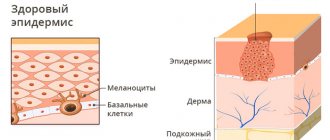
Basalioma is a tumor that grows from skin cells located in the basal layer of the epithelium. The neoplasm is prone to infiltrative growth and can grow into surrounding tissues, causing their destruction and metastases. However, this process occurs very slowly and can take years, which is why basal cell carcinoma is called a semi-malignant tumor.
- Forms of basal cell carcinoma
- Symptoms
- What is the danger of basal cell carcinoma?
- Reasons for the development of basal cell carcinoma
- Risk factors for basal cell carcinoma
- Stages
- Diagnostics
- Treatment methods
- Complications and prognosis of basal cell carcinoma
Forms of basal cell carcinoma
- Nodular-ulcerative form of basalioma. The disease begins with the formation of dense, clearly defined areas that rise above the surface of the skin - nodules. They may be grey, pink or yellowish. Gradually they increase in size, the skin above them becomes thinner and becomes, as it were, pearlescent. Then they merge with each other and form a plaque with raised edges and a depression inside. Gradually, this depression transforms into an ulcer, which becomes covered with a crust. It, in turn, also grows, infiltrating and destroying the underlying tissue, as a result of which the plaque begins to resemble a crater with very dense edges that resemble cartilage tissue. As the tumor grows, destruction of the underlying tissue occurs.
- Large nodular basalioma. This species develops from a single nodule, which, increasing in size, takes the form of a hemisphere with a diameter of up to 3 cm or more. Its surface may be smooth, but the presence of scales is possible. As the basal cell carcinoma grows, destruction begins on its surface - an ulcer appears, from which bloody discharge oozes.
- Infiltrative form. It is characterized by the most malignant course, since it initially grows “inside” the tissue, destroying it. It is very difficult to determine the clear boundaries of this form of basal cell carcinoma.
- The papillomatous or warty form of basalioma is characterized by neoplasms that resemble papillomas in appearance.
- Superficial basalioma. At the initial stage, it looks like a pink spot. Gradually it grows, thickens and transforms into a plaque. Nodules form along its edges, which also increase in size and, when fused, form a roller. The center of the tumor “sags” and changes color to a darker one. The tumor is not prone to infiltrative growth, but if it is large, infiltration into the underlying tissue is still possible.
- Scleroderma-like basalioma. This type of tumor manifests itself with the formation of a yellowish or whitish plaque. As it grows, its edges become eroded and covered with crusts. When they are separated, an inflammatory reaction occurs. Also, cysts filled with calcifications can develop in the thickness of the tumor.
- Fibrous basal cell carcinoma. This tumor begins with the formation of a nodule, which, as it grows in size, transforms into a plaque. Its surface layer becomes thinner and blood vessels can be seen through it.
- Turban basal cell carcinoma. This type of tumor is most often located on the head. It looks like a bluish hemisphere. In size they can reach 10 cm in diameter. There are several such formations.
Reviews about the treatment of basal cell carcinoma
Maria Alexandrovna, 57 years old “ Around the end of the summer of 2022, a reddish spot the size of a pea, with jagged edges, appeared on my right cheek. Over time, the spot began to increase in size and peel off. This alarmed me and I went to the clinic to see a surgeon, who examined me and did not give me a clear answer that it was he who did not give me. He prescribed me ointments, but they had no effect. As time passed, the spot became inflamed and turned into a weeping wound, which began to get worse. I was tired of all this and on the Internet I came across the LazerVita clinic and made an appointment with a surgeon. On the day of the appointment, the surgeon Gafarov Sarkhan Vidadievich saw me, examined the wound, he immediately did not like it and took cytology. After explaining everything to me and reassuring me, he made an appointment with oncologist Violetta Aleksandrovna Purtskhvanidze in 3 days, by which time the cytology will be ready. He prescribed me to treat with antiseptic solutions and antibiotics for now. Three days later, I came to see Violetta Alexandrovna. After examining the wound, she diagnosed Basal cell carcinoma, which was confirmed cytologically. She explained my diagnosis to me in detail, reassured me, and explained to me all the treatment options. Then, on the same day, Dr. Sarkhan Vidadievich performed an operation on me: laser removal. The operation went without complications, everything healed perfectly. I want to express my gratitude to the entire LazerVit team, and especially to doctor oncologist V.A. Purtskhvanidze. and doctor surgeon S.V. Gafarov Thank you very much!
» All reviews about the treatment of basal cell carcinoma and other diseases.
Symptoms
Most often, basalioma is located on open areas of the skin that are exposed to sunlight. For residents of the middle climate zone, this is the area of the face and hands. At the same time, the tumor “loves” the natural folds of the skin, so most often it is found in the area of the wings of the nose and nasolabial folds, on the lips, in the corners of the mouth and eyes. On the hands it is most often located on the folds of the fingers and in the spaces between the fingers.
The most typical manifestation of basal cell carcinoma is a pearly papule, a dense nodule, and sometimes a pink spot in the face, neck or torso. Over time, the tumor may ulcerate and bleed. Anamnesis helps to distinguish basal cell carcinoma from elements of acne or other skin lesions. A malignant tumor is present on the skin for a long time and does not go away. It can grow very slowly, over years. In this case, the patient does not experience any symptoms: he only notices a new “mole” on the skin. Despite the fact that basal cell carcinoma is not an aggressive malignant tumor, such “moles” should not be ignored. You need to visit a doctor immediately.
Prevention
Older people should definitely know that basal cell carcinoma is a disease whose risk increases with the number of years lived. To prevent the disease, you need to follow a few simple tips.
- Monitor your diet and limit your intake of animal proteins. It is worth paying attention to nuts, seeds and vegetables.
- In the summer, try not to go outside during hours of maximum solar activity (from 11 a.m. to 4 p.m.). When visiting the beach, apply a special cream with a protection factor of at least 20 units to unprotected skin. Attention should be paid to the skin of the face and neck, since this is the favorite place for localization of basal cell carcinoma.
- It is important not to traumatize old scars.
- It is necessary to carefully treat wounds that do not heal well. They can provoke the appearance of pathology.
- Maintain personal hygiene when working with carcinogenic substances and lubricants.
- Use cosmetic creams to prevent dry skin.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Reasons for the development of basal cell carcinoma
It is impossible to name clear and unambiguous reasons for the development of basal cell carcinoma in each specific case, as with any cancer. Scientists only know about the risk factors that contribute to the development of a malignant tumor. First of all, this is ultraviolet radiation from the Sun. It is no coincidence that basal cell cancer most often develops in open areas of the skin: in the face, neck, décolleté, and scalp.
The exact localization of the cells from which basal cell carcinoma originates is still a matter of debate. According to modern concepts, the tumor begins with cells located between the hair follicles, where the surface layer of the skin (epidermis) connects with the deeper layer (dermis), as well as in the area of the tubercle of the hair follicle. In 80–90% of cases, mutations in the genes of the Sonic Hedgehog signaling pathway are found in malignant cells.
Features of photo classification of basal cell carcinoma.
The presented photos show basal cell carcinoma in each of its main variants. Attempts have been made to classify basal cell carcinomas based on growth pattern or differentiation patterns, but such methods have not achieved universal acceptance. Thus, there is no generally accepted classification for basal cell carcinomas; about 26 different varieties have been described. The most common types are: 1) nodular, 2) pigmentary, 3) cystic, 4) ulcerative, 5) superficial, 6) fibrosing (scleroderma-like), 7) basosquamous (also known as metatypical cancer), and Pincus fibroepithelioma. Most often, basal cell carcinoma comes in one of three subtypes: nodular, superficial, or ulcerative. You will also see in the photo how basalioma has signs of several varieties at once.
Attempts have been made to classify basal cell carcinomas based on growth pattern or differentiation patterns, but such methods have not achieved universal acceptance. Thus, there is no generally accepted classification for basal cell carcinomas; about 26 different varieties have been described. The most common types are: 1) nodular, 2) pigmentary, 3) cystic, 4) ulcerative, 5) superficial, 6) fibrosing (scleroderma-like), 7) basosquamous (also known as metatypical cancer), and Pincus fibroepithelioma. Most often, basal cell carcinoma comes in one of three subtypes: nodular, superficial, or ulcerative. You will also see in the photo how basalioma has signs of several varieties at once.
Risk factors for basal cell carcinoma
- Light skin type.
- Red or blond hair.
- Prolonged exposure to ultraviolet radiation.
- Exposure of skin to radiation.
- Chronic trauma to the skin, for example, rubbing with uncomfortable clothing or shoes.
- Exposure of the skin to chemical carcinogens, including household chemicals.
The development of basal cell carcinoma may be due to genetic predisposition. This pathology is called Gorlin syndrome. It is characterized by the following symptoms: multiple foci of basal cell carcinoma, endocrine pathology, skeletal and mental disorders. Pathology begins to manifest itself at a young age.
Ulcerative basalioma in the photo.
Any basal cell carcinoma can ultimately develop into an ulcerative one (the so-called “gnawing ulcer”). The disease is often covered with a scab, the edges of the ulcer are roll-shaped, translucent, dense to the touch, and have a network of dilated vessels. The tumor sometimes heals on its own with the formation of scars. Patients think that traditional recipes worked, or they had some kind of “allergy”. Over time, in the same place, basal cell carcinoma will appear again, ulcerate, and heal again. But the size of the lesion will already be somewhat larger. This continues ad infinitum, and ulcerative (see photo) basal cell carcinoma reaches significant sizes.
In the photo, basalioma in the form of a dome-shaped red plaque, covered with dark and light crusts, is flaking. Resembles an injured seborrheic keratoma.
The photo shows a basal cell carcinoma that has turned from a nodular type into an ulcerative one. In the center of the tumor there is a deep ulceration, the edges are sharply raised, ridge-like.
The photo shows a gigantic skin basal cell carcinoma that has destroyed most of the face. In Russia, almost any oncologist sees several such patients throughout his life. The reasons are usually poverty, alcoholism, low funding for medicine, total neglect of one’s own health, and not the severity of the disease.
The photo shows an ulcerative basal cell carcinoma. It affects the occipital, retroauricular areas and spreads to the temple. The entire disease consists of hard tissue, partially covered with crusts. Studying the characteristic edges of the tumor will help make the diagnosis.
Diagnostics
Basalioma is a tumor of superficial localization, so it can be detected by examining the skin. Dermatoscopy—examination of an area of skin under magnification—helps not to miss suspicious neoplasms and to suspect their malignant nature in time. Special technologies are also being developed that allow monitoring the dynamics of skin tumors with the compilation of a detailed cartogram.
Any oncological diagnosis requires morphological confirmation. To do this, a biopsy is performed - a fragment of tumor tissue is taken, which is sent to the laboratory, dissected and studied under a microscope.
For skin pathologies, the following types of biopsy are used:
- Incisional - a small piece of the tumor is cut off with a scalpel, affecting healthy tissue. This method is used for large basal cell carcinomas.
- Excisional biopsy - the entire tumor is completely removed, including healthy tissue. Such intervention is possible if the tumor is small, no more than 1 cm.
If the basal cell carcinoma is located in the facial area, it is not advisable to perform a biopsy for aesthetic reasons. In such cases, you can get by with a cytological examination, when scrapings are taken from the surface of the tumor or its contents are punctured.
To search for metastases, conventional medical imaging methods are used - CT, ultrasound, MRI. If there is evidence of damage to the lymph nodes, they are punctured and the material is sent for cytology.
Pigmented basal cell carcinoma (basalioma) in the photo.
About 2% of all basal cell carcinomas are completely pigmented. A small degree of pigmentation is present in a large number of basal cell carcinomas. Although raised edges, waxy sheen, and telangiectasias (dilated blood vessels) are usually present, they help establish the correct diagnosis. However, such (see photo) basal cell carcinoma can hardly be distinguished from melanoma. The final point in establishing the diagnosis will be made by histological examination.
The photo shows a nodular basal cell carcinoma with several spots of brown pigment. That is why pigmented basal cell carcinoma is often classified as a type of nodular carcinoma.
A pigmented type of basal cell carcinoma. The photo shows a nodule with an uneven black color and uneven edges; the disease can easily be confused with melanoma. In this case, the diagnosis will be prompted by the characteristic translucency and blood vessels on the surface of the tumor.
Photo of pigmented basal cell carcinoma. A black knot of several lobules with waxy, raised edges. This disease is difficult to distinguish from melanoma.
The photo shows a pigmented basal cell carcinoma. An unevenly colored black plaque with an area of spontaneous healing in the center. In appearance it cannot be distinguished from superficial melanoma. Histology is required for diagnosis.
Treatment methods
The main methods of treating basal cell carcinoma are surgery and radiation therapy. The choice of method will be determined by the location of the tumor. In addition, other removal methods can be used: local chemotherapy, photodynamic therapy, etc.
Surgical removal of basal cell carcinoma
Surgery is the preferred method of treating basal cell carcinoma, as it allows you to control the radicality of the intervention. The following methods are used:
- Classical removal - the tumor is excised with a scalpel at a distance of 0.5-1 cm from its edges. The wound is sutured with cosmetic sutures, and the removed material is sent for histological examination. If pathologists issue a conclusion that there are no malignant cells in the cut-off edges, the treatment is considered radical and no other measures are required. However, this method is problematic to use if the basal cell carcinoma is located in the face, and even more so on the eyelids, nose or ear.
- Curettage with electrocoagulation. In this case, the basalioma is scraped out with a curette, and the bottom of the wound is cauterized with an electrocoagulator. After healing, a whitish scar remains.
Regional metastases in the lymph nodes are also surgically removed. Typically, during such an operation, the fatty tissue around the affected nodes is excised.
Radiation therapy for basal cell carcinoma
If surgical treatment is not possible, radiation therapy is prescribed. Considering the good sensitivity of basal cell carcinoma to the effects of ionizing radiation, the effectiveness of such treatment reaches 90%. Radiation therapy is carried out in long courses over several weeks. In this case, irradiation sessions are carried out daily for 5 days, and then a 2-day break is taken in order for healthy tissue to be restored. Indications for radiation therapy are the following conditions:
- Elderly age.
- An inconvenient location for basal cell carcinoma from the point of view of surgical removal is the face, especially the nose, lips, eyelids and ears.
- High risks of recurrence after surgical removal.
Chemotherapy
Local and systemic chemotherapy can be used to treat basal cell carcinoma. Local chemotherapy is used to treat superficial forms of the disease. It involves the use of ointments containing antitumor drugs, for example, fluorouracil.
Systemic therapy is used for persistent recurrent basal cell carcinomas and in the presence of distant metastases. As part of the treatment, drugs are prescribed that act on the processes that ensure the uncontrolled proliferation of malignant cells. For basal cell carcinoma, the effectiveness of drugs from the group of inhibitors of the Hedgehog signaling pathway has been proven, these are Vismodegib and Sinidegib.
Photodynamic therapy
Photodynamic therapy is a relatively new, but very promising method for the treatment of malignant neoplasms of superficial localizations. Its effectiveness is based on the selective destruction of pathologically altered cells, which occurs as a result of a photochemical reaction in which the photosensitizer enters under the influence of light with a certain wavelength.
When treating basal cell carcinoma, the photosensitizer is applied superficially in the form of an ointment or application. Then the tumor is exposed to a lamp emitting light of specified parameters. As a result, the cell activates the production of free radicals, which damage membranes and organelles, leading to the death of the neoplasm as necrosis. After a few days, a scab forms in its place. When it falls off, young skin will form in its place. Photodynamic therapy gives a very good therapeutic effect and aesthetic result. It is recommended for use in the treatment of superficial basal cell carcinoma in the face and hands.
Nodular basal cell carcinoma in the photo.
This is the most common type of basal cell carcinoma, accounting for about 60% of all primary cases. It looks like a raised, translucent papule or nodule with dilated vessels on the surface (telangiectasia). Such a nodule may ulcerate and have pigment inclusions. Most often, nodular basal cell carcinoma appears on the head and neck, you will notice this in the photo. Over time, the borders become roll-shaped and pearly, while the central part ulcerates - a so-called corrosive ulcer is formed. Without treatment, the nodular version of basal cell carcinoma reaches large sizes and spreads deeply, destroying the eyelids, nose or ears. In large lesions, tissue destruction and ulceration often dominate the picture, so that it is not always easy to recognize the true nature of the disease.
The photo shows a classic-looking nodular basal cell carcinoma. Pearly pink tumor with protruding dilated vessels.
Photo of basal cell carcinoma with characteristic vasodilation and glassy sheen. You can also see thin crusts on the surface.
The initial manifestations of basal cell carcinoma are on the nose at the inner corner of the eye. The pearl nodule is oval in shape, there is a depression in the center, the edges are slightly pigmented, roll-shaped.
The photo shows a nodular skin basal cell carcinoma. Smooth, pearly tumor with telangiectasia, small scabs on one of the edges. Dense to the touch, clearly defined, does not bother you in any way.
Complications and prognosis of basal cell carcinoma
We have already said that basal cell carcinoma is a semi-malignant tumor. It grows slowly and rarely metastasizes. With timely treatment, the prognosis is favorable. Relapses develop in less than 10% of patients. The situation is worse in patients with large basal cell carcinomas or with an infiltrative form of the disease. They have a high risk of relapse and distant metastases. Moreover, such forms of basal cell carcinoma can destroy the underlying tissues, leading to disfigurement of appearance, the development of bleeding, chronic inflammation and dysfunction of the affected segment.
Book a consultation 24 hours a day
+7+7+78
Cystic basal cell carcinoma (basal cell carcinoma) in the photo.
Cystic basal cell carcinoma is formed as a result of the accumulation of fluid in the tumor. May have a pink or blue-gray color and releases a clear liquid when pierced or cut. If the tumor is located in the orbital area, it may be mistaken for hydrocystoma. The cystic change is not always noticeable (see photo below), and, therefore, basal cell carcinoma is perceived as a typical nodular variety.
The photo shows a transitional basal cell carcinoma, the so-called nodular cystic type. Mucus slowly accumulates in the nodule, gradually leading to the cystic version of basal cell carcinoma.
The photo shows a cystic basal cell carcinoma. Initially, the disease had the appearance of nodular basal cell carcinoma. Gradually, the accumulation of fluid led to the formation of a tense, translucent cyst (sac) with dilated vessels.
Types of disease
Based on the type of formation and its characteristics, several types of skin basal cell carcinoma are distinguished.
- Nodular-ulcerative. This is a red or pink nodule that appears mainly on the face, grows very slowly and becomes covered with ulcers over time. Over time, the shape becomes deformed and adjacent tissues are affected and destroyed.
- Solid. Light pink or yellow formation in the form of a semicircle. It grows slowly, capillaries are visible under the surface.
- Warty. Multiple node, shaped like a cauliflower. No ulcers.
- Perforating. Grows faster than others, completely covered with ulcers. It mainly appears in areas that are constantly damaged.
- Cylinder. The purple-pink multiple tumor is a basal cell carcinoma of the scalp and scalp.
- Scleroderma-like. Resembles a superficial nodule that may or may not develop an ulcer.
- Flat scar (also pigmented). In the process of development, it looks like a mole surrounded by various formations (like a necklace). Then ulcers appear, and after healing, a scar remains on a dark background.
- Superficial. Resembles a flat plaque surrounded by small formations. It grows for a long time and may not manifest itself for years and not bother the patient.
- Adenoid. Formed in the area of the tonsils, it consists of many cyst-like nodules.
Like other forms of cancer, basal cell carcinoma has its own stages.
Basosquamous carcinoma (metatypical cancer) in the photo.
Metatypic cancer is a tumor that combines the features of basal cell carcinoma and squamous cell carcinoma. This type of basal cell carcinoma behaves more like squamous cell carcinoma than other types of basal cell carcinoma. Namely, it is more aggressive and destructive in its behavior. It metastasizes more often, and also has a greater likelihood of recurrence (reoccurring in the same place) after treatment. This variant occurs in 1% of all basal cell carcinomas. The risk of metastasis of this variant of basal cell carcinoma is 9-10%.
Basosquamous basalioma is recognized on the basis of the picture taken under the microscope. In this photo, basal cell carcinoma resembles the morpheaform variety; ulcerative variants are often also found.
Micrographic surgery of skin tumors using the Mohs method
From history : the method was developed in the 30s by the American surgeon Frederic E. Mohs for the treatment of skin tumors. The principle of the method was a histological assessment of the cleanliness of the entire removed surface. Over the following years, the method was improved in terms of both surgical technique and histological techniques. And currently, Mohs surgery is the number 1 method in the treatment of basal cell and squamous cell cancers of the face (American recommendations - NCCN 1.2019 and European consensus 2019).
The principle of the method . The operation consists of alternating surgical and pathohistological stages, so it is almost always performed under local anesthesia. First, the tumor itself and 1 mm of visually healthy skin are excised. At the same time, the excised lesion is presented in the form of a conventional watch dial, and a mark is applied to the patient’s skin (conventional 12 o’clock, if the size is large there may be several of them). A photographic map of the removed material and the corresponding area of the face with a mark is made. The material is immediately subjected to histological examination.
How is histological examination performed? This is one of the key stages of micrographic surgery. During a standard histological examination, sections are made according to the loaf bread principle - by analogy with how we cut a loaf of bread. This provides good visualization of the tumor, but the cleanliness of the edge can only be assessed at the cut site. There is no information about the edge between the slices.
During Mohs surgery, the entire marginal and deep surfaces of the removed lesion are divided into several parts (the location of these parts on a conventional dial is necessarily noted, the parts are marked with special indelible fabric paints). And the slices are oriented parallel to the removal surface . The study is performed using the technique of fresh frozen sections, then the sections are stained and evaluated by a Mohs surgeon. Accordingly, the entire histological stage, depending on the size of the lesion, takes 30-40 minutes. At this time, the patient is in the rest room with a temporary bandage.
There are then 2 options:
- If all cut edges are clean, the patient is again invited to the operating room and the wound is sutured (either direct suturing, or wound plastic using local tissue, or a skin autograft - it is decided individually depending on the size and location of the wound to obtain the most aesthetic result).
- If the presence of a tumor is detected in any of the sections, then, according to the markings, an additional 1 mm of tissue thickness is removed from the corresponding area of the skin wound and sent for histological examination using the above technique. And so on until the entire surface is “clean,” after which the wound is sutured.
Fibrosing (scleroderma-like, sclerosing, morpheaform) basalioma in the photo.
Sclerosing basal cell carcinoma is a rare subtype that appears as a slightly raised or sunken white, gray, or yellow scar resulting from a strong scarring reaction to tumor cells. This type of tumor penetrates very deeply and has seemingly indefinable boundaries. Often does not have the characteristic features of basal cell carcinomas, such as erythema and telangiectasia. All this makes diagnosis difficult. Palpation (by touch) helps to partially determine the boundaries of the tumor. Sclerosing basal cell carcinoma (see photo below) can progress to nodular or ulcerative varieties. And of course, a biopsy will be important here. The lesions can go quite deep before they are discovered.
The photo shows a fibrosing type of basal cell carcinoma of the skin of the neck. It looks like a plaque with yellow or white scales, with poorly defined edges, reminiscent of a scar.
The photo shows a basal cell carcinoma of the sclerosing variety with areas of independent scarring, ulceration and pigmentation. Located on the lateral surface of the chest.