What is streptoderma?
Most often, streptoderma occurs in children. The reason for this is the imperfection of the protective function of the skin in childhood and the inability to fully control the child’s hygiene. Outbreaks of streptoderma are not uncommon in closed children's groups and preschool educational institutions. Our portal contains verified pediatric dermatologists and reviews
about them, which will help you choose a good specialist for your child. Streptoderma in adults is a consequence of parental contact with an infected child.
How is streptoderma transmitted?
When answering the question whether streptoderma is contagious or not, it should be noted that infection occurs in two ways:
- contact (direct contact of damaged skin with the skin of a carrier of the disease);
- contact-household (through household items, dishes, toys, towels).
Thus, the disease is contagious.
Classification of streptoderma
According to the nature of its occurrence, streptoderma in children and adults can be:
- primary (streptococci enter the body through damaged areas of the skin, an acute inflammatory process develops);
- secondary (the disease joins an existing streptococcal infection - eczema, chicken pox, herpes simplex virus, etc.).
Foci of streptoderma may appear:
- on the face;
- in the armpits;
- on the skin of the upper and lower extremities;
- on the hands, feet;
- on the folds behind the ears;
- in the groin area;
- in the intergluteal fold;
- in the inframammary folds.
Localization depends on the form of pathology. Dermatologists distinguish the following forms of streptoderma:
- streptococcal impetigo (foci form on the torso, upper and lower extremities, face);
- streptococcal diaper rash (affects the groin area, behind-the-ear folds, intergluteal fold, axillary area);
- bullous impetigo (inflammation occurs on the hands, feet, legs);
- streptococcal ecthyma (inflamed elements appear on the upper and lower extremities, buttocks);
- streptococcal infection (the disease is localized in the corners of the lips);
- tourniol (flaky lesions are diagnosed in the area of the nasal plates).
The spread of streptoderma throughout the body is facilitated by scratching painful areas of the skin, as well as getting water on the lesions (for example, while bathing, swimming in the pool).
Provoking factors
Provoking factors are streptococcus and skin damage (minimal is sufficient). The pathogen itself is constantly “in the neighborhood” of a person, but as long as the skin is intact, streptococcus does not manifest itself in any way. A small cut, wound, burn with an open blister is enough for the pathogenic microorganism to enter the tissue - this is how infection occurs. The causes of streptoderma on the arms and legs are frequent damage to the skin of these parts of the body.
But infection does not always occur even with a combination of provoking factors! Often a child’s immunity is so strong, and general hygiene is carried out so thoroughly that streptococci simply have no chance of invading. All parents should know whether streptoderma is contagious and how it is transmitted. This will help to carry out timely prevention and avoid problems.
A child can become infected both in kindergarten and when interacting with any person. The most common route of infection is contact, when the skin comes into direct contact with the skin of a sick person (for example, through hugging or kissing). A little less often, streptoderma is transmitted through household means through towels, toys, and common items. Airborne infection can also occur, but it is extremely rare and is considered an exception.
Reasons for the development of streptoderma
The causes of streptoderma include:
- Hormonal changes in the body. Due to hormonal imbalances, the condition of the skin worsens, so the risk of infection increases.
- Skin injuries. The skin protects against the penetration of pathogenic microorganisms. When abrasions and cuts occur, its protective function is reduced - streptococci can freely enter the body.
- Change in skin pH. Normally, the skin glands secrete substances onto the surface of the epithelium, which, when combined with exfoliated cells, create a protective layer. The latter provides protection against the penetration of infectious agents and promotes rapid restoration of the epithelium in case of cuts and injuries. A sharp change in the acid-base balance of the skin can lead to disruption of the microflora of the skin. As a result, the risk of developing an infectious process will increase.
Patients with allergic reactions manifested by dermatitis (urticaria, atopic dermatitis, seborrheic dermatitis) are also prone to streptoderma.
Symptoms of streptoderma
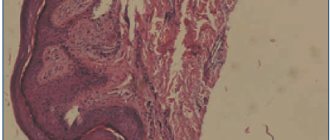
The symptoms of streptoderma in children and adults are the same. The duration of the incubation period for streptococcal infection is from 7 to 10 days. Then:
- Round pink spots appear on the skin (most often the face). Their outlines may be regular or irregular.
- After a few days, purulent-vesicular elements form on the surface of the lesions.
- With impetigo, they quickly open and heal. After them, no scars remain on the skin.
- With ecthyma, the germ layer of the skin is damaged, so the formation of permanent scars is possible.
- With shallow skin lesions, temporary hypopigmentation of the skin is possible after recovery.
There are no subjective sensations associated with the disease. In rare cases, patients complain of:
- skin itching;
- dryness of the affected areas;
- headache;
- muscle pain.
With extensive dermatological lesions in children, there may be an increase in body temperature and enlargement of regional lymph nodes.
If the pathological process takes on a diffuse nature, the foci of streptoderma very quickly spread throughout the body, merging with each other, forming larger elements.
Signs of chronic streptoderma
The disease can become chronic:
- overheating, hypothermia;
- phlebeurysm;
- decreased local immunity;
- the presence of open wound surfaces;
- decreased body reactivity;
- constant traumatization of affected areas of the skin (for example, children scratching sores).
Chronic streptoderma manifests itself:
- Large scaly lesions with uneven scalloped edges (diameter about 10 cm).
- Purulent blisters, after opening which form serous-purulent crusts of yellow or brown color.
- When the scabs are removed, an erosive, bright pink surface is exposed.
With a prolonged course, the disease can develop into microbial eczema.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
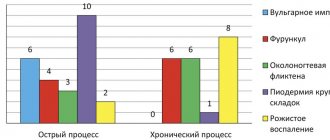
Classification
The pyoderma group includes a large number of diseases that are classified according to several criteria.
For convenience, the classification is presented in the form of a table below. Table 1. Classification of pyoderma
| By origin |
|
| According to the depth of the lesion (form of infection) |
|
| By pathogen |
|
| With the flow |
|
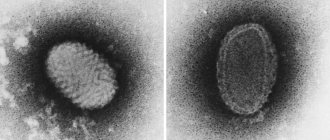
Diagnosis of streptoderma
The basic criteria for diagnosing streptoderma in children and adults are the presence of a clinical picture characteristic of the disease and the presence of the patient in the affected area. To confirm a preliminary diagnosis, the following is carried out:
- bacteriological culture of scrapings;
- microscopic examination.
The doctor finds streptococci in the scraping material. However, if before the consultation the patient independently used antibacterial ointments, microscopy may not be informative. Then the dermatologist relies only on symptoms.
Streptoderma must be differentiated from:
- pityriasis versicolor;
- hives;
- atypical dermatitis;
- eczema;
- pyoderma.
Additional diagnostic methods for the disease include:
- general and biochemical blood tests;
- blood test for thyroid hormones;
- general urine analysis;
- blood test for Wasserman reaction;
- blood test for syphilis.
You can undergo a full diagnosis at any of the dermatological centers
.
Nutrition during an exacerbation
Nutrition plays an important role in the treatment of various forms of pyoderma. The basic principles of diet during an exacerbation of the disease can be described as follows:
- Meals should be regular.
- Complete in composition of proteins, fats, carbohydrates and vitamins.
- The amount of salt in food is sharply limited (up to 5 g).
- The amount of carbohydrates is reduced.
- Alcohol is completely excluded.
- Any products that can provoke allergies are excluded (for this, an allergy history is carefully collected).
- The drinking regime is controlled; it is necessary to consume at least 1.5 liters of liquid.
The diet includes low-fat fermented milk products; fresh vegetables, herbs; lean boiled meat and fish; durum wheat pasta; boiled eggs; olive and linseed oils; buckwheat grain; bran.
How to treat streptoderma
To increase the effectiveness of streptoderma treatment, the patient should adhere to the following recommendations:
- stay at home until recovery, do not contact other people;
- avoid contact with common household objects;
- change bed linen every two days (wash used linen at high temperature and iron after washing);
- do not take a shower or bath, so as not to spread the infection throughout the body;
- wear underwear made from natural fabrics and change it every day.
How quickly a patient recovers depends on his age, individual characteristics of the body, the severity of the disease and the presence of concomitant pathologies. Today, thanks to high-quality antibacterial drugs, the effectiveness of treatment measures has increased significantly - it is possible to get rid of the disease in an average of 7-10 days.
For streptoderma, the patient is prescribed:
- Antiseptics (fucorcide, potassium permanganate, hydrogen peroxide 1%, methylene blue 2%, brilliant green 2%, salicylic alcohol 2%). They are applied not only to the hearth, but also around it. Hard crusts can be pre-treated with Vaseline, and then carefully removed and the resulting wound washed with an antiseptic.
- Antibiotics. For local treatment, ointments can be used: Triderm, Erythromycin, Gentamicin, Retapamulin, Baneocin, Bactroban, etc. They relieve inflammation and destroy pathogens.
For widespread streptoderma, medications are administered intramuscularly or intravenously. Since streptococcus is most sensitive to penicillins, dermatologists recommend penicillin antibiotics (Amoxicillin, Clarithromycin, Ciprofloxacin, Flemoxin Solutab, Erythromycin, Augmentin). The duration of antibacterial therapy is from 7 to 14 days.
To quickly cure streptoderma in children and adults, taking vitamin and mineral complexes that help strengthen the immune system is indicated. Among the effective immunomodulatory drugs: Neovir, Pyrogenal and Levamisole. They have a pronounced anti-inflammatory and desensitizing effect, increase the body's resistance to infectious agents.
Pyoderma in children
Pyoderma in children most often develops due to parents' failure to comply with the hygiene regime. That is, parents do not wash their hands before touching the child, wash the child poorly or rarely, the child’s clothes are poorly washed and not ironed, and their clothes are rarely changed. In rare cases, also if hygiene rules are not followed, it is possible for a child to become infected from relatives who have foci of chronic infection - carriers of staphylococci, streptococci, people with reduced immunity (patients with diabetes, alcoholism, old people, cancer patients).
to the begining