Fungal external otitis is successfully treated in ENT clinic No. 1
Author:
- Golonova Yulia Yurievna
otorhinolaryngologist, clinic director
4.00 (Votes: 5)
The problem of fungal infection of the external auditory canal (otomycosis) is growing every decade. This is due to the problem of decreased immunity, frequent and uncontrolled use of antibiotic therapy, and the dietary habits of modern humans, who consume large quantities of food rich in carbohydrates, often leading to type 2 diabetes mellitus and increased blood glucose levels. All these reasons lead to an increased risk of developing fungal infections, including in the ear canal.
If we add to the overall picture the bad habit of “cleaning” or “scratching” the ears with all available objects, naturally non-sterile (including the so-called “ear” sticks, which are also non-sterile), which helps remove the natural protective factor from the ear canal - earwax and contaminated with all conceivable and inconceivable bacterial and fungal microflora - we get ideal soil for the formation of otomycosis.
Causes of hearing diseases
There are many causes of fungal infection of the ear canal, but the main one is the presence of saprophytic or conditionally pathogenic flora on the skin or mucous membranes of the body.
These microorganisms do not lead to the development of symptoms of the disease in a healthy person, but when exposed to unfavorable factors they can become more active. These reasons include:
- Low level of hygiene - when the ears are dirty, the natural balance of the skin of the external auditory canal is disrupted and favorable conditions are created for the proliferation of microorganisms.
- Foreign body - the presence of foreign objects in the ear canal, which is most often observed in children, can also lead to an inflammatory process.
- Injury to the eardrum or mucous membrane when cleaning the ears with a cotton swab leads to the formation of microcracks and wounds, which are entry points for infection.
- Associated diseases and conditions. Congenital or acquired decreased immunity due to HIV/AIDS, cancer, diabetes mellitus, allergic rhinitis, dermatitis of any etiology can lead to mycosis of the ears.
- Taking certain medications, namely hormonal and cytostatic drugs, long-term or unsystematic antibiotic therapy can also affect the state of the immune system and provoke fungus in a person’s ears.
- Physiological characteristics of the hearing organs, namely a narrow ear canal, exostoses.
- Exposure to environmental factors, such as hot or humid climates, contact with chemical agents, ionizing radiation.
- Other reasons are hyperhidrosis, using someone else's headphones or earplugs.
Find out more
OTOMYCOSIS in childhood
V. R. Chistyakova, Doctor of Medical Sciences, Professor I. V. Naumova Russian Children's Clinical Hospital, Moscow
The frequency of infectious and inflammatory diseases caused by fungi has been steadily increasing in recent years. At the same time, mycotic damage to the ENT organs in children has increased sharply, and the frequency of oropharyngeal candidiasis and otomycosis has especially increased
Fungal diseases of the ENT organs are more common in children than in adults, which is largely due to dysbacteriosis in childhood, as well as various factors that weaken the reactivity of the child’s body. The proportion of mycotic (opportunistic) infection in chronic pathology in children is quite high and has been progressively increasing in recent years.
According to ES Beneke, AJ Rogere (1970), R.N. Rebrova (1970), otomycosis accounts for 10% of all inflammatory diseases of the ears; according to O. K. Khmelnitsky (1973) - 18%, V. Ya. Kunelskaya (1976) - 18.9%, N. D. Chelidze (1984) - 26.3%, Mohammad Shafuil Alam (1986) - 18 %, S. A. Pavlenko (1989) - 37.8%, E. V. Pronina (1996) - 15%.
G. A. Samsygina and co-authors (1996) over 20 years of observation noted an increase in candidiasis in newborns and infants from 1.9% to 15.1%. Moreover, in 40-60% of cases the disease remains unrecognized, late diagnosed and inadequately treated, which significantly worsens its prognosis.
An increase in the incidence of mycoses, infection and superinfection with fungi often contribute to the transition of acute processes into chronic ones, the occurrence of relapses and a more severe course of the disease. Irrational treatment can lead to the generalization of a fungal infection, which is especially severe.
During 1993-1997, the ENT department of the Republican Children's Clinical Hospital treated 305 children with inflammatory ear diseases. Of these, 85 people (27.9%) had otomycosis. In addition, 32 children were treated on an outpatient basis: 16 with mycotic dermatitis of the external auditory canal and 16 with secondary otomycosis, which complicated the course of recurrent otitis media. Thus, under our supervision there were 117 patients with otomycosis from various regions of Russia. The largest number of children (52) were from Moscow and the Moscow region, which was due to a higher level of diagnosis and verification of mycotic infection.
In all children, otomycosis occurred secondarily, complicating the course of the disease of the external and middle ear. The main forms of mycotic damage to the ear were: dermatitis of the external auditory canal, recurrent and chronic otitis media, damage to the postoperative cavities of the middle ear.
The occurrence of otomycosis in children was preceded by repeated long-term use of broad-spectrum antibiotics (often the latest generation), local use of glucocorticoid drugs, especially in young children with recurrent otitis media (frequent use of Sofradex, transmeatotympanic injection of antibiotics with glucocorticoids), cytostatic and radiation therapy.
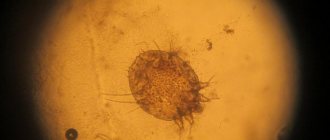
| Figure 1. Total fungal infection of the outer and middle ear against the background of systemic candidiasis and mycotic lesions of the scalp in a 6-month-old child |
Factors such as prematurity, immaturity, early transfer to artificial feeding, intestinal dysbiosis, immunosuppressive therapy, and long-term resuscitation measures are also important. The role of an allergic background, pathology of the gastrointestinal tract and endocrine system, especially diabetes mellitus, blood diseases, and immunodeficiency was noted. All children were found to have a profound disorder of intestinal microbiocenosis.
Persistent otorrhea, not amenable to conservative treatment, indicated the activity and severity of the purulent-inflammatory process in the middle ear, which was the basis for conducting a thorough special microbiological study.
We carried out a comprehensive examination, including a targeted mycological study of the pathological discharge, including microscopy of native and Romanovsky-Giemsa-stained preparations and cultural diagnostics with inoculation on Sabouraud and Chanek’s medium. Microscopy of an unstained specimen revealed fungi in 78% of patients, and of a stained specimen - in 100%. Species identification of fungi of the genus Candida was determined based on biochemical characteristics. When inoculating on nutrient media, uniform growth of fungi at all points was observed in all patients.
Comparative data on the frequency of various forms of otomycosis in terms of age are given in table. 1. The largest number of patients had mycotic otitis media, 12 of them had mastoiditis. Moreover, secondary otomycosis predominated, complicating the course of chronic otitis (15.4%), less often it occurred with recurrent otitis media in young children (12%). Mycosis of the postoperative cavity of the middle ear was observed in 35 children. Mycotic lesions of the external auditory canal were diagnosed in 27.4% of cases. School-age children predominated. The vast majority of them had chronic otitis media, including mycotic lesions of the postoperative middle ear cavity in 42 patients. External otitis in this age group was observed in 22 children. In toddlers, otomycosis mainly complicated the course of recurrent otitis media.
Table 1. Comparative data of various forms of otomycosis in the age aspect
| Age | Clinical forms of otomycosis | Total | |||
| Mycotic dermatitis of the external auditory canal | Mycotic recurrent | Average chronic | Otitis of the postoperative cavity | ||
| 7 months - 1 year | 2 | 16 | 4 | — | 22 (18,8%) |
| 5-7 years | 5 | — | 7 | 8 | 20 (17%) |
| 8-10 years | 15 | — | 9 | 15 | 39 (33,4%) |
| 11-14 years old | 9 | — | 8 | 19 | 36 (30,8%) |
| Total | 31 (27,4%) | 16 (12%) | 28 (15,4%) | 42 (35%) | 117 |
Analysis of clinical and anamnestic data made it possible to identify some features of the development and course of the pathological process in children.
All children were admitted in a state of moderate or severe severity after long-term and unsuccessful treatment at the place of residence. The severity of the condition was determined by the age of the child, the degree of spread of the mycotic process, generalization, the depth of destructive changes in the temporal bone and the nature of complications. In 12 cases, the reason for urgent hospitalization was mastoiditis, which complicated the course of otomycosis.
During mycological examination, candidiasis was most often detected (64.8%); aspergillosis occurred in 21%, penicillosis in 12.5%. In two children, mucorosis was detected during surgery (1.7%).
The majority of children (52%) have chronic disseminated candidiasis with simultaneous lesions of the tonsils, pharynx, tongue, external and middle ear, paranasal sinuses: oropharyngeal candidiasis in 22 patients, mycotic stomatitis in five, candidal glossitis with necrosis of the epithelium of the tongue to the basal layer of the epidermis - in three children, mycotic sinusitis - in three patients.
Systemic candidiasis with simultaneous damage to the genitourinary system and digestive tract was observed in the vast majority of children and had the character of intestinal dysbiosis, biliary dyskinesia, metabolic nephropathy, recurrent urethritis and cystitis in boys and vulvovaginitis in girls. Of the concomitant diseases, five children had diabetes mellitus, 13 had blood diseases, two had genetic syndromes (Fox–Forsythe, Lyell), 15 had vegetative-vascular dystonia and other neurological pathology. All children were diagnosed with profound dysbiotic intestinal disorders caused by a deficiency of bifidobacteria and the presence of associations of opportunistic microorganisms (hemolysing Escherichia, staphylococci, hemolytic streptococci, Klebsiella, Proteus, Candida). A deficiency of bifido- and other lactic acid bacteria leads to the unhindered colonization of opportunistic microflora, primarily fungi, not only of the intestines, but also of other body cavities in contact with the external environment (mouth, nose, ears). This requires the inclusion in the complex of therapy of biologically active drugs that normalize the intestinal microflora.
| Timely mycological research with individual selection of antifungal drugs of general and local action, along with restoration of intestinal microbiocenosis and correction of interferon status, increases the effectiveness of therapeutic measures for otomycosis in children |
The vast majority of patients applied late in the development of the disease. In our observations, in 66 patients, the duration of the disease with otomycosis exceeded three years, while at first the disease was asymptomatic. Despite long-term outpatient treatment, only 37 children were constantly observed by an otolaryngologist.
A feature of the course of the disease in them was persistently recurrent suppuration from the ear, dermatitis of the external auditory canal, and resistance to traditional methods of treatment. Mycotic lesions of the ears in these observations were secondary and occurred against the background of recurrent or chronic inflammation.
Among the main symptoms of the disease in these children were recurrent suppuration, itching in the ear canal, a feeling of fullness and stuffiness in the ear, headache, and fever (hyperthermia in mastoiditis). Even with total osteomyelitic lesions of the middle ear, there were no typical clinical features, with the exception of torpidity of the course and the ineffectiveness of conventional antibacterial therapy. Also common to all forms of otomycosis was a certain cyclical exacerbation of the process in the ear, a constant aching dull pain that intensifies with exacerbation and an increase in discharge, maceration of the skin of the ear canals.
Along with this, there were some features of the otoscopic picture caused by the mycotic process. Aspergillosis is characterized by the phenomena of granulation myringitis, pronounced maceration of the skin and narrowing of the ear canal, discharge in the form of films and plugs of black, brown or white color (resembling rolled paper), a more pronounced decrease in conductive hearing with an increase in air thresholds over the entire frequency range up to 20 -25 dB.
Penicillinosis proceeded most easily and was manifested by scanty mucous discharge, the formation of crusts, and preserved hearing.
| All forms of otomycosis are characterized by cyclical exacerbation of the process, constant dull aching pain in the ear, maceration of the skin of the ear canals |
With candidiasis, the reaction of the skin of the external auditory canal is most pronounced, with a transition to the auricle and the development of eczema-like lesions and even chondroperechondritis of the auricle, followed by severe deformation; curd-like or liquid discharge, formation of multiple perforations of the eardrum, slight (up to 10 dB) hearing loss.
Mucorosis is very dangerous, as it is accompanied by lymphangitis and thrombosis of surrounding vessels with the spread of inflammation into the cranial cavity and high mortality.
Indications for surgery were: mastoiditis, which complicated the course of otitis due to mycosis; chronic cholesteatoma process in patients with secondary otomycosis; untreatable otomycosis of the postoperative cavity of the middle ear.
During the operation, as a rule, gross mycotic changes were revealed in the area of the mastoid process (mainly in the area of its apex and the Citelli angle) in the form of rounded areas of black-green fungal growth, total osteoperiostitis of the entire cellular structure of the mastoid process, excessive growth of granulations and polyps, caseosis
Postoperative cavities were carried out using the open method using general and local antifungal agents and MAG films (adsorbing hydrophilic polymer material) with dioxidin and propolis. Suturing of a postoperative fistula in the postauricular area was performed no earlier than a year after surgical treatment with a triple negative mycotic study.
Mycotic changes in the middle ear identified during surgery allow us to recommend expanding the indications for surgical intervention in children with long-term, often recurrent mycotic lesions.
Currently, the tactics of treating otomycosis have changed significantly: the main principle is a differentiated choice of complex treatment based on the obtained mycogram, including antifungal drugs of general and local action, correction of interferon status and dysmetabolic disorders, correction of intestinal biocenosis.
Among antifungal agents, the most appropriate is the use of triazole compounds of the ketonazole, fluconazole and intraconazole series. These drugs block the synthesis of ergosterol in the fungal membrane, providing an active fungicidal effect. These include: diflucan, orutal, nizoral, amphoglucamine, amphotericin, amphomoronal, mycoheptin. When prescribing ketonazole drugs, we necessarily took into account their incompatibility with second-generation peripheral H1-histamine receptor inhibitors and macrolide antibiotics. This combination causes a prolongation of the QT interval on the ECG with the possible development of rhythm and conduction disturbances. The use of nystatin and levorin orally is not advisable, since they are not absorbed through the intestinal wall and are ineffective when applied topically.
Local treatment of otomycosis includes a thorough toilet of the ear, since even with a small amount of mycotic masses, the therapy will be ineffective. There are many drugs for local treatment (resorcinol, quinozol, tannin in glycerin). We recommend the use of triazole compounds in the form of ointments and lotions, such as travogen, pevaril, nizoral, baykuten, on turundas for a month, taking into account the mycogram.
The therapeutic complex necessarily includes biologically active drugs that restore intestinal microbiocenosis, lasting from three weeks to three months: acipol, bactisubtil, bifidumbacterin, bificol, lactobacterin, colibacterin, proteus phage, hilak forte, primatofilus, linex. With the 4th degree of dysbiosis, antibiotics are prescribed to suppress intestinal infection.
Along with antifungal drugs, agents that accelerate regeneration processes and inducers of local interferon were also used in operated patients.
We conducted a study of interferon status in 20 patients, since during the course of mycosis in the child’s body, changes in general and local immunological reactivity, including its interferon component, occur. All children examined were found to have a defective interferon system, which was the rationale for including interferon replacement therapy in the treatment complex. Treatment was carried out according to the following scheme: Viferon-250 in children under 7 years of age and Viferon-500 in children over 7 years of age, two suppositories every 12 hours for 10 days and then one suppository twice a day three times a week for three months . For local treatment, a natural interferon inducer, megasyn, was used on an ointment basis.
As a result of the monitoring, the feasibility and high efficiency of using interferon inducers (gene-interferon drug Viferon) in the complex treatment of otomycosis in children to correct interferon status was proven.
The use of drugs that optimize energy metabolism, such as lipoic acid, pantothenic acid, limontar, Wobenzym, and B vitamins, indirectly helped to correct the impaired immune status.
We managed to achieve a positive effect in all the patients we observed. The criteria for cure were the complete cessation of suppuration from the ear and the absence of relapses within a year, achieving complete epidermization of the postoperative cavity.
References
1. Mohammed Shafuil Alam. Clinic, diagnosis and treatment of otomycosis in Bangladesh. Abstract, Ph.D. dis. M., 1986. 2. Pavlenko S. A. Otomycoses in Kuzbass and organization of specialized care. Abstract, Ph.D. dis. M., 1989. 3. Kunelskaya V. Ya. Otomycoses. M., 1976. 4. Pronina E. V. Visceral and systemic forms of candidiasis in young children. Abstract, Dr. dis. St. Petersburg, 1996. 5. Rebrova R. N. Mushrooms of the genus Candida. M., 1970. 6. Samsygina G. A., Buslaeva G. N., Kornyushin M. A. Diflucan in the treatment and prevention of candidiasis. Pediatrics named after Speransky. Supplement, 1996. 7. Khmelnitsky O.K. Histological diagnosis of superficial and deep mycoses. L., 1973. 8. Chelidze N. D. Otomycosis in childhood. Author's abstract. Ph.D. dis. 1984. 9. Beneke ES, Roger AJ Tropical Otomycosis, J. Laryng. 1970, 81, 9, 487-999.
Symptoms of ear fungus
Symptoms of ear fungus vary; at first, the disease may be asymptomatic or manifest itself as mild itching in the ears. For early diagnosis and effective treatment, it is important not to miss the disease in its early stages of development and take into account all the symptoms. Otomycosis can also cause the following complaints in patients:
- Ear congestion, itching and peeling of the skin are the primary signs of an inflammatory process of any etiology; with external ear fungus, these symptoms are pronounced and lead to a significant deterioration in the patient’s condition.
- Patients also experience severe pain, swelling and hyperemia of the skin and mucous membranes.
- Inflammation leads to the formation of discharge, which can be either minor serous or profuse purulent, or specific, characteristic of a particular pathogen.
- With fungal myringitis (inflammation of the eardrum), patients may experience a sensation of a foreign body in the ear, a feeling of fullness. Prolonged course of the disease can lead to tinnitus, hearing loss, dizziness and local or systemic complications.
Otomycosis can be complicated by inflammation of regional lymph nodes, the upper jaw joint, mastoid process, and mastoiditis. In patients with concomitant infectious diseases or decreased immunity, fungus in the ear canal can lead to systemic mycoses.
What should you be afraid of with otomycosis?
Fungal external otitis tends to chronicize the process, forming a sluggish, constantly persistent process of fungal inflammation. In this case, an increase in symptoms is provoked either by antibiotic therapy or changes in diet: an abundance of “fast” sugars - when the mushrooms begin to grow “by leaps and bounds.”
A long-term fungal process leads to sensitization (allergization) of the body, decreased immunity, and the presence of itching often leads to scratching and the risk of secondary purulent infection.
Classification of the disease
Fungal infections of the hearing organs are classified depending on the pathogen, the course of the disease, and the site of inflammation. Depending on the duration of the disease, there are:
- acute otomycosis (lasting less than 1 month),
- subacute (from 1 to 6 months),
- chronic (lasts more than six months).
Chronic fungal otitis occurs with improper or untimely treatment of an acute process, decreased immunity, concomitant diseases and injuries.
This pathology is difficult to treat with conventional antifungal agents and most often occurs with exacerbations and relapses of the disease.
The classification of the disease also distinguishes the following forms: otitis externa, myringitis (inflammation of the eardrum), otitis media and internal, as well as otitis of the postoperative cavity.
Postoperative otitis may occur due to fungal spores getting into the wound during or after surgery, namely mastoidectomy.
Frequent complaints of patients with this pathology are significant discharge from the external auditory canal and pain behind the ear. This type of otomycosis is characterized by a long course due to a decrease in the body’s resistance after surgery, and the occurrence of insensitivity to drugs due to antibiotic therapy.
Types of ear fungus
Based on etiology, fungal diseases of the hearing organs are divided into:
- Ear aspergillosis caused by mold fungi of the genus Aspergillus, Penicillum.
- Candidiasis of the ear, caused by fungi of the genus Candida, most often Candida albicans.
- Actinomycosis caused by actinomycetes fungi.
- Other types of mycoses are mucoidosis, coccidioidosis, cryptococcosis, blastomycosis.
- A combination of fungal infection with bacterial or viral-bacterial associations.
The most common are aspergillosis and candidiasis of the auditory organs; these diseases have their own specific signs, with the help of which the disease can be diagnosed in time and the correct treatment can be prescribed.
Aspergillosis is characterized by the presence of dark gray or greenish discharge from the external auditory canal, plaque on its wall, which is difficult to remove. After removing the plaque, wounds with a bleeding surface often remain.
There is also swelling of the walls of the passage, the spread of inflammation to the eardrum, its thickening and hyperemia. This leads to significant hearing loss during the course of the disease.
With the development of candidiasis, the discharge is insignificant, light yellow in color, reminiscent of earwax. Characterized by eczematous rashes with serous or purulent contents on the skin of the external auditory canal.
Inflammation also spreads to the cartilage tissue, which can lead to deformation of the outer ear.
Can there be complications?
Complications from ear mycosis are possible if treatment was started untimely or incorrectly. The disease can lead to damage to the hearing aid or become chronic with periods of exacerbation. The following complications are possible against the background of the disease:
- purulent otitis, severe pain and pus discharge;
- the spread of mycosis can spread to the face, neck and other parts of the body.
- intoxication of the body, characterized by fever and muscle pain.
If the treatment does not have the desired effect and complications begin, you need to contact an otolaryngologist, who will help you choose the appropriate medications and prescribe additional tests if necessary.
Methods for diagnosing ear fungus
Diagnosis of otomycosis includes general clinical tests (complete blood count, urinalysis, blood glucose) and special studies. These include:
- Otoscopy is an examination of the outer ear using an otoscope. Signs of fungal otitis are redness and swelling of the walls of the ear canal, its narrowing, and discharge from the ear.
- For bacteriological and mycological studies, material is collected - secretions from the ear canal. Using a microscopic examination, you can detect mycelium or spores of fungi and determine its genus. Sowing the material on nutrient media, or mycological examination makes it possible to find out the type of pathogen and its sensitivity to antifungal drugs.
Treatment of ear fungus
Treatment of fungus in the ears should be comprehensive and directly affect the cause of the disease. First of all, it is necessary to identify the factors that influenced the occurrence of otomycosis and eliminate them.
The treatment regimen also includes a rational diet, vitamin therapy, dosed physical activity, and herbal medicine. Drug treatment consists of etiotropic, affecting the pathogen, and symptomatic.
Antifungal drugs are used for mycoses of any localization; for ear fungus, local drugs in drops, ointments, and solutions are most often used.
Before using medications, you need to clean the ear canal of secretions and earwax. You can rinse the ear canal with antiseptic solutions or hydrogen peroxide.
Before instilling the medicine into the ear canal, the bottle must be warmed, the auricle must be pulled back and up for adults, for children under 5 years old - down and back to align the ear canal.
Systemic agents are prescribed for chronic otitis media, serious condition of the patient, and concomitant diseases. Symptomatic drugs are used for pain relief when the temperature rises and additional symptoms occur.
Additionally, the treatment regimen for ear mycosis includes pro- and prebiotics for the treatment of intestinal dysbiosis, desensitizing drugs, immunocorrectors, and vitamins.
For additional treatment of otitis, folk remedies are used, for example, celandine infusion, onion or garlic juice, walnut oil, propolis infusion, decoctions of chamomile flowers, bay leaves and bird cherry leaves, warming the outer ear with dry heat.
It must be remembered that treatment only with folk remedies, without the use of antifungal drugs, is unacceptable.
Prevention of ear fungus
Prevention of otomycosis consists of the following techniques:
- Maintaining a healthy lifestyle, hardening, avoiding hypothermia.
- Timely treatment of diseases of the ENT organs and other chronic diseases, improvement of immunity.
- Maintain personal hygiene, clean the ear canal, treat small wounds with antiseptic agents.
- Take antibiotics and hormonal medications only as prescribed by a doctor.
- Protecting the ear canal cavity from water ingress when swimming.
Disease prevention measures
To prevent the occurrence of fungal infections of the ears, you should adhere to basic preventive measures:
- Do not injure the ear canal.
- Do not touch your ears with dirty hands.
- Avoid deep cleaning of the ear canal with cotton swabs; they should only be used for cleaning outside the hole.
- Do not self-medicate by taking antibiotics unnecessarily.
- Promptly treat concomitant diseases that can worsen immunity.
- Undergoes preventive examinations with an otolaryngologist.
- Do not use headphones from strangers.
- When swimming in open waters and pools, if possible, wear earplugs.