Free consultation with a doctor by phone
Surgeon appointments are available daily by appointment!!!
LLC "Your Doctor"
Chat with the doctor
Addresses of medical centers in Moscow (unified reference) +7 (495) 255-45-59
Make an appointment at the clinic Discount on services Promotions
- +7 (495) 255-45-59
- Surgical centers in Moscow
- Every day from 9.00 to 20.00
- call me back
You can make an appointment with our operators by calling +7 (495) 255-45-59
Prices for services Clinic address Make an appointment Call a surgeon to your home Pediatric surgeon Ligation
Hidradenitis on the labia can develop in women of both fertile and menopausal age, as well as in girls during puberty.
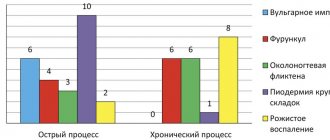
This disease refers to purulent-inflammatory processes of the apocrine glands. The most common causative agent is streptococcal infection; less often, opportunistic microorganisms can cause inflammation.
Useful information on the topic:
- Treatment of hidradenitis
- Hidradenitis in children
- Hidradenitis in pregnant women
- Causes of hidradenitis
- Hidradenitis inguinalis
- Autopsy of hidradenitis
- Hidradenitis suppurativa
- Hidradenitis under the armpit
- Removal of hidradenitis
- Prevention of hidradenitis
- Diagnosis of hidradenitis
- Lump under the arm
- Hidradenitis of the scrotum
Clinical signs
The disease usually develops gradually. In the initial stages, a compaction nodule can be detected on the labia. There may be several such nodules. The patient usually complains of pain or severe itching in the groin area. Next, clinical signs increase in the following sequence:
- Inflammatory nodules quickly increase in size. The affected area swells, turns red, and the local temperature rises.
- A purple, pear-shaped formation forms on the labia. The nodes are tightly fused to the skin. At this stage of the disease, the patient’s general condition suffers - the temperature rises, malaise, weakness, and headache develop.
- The maturation stage is accompanied by softening of the nodes and a breakthrough of purulent discharge. The pus may contain blood. The patient's general condition improves after the pus breaks through.
- After healing of some nodes of suppuration, others may develop in the neighborhood. Thus, the process can become chronic.
If you notice the first signs of the disease, you should not postpone your visit to the doctor. An experienced surgeon at our clinic will prescribe the necessary examinations and provide effective treatment.
Useful information about visiting a surgeon at the clinic:
- How to prepare for a surgeon's appointment
- What diseases does the surgeon treat?
- Calling a surgeon to your home
- Surgical care in the clinic
- Surgical care at home
- What symptoms should you contact a surgeon for?
- Treatment of surgical diseases
- Treatment of intestinal pathologies
- Treatment of skin surgical pathologies
- Treatment of bedsores and necrosis
- Treatment of parasitic diseases
- Treatment of inflammatory processes of soft tissues
- Treatment of diseases of the musculoskeletal system
- Diagnosis of surgical diseases
The effect of therapeutic therapy
- Antibiotics. The duration of treatment is a week, but in some cases it can last 10 days. Typically, the doctor prescribes the patient to take broad-spectrum antibiotics. Levofloxacin, at a low cost, suppresses the activity of pathogenic microorganisms and has a minimum of contraindications.
- Analgesics. For Bartholin gland cysts, dual-action drugs are prescribed: anti-inflammatory and analgesic. Spazmolgon and Diclofenac will help relieve both symptoms. For more pronounced pain, tablets are replaced with injections in the form of Analgin.
- Antiallergens. The disease in its progressive form causes swelling of the external genital organs. An unpleasant symptom is accompanied by itching and burning in this area. Suprastin, Zodak and Tavegil will help get rid of them.
- Sedatives. When antiallergenic drugs are included in the treatment regimen, it is necessary to take sedatives. You can use herbal medicines: tinctures of peony, motherwort and valerian. Echinacea, Timalin and Alfarekin are suitable immunostimulants.
- Vitamin therapy. Useful organic substances are taken in combination for effectiveness. Complivit and Centrum have proven themselves to be excellent in this regard.
You should dwell in more detail on reducing swelling and eliminating pain using ointments:
- Levomikol. For extensive swelling in the intimate area, this particular remedy is used because of the antibiotic in its composition. An exception is the desire to eliminate inflammation when the abscess capsule is intact.
- Ichthyol. If your doctor allows you to use this drug, you can use it to treat swelling in the area of the Bartholin gland. It is prohibited to use ichthyol ointment on your own for such purposes. Otherwise, the abscess will begin to rapidly grow in volume.
- Vishnevsky ointment. The basis of the drug is birch tar, which can accelerate the process of maturation of the abscess. For this reason, Vishnevsky ointment can only be prescribed by a specialist.
Types of surgical techniques for Bartholin gland cyst:
- Marsupialization. The operation is performed under local anesthesia because it involves the creation of a replacement glandular duct based on the blocked area. The scheme of its formation: penetration into the cyst cavity using an incision and cleaning it of pus. Next, the problem area is treated with an antiseptic and sutured to the mucous membrane of the external genitalia. In this case, the Bartholin gland does not change its position, and the secretory fluid is directed along a new channel.
- Use of laser (vaporization). In medicine, this method is considered a soft method that acts directly on the problem area. The laser does not injure healthy tissue, and the woman does not feel pain during the procedure. During the operation, a narrow-spectrum laser beam eliminates the cyst without bleeding.
- Husking. It is performed under general anesthesia, because the procedure involves the removal of the cystic capsule and its membrane. The recovery period reaches a month until the wound finally heals. The peeling process should be entrusted to a professional with extensive experience. The incision during surgery is reminiscent of the process of plastic surgery, where precision must be brought to perfection. An experienced surgeon will be able to make an incision right up to the cyst without causing injury to adjacent tissues without rupturing it. If there is an increased risk of touching a large number of blood vessels, enucleation is carried out in special cases.
- Radical method (extirpation). The procedure is complicated due to the need to excise the Bartholin gland itself along with the cystic capsule. It is prescribed for an organ abscess and the impossibility of blocking it with drug treatment. The disadvantage of extirpation is a decrease in the quality of a woman’s sexual life. In addition, the second gland will have to work for two, which it may not be able to cope with. The patient should prepare for the fact that a small suture will not be possible after extirpation.
The following complications may occur during and after surgery:
- Swelling of the vulva. It is usually diagnosed after enucleation. In most cases, swelling does not bother a woman for more than two days. Hematomas in this area can also occur after extirpation.
- Heavy bleeding. It begins when the veins at the base of the cyst are damaged during surgery.
- Loss of interest in intimate life. It is usually accompanied not by a woman’s desire to refuse sex, but by serious injury to the external genital organs.
- Relapse. The voiced pathology quite often, even after the removal of one gland, provokes blockage of the ducts in the second gland.
Causes and mechanisms of the disease
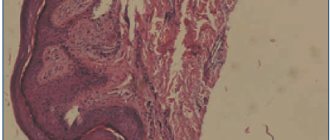
Pathogenic bacteria begin to spread through microscopic breaks in the integrity of the skin, and also through the blood and lymphatic vessels. Direct penetration of pathogenic flora into the mouth of the sweat gland is possible. Subsequently, the process involves the sebaceous glands, hair follicles and subcutaneous tissue.
Provoking factors are non-compliance with personal hygiene rules and careless hair removal during depilation. Wearing uncomfortable synthetic underwear can contribute to the development of skin irritation or diaper rash. Excessive sweating promotes the proliferation of microflora and the development of the pathological process. Metabolic disorders - obesity. Diabetes mellitus and endocrinopathies also create a favorable environment for the development of inflammation. A decrease in immunity after a serious illness or during pregnancy can help reduce the barrier functions of the skin and facilitate the entry of pathogens into tissues.
What symptoms do you see a surgeon for:
- Presence of hernial protrusion
- Daggering pains in the abdomen
- Bloating
- Pain in the right hypochondrium
- Bitterness in the mouth
- Nausea
- Presence of neoplasms on the skin
- Swelling and redness of the skin
- Bone fractures and bruises
- Wounds of any location
- Vomit
- Enlarged and painful lymph nodes
Symptoms
Bartholin gland cysts are common problems in women of reproductive age. Most often, women complain about aesthetic issues - asymmetry of the labia, swelling on one side of the labia majora. Cysts are usually asymptomatic and can be detected by a gynecologist during a routine examination. But in some cases (hypothermia, acute or subacute inflammatory process of the respiratory tract, acute or subacute inflammatory diseases of the genital tract, pelvic organs), they can increase and cause significant pain. Women with larger cysts may complain of discomfort when walking, sitting, and during sexual intercourse. If the Bartholin gland is functioning on the other side, the hydration of the vagina does not change during sexual intercourse. Due to blockage and the presence of a cyst, the Bartholin gland cannot fully function.[2] .[1]
Complications of hidradenitis on the labia
Treatment of hidradenitis at any stage in our clinic is usually highly effective.
If timely and adequate treatment is not carried out, hidradenitis on the labia can lead to a number of complications:
- If the abscess cavity is not opened in a timely manner, the pus may spread deep into the tissues. An abscess of the soft tissues of the genital organs develops.
- Decreased immunity and the presence of severe concomitant diseases can lead to the development of an abscess or phlegmon in the pelvic cavity.
- Penetration of a pyogenic infection into the bloodstream can cause the development of thrombosis of the veins of the lower extremities, iliac veins and pelvic veins.
- In severe cases, when the pathological process is at an advanced stage and against the background of severe immunodeficiency, sepsis and infectious-toxic shock can develop.
Diagnosis of the disease is usually made on the basis of clinical data. If you seek medical help in a timely manner, the prognosis of the disease is usually quite favorable.
Diagnostic methods in surgery:
- Doppler in surgery
- Colonoscopy
- Angiography
- CT scan
- Gastroscopy
- MRI
- Abdominal ultrasound
- X-ray
- Endoscopy
Prices:
| Code | Name of service | Prices |
| 1 | Initial appointment | 1200 |
| 2 | Repeated appointment | 900 |
| 3 | Calling a surgeon to your home | 3500 |
| 4 | Abdominal ultrasound | 2200 |
| 5 | Ultrasound of veins and vessels | 2400 |
| 6 | Doppler 2-3 trimester | 1200 |
| 7 | Rectoscopy | 1500 |
First aid for yourself
- Applying cold. They apply it only to the inflamed area, so as not to chill the ovaries and not provoke the occurrence of cystitis (pathology of the bladder). The exposure time to the problem area should not exceed 40 minutes. After a couple of hours, the procedure can be resumed.
- Application of antiseptic. The external genitalia can be treated with Miramistin solution. It is also suitable for douching if the woman does not have purulent discharge.
- Preparation of saline solution. Add 2 tbsp to a liter of warm boiled water. l table salt. The lotions are kept on the inflamed area for half an hour. The procedure is carried out 3-4 times a day.
Differential diagnosis
Includes cystic and solid lesions of the vulva, such as epidermal inclusion cyst, hidradenoma papilliferum and lipoma [3], vulvar neoplasms; - abscess of the Bartholin gland; - bartholinitis; vulvar abscess.
— Hematoma in the vulva area – there may also be complaints about a formation in the vulva area, discomfort during sexual intercourse, and pain. But when collecting anamnesis; and gynecological examination - the woman associates its appearance with mechanical trauma, childbirth; And the location is not in the area of projection of the large vestibular gland. [1]
— Paraurethral cysts – similar complaints. On examination - swelling in the paraurethral region (the area near the urethra) [1]
- Furunculosis of the labia majora. Complaints include formations in the perineal area, general malaise, hyperemia, edema, hyperthermia. Upon examination, the formation is localized in the area of the hair follicle and sebaceous gland. [1]