The epidemiology (prevalence) of tongue cancer is on average 5 cases per 100 thousand population.
Among the recorded cases of oral tumors, it accounts for up to 60%. Despite the relatively simple diagnosis of this disease, there are advanced cases - people often do not notice the signs or ignore the symptoms of tongue cancer.
What is glossitis?
Glossitis (from the Greek glossa (tongue) + suffix –itis) is an inflammation of the tongue. The reasons for its occurrence are different. Glossitis can develop as a result of a viral or bacterial infection, or as a result of another disease in the body. In addition, there are some other factors that provoke the development of the disease. These include mechanical, chemical and thermal damage to the oral cavity; nicotine; food that is too spicy or too hot; alcohol; caramel; some components present in toothpastes.
Glossitis has the following forms:
- folded
- diamond-shaped median
- desquamative
- hairy black
- Gunter's
- interstitial
According to the duration of the inflammatory process, acute and chronic glossitis are distinguished. The acute form of glossitis manifests itself as inflammation of the tongue, a change in its structure or color. Symptoms of the chronic form are more varied, but in most cases the disease is diagnosed by the presence or absence of papillomas - fungal growths on the tissues of the tongue. There are cases when the cause of the disease can be identified only after comprehensive medical research. True, this happens quite rarely and, as a rule, is associated with the presence of congenital, hereditary diseases.
Etiology - causes of tongue cancer
The main cause of tumors on the tongue, like any other cancer, is a genetic malfunction in the cells.
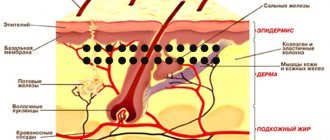
In this case, these are epithelial cells - the tissue that forms the mucosa. Several main factors contributing to this process have been identified:
- Exposure to carcinogens. A huge amount of harmful substances is contained in cigarette smoke and chewing mixtures (nasvay, betel). It is in smokers and nasal users that cancer of this localization is most often diagnosed, and in men it is detected 3 times more often than in women. Alcohol increases the impact of carcinogens.
- Occupational hazards. The incidence of tongue cancer in people employed in hazardous industries is much higher. Salts of heavy metals (mercury, lead), asbestos, and petroleum products can also be classified as carcinogens by their nature.
- Photo: neoplasm on the tongue
Impact of viruses. Recent studies have proven a direct link between chronic viral infection and the incidence of cancer. Human papillomavirus, herpes simplex virus and HIV are capable of transforming the genome of cells, turning them into cancerous ones. According to statistics, up to 70% of women are carriers of HPV. The mechanism of oncogenic effects of viruses is associated with their ability to suppress antitumor genes.
- Chronic oral injuries. They may be associated with improper installation of dentures, improper treatment of fillings, or chronic biting of the mucous membrane.
Long-term exposure to these factors on the mucosa is accompanied by damage to the DNA structure of epithelial cells. As a result, papillary hyperplasia (excessive growth) develops, which looks like a thickening at the sides, or dysplasia (improper development) of the mucous membrane.
Further exposure to these causes leads to the development of precancerous conditions: leukoplakia, Bowen's disease, hyperkeratosis and papillomas. Subsequently, these conditions transform into oncology.
Main symptoms of glossitis
Glossitis, the symptoms of which are very diverse and largely depend on the cause of the disease and the stage of development of the process, but the following signs are almost always present:
- coating on tongue uneven with spots
- ulcers in the oral cavity of varying depth and extent
- color changes (general or in the form of local spots)
- swelling of the tongue, the presence of “imprints” of teeth on its lateral surfaces and other sores
- limited tongue mobility
- bad breath problem
- salivation disorder
Often these changes are accompanied by a decrease in taste sensitivity, a burning sensation and pain at the slightest movements of the tongue while eating and when talking. Sometimes, as the inflammatory process progresses, there is a deterioration in general health: an increase in temperature, enlargement of the submandibular and cervical lymph nodes.
Sialadenitis
This is an inflammation of the salivary glands, which is most often caused by infection. Children and the elderly are more often affected by the disease. The rash usually appears on the salivary glands, but can also affect the root of the tongue. They look like multiple white bumps. At the beginning of the disease, the patient may not experience any discomfort. But then there is pain in the neck, fever and deterioration in general health. Bumps on the base of the tongue and on the salivary glands often fester.
Sialadenitis is a rather dangerous disease. Without treatment, stones form in the salivary glands. It becomes difficult for a person to eat because he has poor saliva production. In advanced cases, the infection can spread to the brain, leading to meningitis.
Types of disease
Depending on the prevalence of the process and the predominance of a certain nature of changes, the following are distinguished:
Catarrhal glossitis
It is manifested by swelling, redness of the tongue, and the appearance of plaque on its surface, but the process does not extend to its deeper layers. Most often, catarrhal glossitis occurs with superficial injuries and burns of the tongue (chemical, thermal), oral candidiasis (disturbance of the balance of normal microflora), various forms of stomatitis, infectious diseases (viral and bacterial nature), as well as with a number of diseases (anemia, hypovitaminosis , metabolic disorders, diseases of the digestive system, etc.).
Ulcerative glossitis
It is usually manifested by the formation of single or multiple small ulcers on the tongue (the so-called aphthae, hence another name for it - aphthous glossitis). Ulcerations are often accompanied by bleeding, severe swelling, severe pain and deterioration in general condition. This type of glossitis can develop from catarrhal glossitis, and also be a manifestation of diseases of the oral cavity, gum diseases, and diseases of internal organs.
Purulent-phlegmous glossitis
It is a severe form of inflammation, spreading not only to the deeper layers of the tongue, but also to other tissues of the oral cavity; the nearby lymph nodes are also involved in the process. In this case, the patient’s condition is serious, with severe intoxication and elevated temperature, so such patients are usually treated promptly. Antibiotics for this glossitis are a mandatory component of treatment.
Preventive measures
Simple preventative measures will prevent the onset of the disease. Basic rules of behavior and hygiene:
- Fruits and vegetables should always be washed before consumption.
- Food should not be excessively hot, cold, spicy or rough.
- The chewing process should be slow, which will prevent tongue biting.
- Personal hygiene should be observed: dental and oral care.
- It is necessary to have individual cutlery and a toothbrush.
- The brush should be renewed monthly. Change immediately after an illness.
- Regular visits to the dentist are recommended. It is necessary to treat diseases of the teeth and oral cavity in a timely manner, remove tartar and plaque, because these are the main sources of infection in the mouth.
- It is necessary to maintain adequate physical activity, which will increase immunity and the condition of the entire body.
Any pimple, growth or tubercle on the mucous membrane, both in an adult and in a child, requires close attention. You should not treat the bumps yourself; only a doctor can do this.
You should not pierce or try to squeeze out pimples on the mucous membrane; such actions can lead to negative consequences: the growth of foci of inflammation, the appearance of open wounds as a result of injuries.
The best thing a person can do if they have bumps on their tongue is to see a dentist or therapist. Such a decision will speed up recovery and prevent possible complications.
Special types of glossitis and their treatment
In addition to the above types of glossitis, dentists distinguish special types of glossitis, characterized by the development of limited specific changes in the tongue. These include:
Desquamative glossitis
It appears in the form of a “geographical” tongue, which has a “variegated” pinkish-red appearance, somewhat reminiscent of the outlines of the continents on a geographical map. In some cases, with the development of the inflammatory process, thinned areas cleared of plaque may change their position and shape within a short period of time (2 - 4 days). In such cases, desquamative glossitis is also called wandering glossitis. This can usually be observed with exudative diathesis, diseases of the digestive system, helminthic infestations, metabolic disorders, blood diseases, pregnant women, etc. Desquamative glossitis involves standard treatment, which leads to a gradual cleansing of the surface of the tongue and the disappearance of associated complaints in the patient.
Median rhomboid glossitis
It is characterized by the presence of a local thickening of the epithelium, usually located in the middle of the back of the tongue. In this case, the thickened area of the epithelium has a diamond-shaped or oval shape and can change its color from red to bluish. Rhomboid glossitis most often occurs in chronic diseases of the digestive system and is prone to chronicity and recurrence. Depending on the form of glossitis (flat, tuberculate, papillomatous), appropriate treatment is carried out: laser therapy, surgery, etc.
Atrophic glossitis
It often develops with insufficient intake of vitamins A and E. It usually appears as a single bright red, smooth spot that occupies the entire surface of the tongue. The focus of atrophy can persist for quite a long time without progressing. Sometimes the tongue decreases in size. Histological examination reveals dilation of blood and lymphatic vessels, swelling and inflammation in the papillary layer. Often, atrophic glossitis is a symptom of tongue damage due to gonorrhea.
Gunter's glossitis
Appears with a deficiency of vitamin B12 and folic acid. It most often occurs with blood diseases (usually anemia associated with impaired hematopoietic processes). In this form of the disease, the surface of the tongue is bright crimson in color and, due to atrophy of the papillae, has a “varnished” appearance. Gunter's glossitis involves treatment of the underlying disease by a therapist or hematologist.
Mycotic, candidal, or yeast glossitis
As a rule, it is a consequence of intensive antibacterial therapy, as a result of which the normal microflora in the patient’s body was suppressed. The disease manifests itself as swelling of the tongue, an accumulation of white plaque on it, with pronounced longitudinal and transverse grooves. Very often, mycotic glossitis occurs in young children and the elderly, as well as in people with weakened immune systems. Candidal glossitis requires treatment with antifungal drugs.
As an additional means for the treatment and prevention of glossitis, many experts have recently begun to recommend the use of an ultrasonic brush for oral hygiene.
Congenital pathologies
Sometimes neoplasms on the root of the tongue can be congenital. They appear as a result of developmental disorders of the fetus during the intrauterine period. Most often, such tumors are diagnosed in childhood. Let's take a closer look at congenital pathologies of the tongue:
- Hemangioma. This is a tumor consisting of blood cells. Its etiology is associated with a violation of embryogenesis. More often girls suffer from hemangioma; the disease is detected either at birth or in early childhood. The neoplasm looks like a red spot or a blue-purple lump. When the tumor is injured, heavy bleeding occurs.
- Lymphangioma. The tumor grows from lymphatic vessels. The rashes look like warts. Often the tongue is greatly enlarged in size. Lymphangioma is diagnosed in childhood. The tumor often becomes inflamed due to injury from hard food or teeth.
- Struma of the root of the tongue. This is a very rare disease. If embryonic development is disrupted, thyroid cells may enter the developing tongue. This is the cause of the pathology. The struma consists of thyroid tissue. It looks like a nodule under the tongue up to 3 cm in size. This disease is otherwise called goiter of the tongue. Clinically, it usually manifests itself during puberty. It becomes difficult for the child to swallow and speak. This tumor must be removed surgically, as it is prone to malignant degeneration.
Manifestations of tongue glossitis in children
In children, glossitis usually occurs at an early age - from 1 to 5 years. The causes of this pathological process have not yet been fully studied and can be very diverse: from infection to poor heredity. Externally, glossitis in children is manifested by the appearance of spots on the tongue, which slightly swells and itches. Itching and a burning sensation are the most unpleasant signs of glossitis, since a small child begins to scratch the tongue, thereby contributing to the appearance of microcracks with their subsequent infection. However, the disease does not pose a threat to the child’s life. The famous pediatrician Komarovsky does not recommend panicking about this and self-medicating by giving the baby serious medications. As a rule, multivitamins and a gentle regimen will have a positive effect within a week.
Features of glossitis during pregnancy
The causes of glossitis of the tongue in pregnant women are due to the fact that the immune defense weakens to allow the fetus to develop, which means that the body during this period becomes practically defenseless in the face of various bacteria and viruses. The second risk factor is a lack of vitamins and minerals obtained from food.
According to statistics, most often pregnant women experience a picture of desquamative and Gunter's glossitis. Symptoms that should alert you during pregnancy include:
- Profuse drooling. During the period of bearing a child, a woman already secretes a larger amount of saliva than usual, but a sharp increase may indicate the onset of glossitis.
- "Lacquered Tongue" A specific symptom that indicates the development of B12 deficiency anemia.
- Color change. White spots on the surface of the tongue alternate with spots of rich red color.
- Refusal of food. Acute glossitis in pregnant women is characterized by severe pain in the tongue during chewing and speaking, which, among other things, affects appetite.
As for the treatment of glossitis in pregnant women, the safety of the fetus comes first. Therefore, all therapy is exclusively local in nature (sprays, rinses), eliminating the penetration of the drug through the placenta. It is recommended to adjust your diet in such a way as to remove any foods that irritate your tongue.
Attention!
In order to avoid complications that can negatively affect the health of the fetus, treatment of glossitis during pregnancy must be carried out under the supervision of an obstetrician-gynecologist monitoring the woman.
Benign formations
Benign tumors usually appear as painless lumps on the base of the tongue. They rarely cause discomfort to the patient. Unpleasant sensations can only occur if there is accidental trauma or significant growth of the tumor.
However, we must remember that some tumors can develop into dangerous malignant neoplasms. Therefore, if a lump is detected in the tongue area, you need to make an appointment with a therapist or oncologist as soon as possible. Early diagnosis and treatment of tumors will help to avoid cancer pathologies.
Let's look at the most common types of benign neoplasms on the root of the tongue:
- Lipoma. In everyday life, such a lump is called a wen. It can form not only on the outer skin, but also on the tongue. Lipoma is often observed in people suffering from atherosclerosis and fat metabolism disorders. This is a mobile, painless formation in the form of a ball filled with the secretion of the sebaceous glands. There were no cases of malignant degeneration of lipoma.
- Fibroma. The tumor consists of connective tissue fibers. More often observed in children and adolescents. It looks like dense, painless bumps on the root of the tongue. Trauma stimulates tumor growth and can lead to malignant transformation.
- Neurofibroma. This neoplasm consists of nerve branches. Unlike most benign tumors, neurofibroma is quite painful. They look like a nodule on the root of the tongue. Rarely seen.
- Botriomycomoma. This tumor is otherwise called pyogenic granuloma. It looks like a bright red nodule on a stalk. The neoplasm does not cause any particular inconvenience to the patient and does not pose a threat to health or life. However, without treatment, the tumor grows rapidly and bleeds.
- Adenoma. The tumor grows from epithelial cells. It looks like growths in the form of polyps on the root of the tongue. Large adenomas can undergo malignant transformation.
- Myoma. This neoplasm occurs due to the proliferation of muscle tissue. It looks like a dense tumor up to 1 cm in size. Protrusions in the form of papillae sometimes appear on its surface. There is a danger of fibroids becoming malignant.
It is important to remember that the rapid growth of a benign tumor, a change in its color and the appearance of pain are often signs of malignant degeneration. Therefore, it is recommended to remove such tumors in the early stages.
Diagnosis and treatment
To diagnose glossitis in adults, the following basic methods are successfully used today.
- Examination
An experienced dentist in 95% of cases is able to diagnose glossitis based only on visual data. - RPR test
A special test that detects antibodies to the cardiolipin antigen. - Scraping
It is taken from the surface of the tongue to exclude syphilis, whose symptoms are similar to glossitis. - PCR
The most modern and accurate diagnostic method for identifying a wide range of infectious pathogens.
Treatment of glossitis depends on the form of the disease and analysis of concomitant diseases, but in any case it should be comprehensive:
- enhanced oral hygiene;
- general strengthening therapy aimed at increasing immunity;
- local treatment with antiseptics;
- strict diet;
- targeted medications (for example, for candidal glossitis - antifungal agents).
You can find out more about how to treat glossitis of the tongue in the article.
Treatment methods for tongue cancer
Regardless of the cause of tongue cancer, combination therapy is used to treat it, including the following methods:
- Surgery. The operation is aimed at radical removal of a malignant tumor: either partial resection (excision) of the tongue or its complete removal (glossectomy) is performed. In advanced cases, when the tumor has grown into the surrounding tissues, they are resected down to the bones of the lower jaw.
- Radiation therapy. There are remote therapy, when the tumor is irradiated at a distance with X-rays, and contact therapy (brachytherapy), when the radiation source (radioactive isotopes) is placed deep within the organ. Radiotherapy is performed both before and after surgery. The doctor determines how many sessions are needed.
- Polychemotherapy. It is used in advanced cases in the presence of distant metastases, when other methods cannot be used, or their effect is insufficient. Patients are treated with Cisplatin, Methotrexate and other drugs.
Surgeries in the later stages of the disease are often mutilating in nature - in some cases it is necessary to remove almost the entire lower jaw. After surgery, patients live with some restrictions. In order to create a satisfactory quality of life, they undergo reconstructive medical operations.
Is it worth treating glossitis with folk remedies?
If you have a question: how to cure glossitis, don’t waste time looking for folk remedies! If you notice characteristic symptoms that do not go away for more than a day, you need to seek help from a specialist. Treatment of glossitis should be carried out only by a dentist, who will determine the cause of the changes in the oral cavity, carry out all the necessary therapeutic and diagnostic procedures, prescribe a set of therapeutic measures that the patient can perform at home, and also monitor the entire treatment process, making changes to it as needed. necessary adjustments. Moscow dental clinics are presented in the “Search” section on our website.
Glossitis, like other periodontal diseases, is fraught with many complications, so treatment with folk remedies can only serve as an aid in complex therapy.
In order not to come face to face with glossitis, it is enough to brush your teeth regularly, including brushing your tongue, and do not skip preventive examinations at the dentist. In addition, doctors recommend avoiding excessive consumption of spicy foods and spices, limiting the intake of alcoholic beverages and smoking. Remember, disease is easier to prevent than to treat.