges of the fingers. These include:
- Work that places prolonged stress on the phalanges of the fingers. The range of such work is very wide - from bricklaying to professional piano playing.
- Hygroma, which is a chamber filled with a gel-like liquid. To the touch it is an elastic formation that does not cause pain. It is better to refrain from self-punctures to remove fluid. After such self-medication, the hygroma forms again.
- Fibroma. This problem occurs very rarely and is associated with pinched nerve endings.
- Skin cancer or sarcoma.
- In women, menopause.
You should not hesitate to consult a doctor if alarming symptoms begin to appear in your finger work - crunching or painful sensations when flexing/extending the phalanges.
Typical signs of disease development
The first symptoms of this disease may resemble simple irritations. These include: redness of the skin on the joint with the appearance of a tumor; the inflammatory process in the joint, like any other part of the body, causes an increase in the content of leukocytes in the blood. But the following signs give cause for concern:
- Pain caused by finger movement.
- The need to make extra effort to bend or straighten the finger.
- Beginning of lump formation.
In addition, a decrease in the number of lymphocytes in the patient’s blood can be a warning signal about the development of the disease. These are cells that support the immune system. If there are fewer of them, the likelihood of infections entering the body increases, which can cause arthritis. It has already been mentioned that this is one of the possible reasons for the appearance of bumps. If a patient exhibits at least some of these symptoms, it would be wise to undergo testing.
Diagnosis of finger joint seals
During the first visit with a complaint about such symptoms, a rheumatologist will examine the affected area and take an anamnesis. Sometimes this is enough to accurately determine the cause of pain in the phalanges of the fingers. In other cases, it may be necessary to take a puncture, do an x-ray or magnetic resonance imaging. To verify the presence or absence of a malignant tumor, histology of the lump tissue is prescribed. For this, a biopsy is used.
Treatment of bone formations
Each patient is prescribed his own therapy. But it is still possible to define general methods. In turn, they are distributed for treatment with drugs, traditional medicine, and prevention. The group of drugs includes the following drugs:
- Painkillers.
- Anti-inflammatory action.
- Hormonal.
- Chondroprotectors.
- Vitamins.
Despite the abundance of treatment methods in traditional medicine, you need to exercise caution and consult your doctor before using them. You need to understand that traditional medicine does not replace scientific medicine, but only complements it. Among these additions are the following:
- Mustard powder is mixed with camphor oil. Take 50 grams of both ingredients. Whites from two chicken eggs are added to them, and this entire mixture is diluted with 70% alcohol until a homogeneous mass is formed. The finished medicine is applied in a thin layer to the sore spot and wrapped in a clean piece of natural material. The bandage is not removed for two hours, and the interval between procedures should not exceed four days.
- Squeeze out as much juice as possible from pre-chopped garlic, moisten a clean piece of natural cloth with it and wrap it around the bone growth. Repeat the procedure for a week.
- Dip a fresh cabbage leaf into boiling water, then pull it out and spread it with liquid honey. Coat the bones on your fingers and wrap with cling film. Continue treatment for two weeks and apply the bandage at night.
- Celandine oil can save you from severe pain. This drug is purchased at a pharmacy or obtained by manual processing of the plant. To do this, pass celandine through a meat grinder and infuse the pulp in vegetable oil. This method is not applicable for patients suffering from allergies.
In case of hygroma formation, similar treatment methods are taken.
Apply cabbage leaves or make lotions from celandine juice. The sore spot is steamed in salt water, smeared with honey, and wrapped in woolen cloth. Honey and peeled aloe are added to rye flour. This paste is applied to the sore spot overnight. Before using any type of traditional medicine treatment, you must agree with your doctor. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Erythema nodosum - symptoms and treatment
Erythema nodosum is an inflammation of the subcutaneous fat, which is accompanied by the appearance of painful, palpable red or purple subcutaneous nodules. Most often they appear on the legs, sometimes in other areas.
This disease is caused by an increased immune response of the body to the pathogen [1][3]. Despite numerous studies of this pathology, the causes of erythema nodosum and the mechanism of its development have not been sufficiently studied. However, there is a theory that the main cause of erythema nodosum may be various infectious diseases.
Table 1. Causes of erythema nodosum.
| Main reasons | Diseases that may cause erythema nodosum | Other |
| — B-hemolytic streptococcus of group A — Tuberculosis bacillus — Chlamydia — Hepatitis B and C — Herpesvirus family — Various fungi — Protozoa — Lymphogranuloma venereum — Psittacosis — Measles — Cat scratch disease — HIV, etc. | — Sarcoidosis — Ulcerative colitis — Regional ileitis — Hodgkin's disease (Hodgkin's lymphoma) — Lymphosarcoma — Leukemia — Rheumatoid arthritis — Behcet's disease — Malignant neoplasms — Chronic hepatitis — Ankylosing spondylitis — Granulomatous mastitis — Takayasu's arteritis — Vogt's disease — Koyanagi — Granuloma Wegener's ematosis - APS syndrome - Systemic lupus erythematosus, etc. | — Taking medications: sulfonamides, bromides, clomiphene, codeine, co-trimoxazole, D-penicillamine, dapsone, diclofenac, dicloxacillin, estrogens, ibuprofen, indomethacin, interleukin-2, etc. — Pregnancy — Jellyfish burns — Smoke inhalation in firefighters and etc. |
Risk factors for the appearance of erythema nodosum include fungal diseases, inflammatory diseases of the gastrointestinal tract, hormonal imbalances, tuberculosis, and taking various medications [2]
An important role is played by provoking factors , such as climate change, transitional seasons, stress, temperature changes (hypothermia), varicose veins of the lower extremities, etc. The disease is seasonal, usually appears in early spring and late autumn, which is due to frequent colds, sore throats, and decreased immunity.
The incidence of erythema nodosum in different countries can vary from 1 to 5 cases per 100,000 population per year [12]. This depends on the prevalence of diseases that can cause erythema nodosum in a particular area. Mostly, erythema nodosum is detected in people 20-30 years old [2][12]. It is at this age that a person first encounters many infections.
Women who have the HLA B8 gene are more susceptible to erythema nodosum, which may confirm the fact of a hereditary predisposition to this disease [4]. HLA (Human Leukocyte Antigen - human leukocyte antigen) is responsible for recognizing foreign cells and activating the immune response to them. When this mechanism is triggered, we see a clinical picture of inflammation, which is caused by the reaction of the immune system.
It is known that HLA B8 is associated with several groups of diseases, including erythema nodosum. And it is so programmed that it occurs more often in women [11]. This is why women get sick much more often than men (about 3-6 times) [12]. If we do not take into account changes in the genome, then erythema nodosum occurs proportionally equally in men and women, since they are equally susceptible to streptococcal infections and other diseases.
Erythema nodosum is more often detected in the European population, particularly in Scandinavia, while it is rarely diagnosed in Asians, since the HLA B8 gene is almost never found in them [11][13].