Amelanotic melanoma occurs in 1.8-8.1% of all malignant melanocytic tumors. This tumor is characterized by aggressive growth, so it needs to be treated as early as possible.
At Euroonco, treatment of non-pigmented melanoma is carried out according to international standards. In some cases, patients may take part in clinical trials of new therapies.
- Amelanotic melanoma - what is it?
- Causes and risk factors
- Symptoms of the disease
- Localization zones of formations
- Diagnostics
- Classification of the disease
- Stages
- Complications and consequences of the disease
- Treatment of the disease
- Prognosis and prevention
Amelanotic melanoma - what is it?
This is a malignant tumor whose cells contain an extremely small amount of the pigment melanin (this is what gives the brown color to “regular” melanoma). As a result, neoplasia is very similar to various other skin growths, both malignant and benign. Therefore, it is quite difficult to diagnose achromatic melanocytic tumor at an early stage.
Melanoma containing little melanin is characterized by fairly rapid growth into fatty tissue and early ulceration. This creates conditions for metastasis.
A peculiarity of non-pigmented melanoma is the cessation of its growth after the sending of the first metastases. Moreover, after this, the primary tumor can completely disappear.
Colorless melanoma cells contain small amounts of melanin due to:
- insufficient content of the amino acid tyrosine in the body;
- disruption of melanin formation during tumor cell division.
Why does a mole hurt?
There are several main reasons why a mole hurts.
Most often, pain occurs as a result of injury.
This is also accompanied by minor bleeding, swelling and hyperemia of the surrounding soft tissue.
If the mole hurts and itches, and new nevi appear, hormonal changes are suspected.
This occurs more often in women during pregnancy.
Painful moles are caused by the following reasons:
- Injuries - a hanging mole in particular often hurts, which can easily be touched by clothing, a washcloth or jewelry, depending on its location. But other types of moles can also be injured, sometimes this happens in beauty salons when performing intense massage, using anti-cellulite cups, or performing depilation. More often, nevi located in the armpits, pubis, collar area, and on the folds of the lower and upper extremities are injured. Often the cause of pain is an injury to a mole while using a razor. Any damage to a benign formation should not be ignored, since even minor scratching can provoke malignancy, which poses a direct threat to human life.
- Increase in size - the cause of such changes is often hormonal changes, but sometimes the mole grows and hurts when the process becomes malignant.
- Prolonged exposure to direct sunlight or staying in a solarium leads to burns. In this case, the mole hurts and may itch, but after 3-5 days the discomfort goes away on its own. If after being under the hot sun the pain does not disappear for 7 or more days, you should see a doctor and undergo an examination, the process of malignancy (malignancy) may have begun.
- Inflammatory processes - most often occur when a mole is damaged and infection enters, which causes hyperemia, pain and even swelling.
- Thermal burn of the skin - exposure to hot steam or liquid, fire, high temperatures causes burns of varying degrees of severity, the most sensitive areas are moles and age spots, where increased pain is felt.
- Hypothermia or overheating of the body - with any deviations in body temperature from the norm increases the sensitivity of the skin. Not only existing nevi can hurt, but also the site of a mole removed in the recent past.
Causes and risk factors
There is no single cause of melanoma, either pigmented or non-pigmented. In 5-12% of cases, the disease occurs under the influence of hereditary predisposition. Then one of the genes that has undergone mutation is passed on to the descendants. The main ones are:
- CDK4, responsible for the production of an enzyme that suppresses tumor development;
- CDKN2A, essential for normal cell division.
The risk of developing melanoma in relatives is 8-14% if:
- amelanoma has been diagnosed in two or more of the person's siblings, especially if they are twins;
- malignant melanocytic formation was present in both parents;
- Two or more of the person's children have been diagnosed with melanoma.
Melanoma genes can “accumulate” and be passed on in families living in regions with a high incidence of this tumor. In this case, the risk of developing such a neoplasm is 5-10%. In approximately every 12-50th case, the formation of non-pigmented neoplasia will occur.
The majority (about 90%) of cases of melanoma development are sporadic, that is, not associated with hereditary transmission, cases. In this case, the cause of the tumor is considered to be ultraviolet radiation - rays of types B and A.
Risk factors for malignant neoplasms from melanocyte cells are:
- fair skin (Fitzpatrick phenotype I and II), especially in combination with red hair and freckles;
- received sunburn (including in early childhood);
- use of PUVA therapy (for the treatment of psoriasis, vitiligo);
- large congenital nevus - when it occupies an area of more than 5% (5 palms) of the body area;
- immunodeficiency - congenital, caused by taking glucocorticoid drugs or cytostatics for the treatment of rheumatoid arthritis, autoimmune diseases, to prevent transplant rejection.
In 70% of melanomas do not develop on “clean” skin, but as a result of the degeneration of such benign formations as:
- blue nevus;
- nevus of Ott;
- dysplastic nevus;
- Dubreuil's melanosis;
- complex pigmented nevus;
- Pick's melanosis.
The process of melanoma formation is triggered by injury, frequent exposure of pigment formation to ultraviolet rays. A change in hormonal balance may also be a trigger factor. The risk of developing non-pigmented melanoma is 1.8-8.1%.
Cause of melanoma
The content of the article
The causes of melanoma can be different. Scientists include genetic and environmental factors among them. It is estimated that up to 10% of cases of the disease are associated with genetic complications. It is therefore recommended that the next of kin (for first degree relatives) of the patient undergo dermatological consultation and monitoring.
Environmental factors are also of great importance, among which sunbathing and associated skin burns stand out first.
Skin burn from sunbathing
Melanocytic changes can also cause melanoma. They usually appear on the skin as small nevi. They can be congenital or acquired. However, assessing the change, whether it is just a harmless mole or cancer, is based on additional diagnostic tests.
Almost everyone is at risk of developing this disease because we are exposed to sunlight every day, which is a very important factor in the development of melanoma. Therefore, it is very important to regularly examine moles yourself and have an annual examination with a dermatologist. A timely removed mole will save you from painful procedures and difficult operations.
Symptoms of the disease
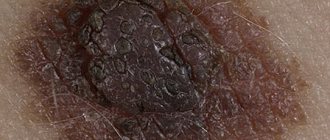
Amelanotic melanoma is a nodule on the skin:
- round or oval;
- densely elastic to the touch;
- "fleshy";
- flesh-colored, pinkish, brownish or bluish-reddish in color;
- with a surface on which there is no usual skin pattern;
- may have a leg;
- It doesn't hurt, but it may itch.
Unlike pigmented melanoma, a tumor of melanocytes without pigment is often more symmetrical, it is less prone to swelling and the formation of small satellite papillae around it.
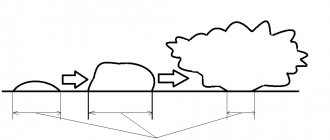
“Colorless” melanomas grow quickly - growing from 2-3 mm to 2-3 cm in just 2-4 months. Such a “nodule” may be lumpy, and ulcers or formations similar to small papillomas can be found on it.
The most dangerous thing is that the growth of achromatic melanoma is observed not only upward, but also deep into the skin. It is prone to decay. Therefore, in the later stages, the tumor looks like an ulcer, the edges of which are dense and raised, and small papillae are visible at the bottom.
How to recognize amelanotic melanoma in the early stages?
The first symptoms of non-pigmented melanoma are the appearance of a pink spot on the skin (clean or in the area of pigment formations). Such a spot grows over several weeks/months and is characterized by increased friability and bleeding.
Some types of melanoma without pigment look like a gradually enlarging wart or papilloma. Other non-pigmented melanomas appear as a brown streak on the nail that extends to the tip of the finger.
In the initial stages, non-pigmented tumors do not hurt or itch, so they are rarely paid attention to.
Types of melanoma
Skin lesions diagnosed as melanoma do not always look the same. Thus, there are several types of melanomas, which define different clinical subtypes of the disease.
- Superficial melanoma
. It is indicated that the most common type of melanoma, which accounts for up to 60-70% of all cases of the disease, is superficial melanoma. This group of melanomas is most often based on pigmented lesions of a dysplastic nature. - Nodular melanoma
. Indicated as the most severe form of the disease, affecting 10-30% of patients. This group, in turn, includes two clinical subtypes. The first is lentiginous melanoma, which is a malignant form. Occurs in 5-15% of cases. It most often affects older people, especially in the neck or face. Lentiginous melanoma is caused by prolonged and prolonged exposure of the skin to sunlight. The second subtype is acral melanoma, which is observed on the inner surface of the skin of the arms and legs. - Colorless melanoma
. The disease also includes pigmented melanoma. Only 2% of patients suffer from it. This is a characteristic type of skin lesion in which pigment is absent. In this case, the symptoms are also quite specific, and the not very characteristic but enlarging pink-red papule should be of concern.
Superficial melanoma
Nodular melanoma
You should also pay attention to the so-called Spitz moles, which are a juvenile form of melanoma. Most often, scientists indicate that this is an active nevus, usually single, and occurs in young people.
The surface of a Spitz mole is very well demarcated from the surrounding area and has a smooth, red or bluish color. Most often it occurs on the face. When observing the lesion, there is no inflammatory reaction. Spitz nevi rarely become cancerous, although it is recommended to remove them before puberty.
Diagnostics
At the slightest suspicion of melanoma, you should consult an oncologist or dermato-oncologist. With the help of an examination, which at the first stage is simple and painless, the doctor will be able to distinguish non-pigmented melanoma from similar diseases: seborrheic keratosis, pyogenic granuloma, Spitz nevus, basal cell skin cancer, hemangioma.
The first thing Euroonco doctors begin diagnosing melanoma with is an examination of the formation. The dermato-oncologist needs to evaluate the appearance, consistency, symmetry, bleeding of the tumor, and palpate the nearest lymph nodes.
Next, he collects an anamnesis - he finds out from the patient when the non-pigmented neoplasm appeared, whether a diagnosis of melanoma was made in one of the closest relatives, whether there were frequent injuries to the tumor, whether it was exposed to excessive sun exposure.
At the same stage, the doctor performs digital dermatoscopy - examination of the tumor using a special device. A dermatoscope magnifies the tumor and allows you to analyze the structure of its deep layers, assess the location and course of blood vessels. This is very important for diagnosing amelanoma.
If, according to dermatoscopy, malignancy of the tumor cannot be excluded, a second diagnostic stage is prescribed. This is a biopsy - obtaining tumor tissue for research. It is performed under local anesthesia and is excisional. This means that both the tumor and the surrounding tissue are completely removed.
The area obtained by biopsy is examined under a microscope. Immunohistochemical studies (IHC) are also performed. It involves detecting certain types of proteins in a tissue sample (biopsy) to determine the type of melanoma and its sensitivity to chemotherapy drugs.
When the diagnosis of non-pigmented melanoma is confirmed, the third diagnostic stage is carried out - determining the extent of the process (tumor stage). To do this, metastases are detected in the lymph nodes and internal organs:
- Lymph node metastasis is determined by sentinel lymph node biopsy
The procedure is not mandatory. Euroonko doctors recommend undergoing it if the thickness of the removed melanoma is more than 1 mm. This is due to the fact that in this situation the risk of metastases to regional lymph nodes increases. Thus, even with a tumor thickness of 0.75-1 mm, micrometastases in the “sentinel” node are observed in 4-12% of patients.
A sentinel lymph node biopsy is performed as follows. A special drug is injected into the area of the removed melanoma. Next, the doctor observes which lymph node the drug entered first and removes it. This happens under local anesthesia.
After this, the lymph node is carefully examined under a microscope, using also the IHC method. If no melanoma cells are detected, it means that the tumor has not sent daughter cells beyond the occupied area.
- Metastasis to internal organs
It is determined by magnetic resonance imaging (MRI) and computed tomography (CT) methods.
Melanoma is a malignant skin tumor
Melanoma is one of the types of malignant skin tumors. The test that confirms or excludes the diagnosis is a biopsy, which confirms the diagnosis based on microscopic examination. The results of the performed biopsy provide information about factors that have a significant impact on the prognosis of the patient's treatment. This information allows you to determine the further course of the treatment process.
Melanoma biopsy
Examination of removed tumors for malignancy is carried out on the basis of macro- and microscopic examination. Among the factors that play a significant role in assessing the patient's health prognosis, primary outbreaks are of great importance. If there are no metastases in the progression of the disease, the change in thickness (Breslow scale) and the presence of ulcers observed in the primary lesion are assessed.
Due to the fact that melanoma is classified as a malignant neoplasm, some patients experience metastases to other organs. Therefore, during diagnosis and treatment, the surrounding lymph nodes are also checked.
Stages
In its development, amelanotic melanoma can go through 4 stages. Each of them, except the fourth, is divided into several substages.
The stages are determined according to three criteria:
- thickness of the tumor (depth of its germination into the skin);
- metastases to regional lymph nodes;
- metastases to internal organs.
| Stage | Tumor thickness | Metastases to regional lymph nodes | Metastases to internal organs |
| 0 | within the epidermis | No | No |
| I.A. | to the papillary layer of the dermis, reticular (deep) does not affect, no ulcers | No | No |
| I.B. | penetrates into the deep layer of the dermis, possibly into the subcutaneous tissue (thickness - from 1 to 2 mm), no ulcers | No | No |
| II A | tumor thickness - from 1 to 2 mm, there is ulceration or thickness from 2 to 4 mm, no ulcers | No | No |
| II B | thickness from 2 to 4 mm, with ulcerations or thickness above 4 mm, without ulcers | No | No |
| II C | thickness more than 4 mm, with ulcerations | No | No |
| III A | any thickness, no ulcers yet | there are micrometastases in 1-3 regional lymph nodes | No |
| III B | any thickness, without ulceration | or macrometastases in 1-3 regional lymph nodes or metastases to the skin near the tumor, but without metastases in regional lymph nodes | No |
| any thickness, with the formation of ulcers | or micrometastases in 1-3 regional lymph nodes or metastases to the skin near the tumor, but without metastases in regional lymph nodes | No | |
| III C | any thickness, with ulceration | or micro- or macrometastases in 2-3 regional lymph nodes | No |
| any | more than 3 regional lymph nodes are affected by metastases, or there are several affected lymph nodes fused together, or there are metastases in the skin near the tumor, despite the fact that they are also present in the regional lymph nodes | No | |
| IV | any size | any quantity | There is |
By what signs can you distinguish melanoma from a mole?
The differences between a mole and melanoma are mostly obvious and distinguishing them is not difficult. However, it will be useful to know a number of specific changes that you should pay attention to first. They are classified according to several relevant parameters.
C (Color)
The color of the pigmented spot plays a big role. First of all, excessive pigmentation or, conversely, discoloration indicates the danger of a mole. Especially if these changes occurred abruptly. In addition, the alarm should be sounded if the mole has more than two shades of color - it could be darker specks on a light background or simply uneven color. Black, dark brown and other bright colors are also a reason to consult an oncologist. Taking these parameters into account, you can understand how to recognize melanoma in time.
D (Diameter)
The normal size of a mole should not exceed 5 millimeters. If the diameter of the pigmentation is larger, it is necessary to conduct a histological examination. This applies to moles that have no other pathological parameters other than color.
A (Assymetry)
Asymmetry of the shape of the pigmented spot. How to determine melanoma by the asymmetry of a mole? Birthmarks should have at least approximate symmetry, that is, if you draw a line through the middle of the mole, the halves should be at least similar.
E (Evolution)
Development of a mole and changes in it. If at least one of the listed factors - size, symmetry or color - changes its parameters within a short period of time, you should immediately contact a specialist for examination.
B (Boarder)
The border of the mole should be smooth or rounded. All unevenness, jaggedness and roughness should alert you. In a situation where such a sign is combined with others, it will be a reason for additional examination of the mole or consultation with a doctor.
Additional signs will also be the appearance of ulcerations or inflammatory processes at the site of the mole, unpleasant sensations on it (itching, pain, paresthesia).
Thus, the degeneration of a mole into melanoma is not an instantaneous or very fast process. It is important to recognize the tumor in time and seek medical help.
Complications and consequences of the disease
Pigmentless melanoma can be complicated by screenings of daughter tumors, metastases, and internal organs. This leads to a deterioration in their performance:
- metastases in the lungs impair blood oxygen saturation;
- brain metastases cause seizures, personality changes, and impaired movement and/or sensation in the limbs. Daughter tumors in the brain stem lead to disturbances in breathing, heartbeat, and maintaining normal blood pressure levels;
- metastases in the bones cause severe pain, bone destruction, difficulty in movements - up to their complete impossibility;
- metastases to the liver lead to indigestion, yellowing and itching of the skin, and deterioration of brain function;
- metastases to the skin cause pain.
When neoplasia is detected by the body's immune system, intoxication develops. It manifests itself as weakness, loss of appetite, drowsiness, and nausea. A person stops eating normally, and the body does not receive the nutrients it needs for life and to fight the tumor.
Over time, cancer cachexia develops - exhaustion. It is manifested by weight loss, constant weakness, and lack of appetite. Cachexia further worsens a person’s condition, disrupting metabolism and the functioning of all his internal organs.
Treatment: removal or observation?
Benign neoplasms of the skin do not require removal, but surgery can be performed for aesthetic reasons, as well as in situations where the nevus is located in an open area of the body, is exposed to ultraviolet radiation, or is injured by parts of clothing or jewelry.
Removal of benign black moles that are not melanoma-dangerous is carried out in the following ways:
- Surgical removal;
- cryodestruction;
- electrocoagulation;
- radio wave removal;
- laser removal.
Melanoma-dangerous nevi can only be removed surgically. The operation is performed in the presence of an oncologist and involves healthy skin. The removed tissues are necessarily sent for histological examination. Melanoma-dangerous nevi can also be removed in aesthetic medicine clinics if the medical institution has a dermatologist oncologist on staff. The operation is performed in a classical way; cryodestruction and other modern technologies are not used.
If malignant degeneration of the neoplasm is diagnosed, complex antitumor therapy is indicated, which includes surgical removal with wide coverage of adjacent tissues, radiation and chemotherapy.
Treatment of the disease
At Euroonko, non-pigmented melanoma is treated according to modern protocols, taking into account the stage of the process:
- In stage I of the disease, surgical removal of the tumor and tissue around it is performed.
- In stage II, the tumor is removed and the lymph nodes are additionally checked for cancer cells. If mutated melanocytes are found in the lymph nodes, the nodes are removed. Treatment may include photodynamic therapy and radiation therapy. Here, if there is a mutation in the BRAF gene, treatment is carried out with BRAF inhibitors.
- Stage III is treated by removing the tumor and all nearby lymph nodes. Treatment is complemented by chemotherapy and radiotherapy. Immunotherapy and the introduction of BRAF inhibitors are involved. Therapy is required to improve the condition and relieve symptoms.
- At stage IV, large tumors and metastases are removed, if necessary. Chemotherapy, radiotherapy and palliative treatment are prescribed. Immunotherapy is mandatory.
Modern treatment of melanoma includes such a new and very promising direction as immunotherapy. And if previously only chemotherapy was carried out, which was successful only in 10% of cases, now the concept has changed greatly for the better. Immunotherapy involves the administration of special drugs that bind to certain proteins on the membranes of lymphocytes and “show” them that there are cancer cells in the body. Then the lymphocytes start working again and destroy them - throughout the body, and not locally.
Immunotherapy helps the body fight cancer. Even with advanced forms of malignant melanocytic tumor, patients can count on successful treatment.
For amelanotic melanoma containing a BRAF gene mutation, Euroonko provides targeted therapy with BRAF inhibitor drugs. These drugs suppress tumor progression and enhance immune activation. BRAF inhibitors are used starting from stages IIC-III. They increase long-term survival and are recommended for use even with an inoperable tumor or the presence of distant metastases.
Therapy with BRAF inhibitors is carried out for a long time - 6-9 months.
Treatment of melanoma: what will happen with delayed examination and treatment?
When analyzing methods of treating melanoma, it is indicated that surgical treatment is the basis. However, you should know that only rapid diagnosis and radical action, that is, removal of the entire lesion, can determine the effectiveness of treatment. The basis for the treatment method is an excisional biopsy, which determines the malignancy of the tumor. The lesion is excised along with the edge of healthy tissue.
In special cases, re-treatment is carried out, during which the original lesion site is cut off. A sentinel lymph node biopsy is also performed to assess the severity of the disease. The selection of the sentinel node is made taking into account the location of the original lesion.
Excision of the lesion and histopathological result allow the selection of appropriate treatment. As a rule, if the lesion has been removed and the correct margin has been preserved, and lymphadenectomy has been performed, that is, removal of the lymph nodes, then there is usually no indication for further treatment, but it is necessary to be under constant medical supervision.
Metastases associated with melanoma can appear even several years after surgery to remove the primary lesion. The risk of metastases, as well as the time at which they may appear, depend on several factors, the most important of which is the thickness of the primary lesion.
Melanoma metastasis
Prognosis and prevention
The prognosis of the disease depends on its size and the number of metastases. Thus, with a tumor thickness of less than 0.75 mm, non-pigmented melanoma is completely cured. If the tumor extends to 0.75-1.6 mm in thickness, the 5-year survival rate is about 85%. The nodular form of the tumor has a poor prognosis due to its rapid progression.
Prevention consists of protection from ultraviolet radiation - clothing, sunscreen, avoiding sunbathing. If there have been cases of skin cancer in the family, or the person has risk factors for melanoma, the presence of mutations in individual genes can be determined. If the result is positive, you will have to be extremely careful when tanning, avoid skin injuries and, in particular, damage to pigment formations.
| Read more about dermatological research at Euroonko | |
| Consultation with a dermatologist-oncologist | from 5,100 rub. |
| Skin examination using the German FotoFinder device | RUB 13,400 |
| Diagnosis of melanoma | from 5,100 rub. |
Book a consultation 24 hours a day
+7+7+78
Literature
- Fernanda Teixeira Ortega, Rogério Nabor Kondo and etc. Primary cutaneous amelanotic melanoma and gastrointestinal stromal tumor in synchronous evolution // An Bras Dermatol. 2022, Sep-Oct; 92 (5)
- Kubanov A.A., Gallyamova Yu.A., Bisharova A.S., Sysoeva T.A. Features of diagnosing amelanoma // Attending physician, No. 8, 2018.
- Snarskaya E.S., Avetisyan K.M., Andryukhina V.V. Pigmentless nodular melanoma of the skin of the leg // Dermato-oncology, No. 2, 2014.
- Lemekhov V.G. Epidemiology, risk factors, screening for skin melanoma // Practical Oncology, No. 4, 2001.
- Melanoma of the skin. Clinical recommendations of the Ministry of Health of the Russian Federation. 2022 approval year.
- Zhapekova Zh.A. Genetic predisposition to melanoma. Materials of the IX International Student Scientific Conference, 2017.
- Queirolo P., Spagnolo F., BRAF plus MEK-targeted drugs: a new standard of treatment for BRAF-mutant advanced melanoma, 2022.
How to recognize melanoma?
To diagnose melanoma, it is necessary to carry out very extensive diagnostics. Of course, the basis is the medical interview conducted during the first visit. The information obtained from the patient concerns mainly information about the condition of the skin, with particular emphasis on changes in moles on the skin or the appearance of new ones.
Information regarding factors that have been identified as increasing the risk of melanoma is also very important to the dermatologist. This group usually includes sunburn or the use of tanning beds. It is also very important for the doctor whether there have been cases of skin melanoma in the patient’s family.
An in-depth interview is the basis for further action. The most important element of diagnosis is the skin examination, which the dermatologist performs during the visit.
What do benign moles look like?
It is not difficult to notice moles on the body.
It is much more difficult to determine the types of neoplasms on your own, since some nevi do not have specific manifestations.
Classic signs of a benign mole:
- smooth/rough surface
- symmetry
- brown/black shade
- small size
- absence of dots inside the mole
- no tendency to growth and inflammation
It doesn't hurt, doesn't itch, doesn't itch.
Even harmless moles can become a source of mortal danger
Most often, melanoma occurs in the cells of borderline or epidermal-dermal moles. The cells that form the skin pigment – melanocytes – undergo malignant degeneration. Most often, skin cancer and melanoma occur in people aged 50-60 years, but in recent years cases of the disease have been reported even in young children. Especially often, malignant processes occur in the tissues of moles that are constantly squeezed or injured (by a razor, bra, clothing belt, etc.). It is advisable to remove such nevi for preventive purposes.
What complications may arise after mole removal?
If the scar hurts after removing a mole, a relapse is possible.
This happens in cases where, during surgery, not all melanocytes were eliminated; new birthmarks begin to form from the smallest particles remaining.
If moles grow again, they may need to be removed again.
If the wound becomes infected during the postoperative period, the following symptoms may occur:
- increased feeling of itching, weeping
- bleeding
- purulent contents are released from the wound
- the place of the mole is swollen and hurts
- swelling of surrounding tissues (lasts more than three days)
- increase in body temperature (over 38 degrees)
Preparation for dermatoscopy of moles, disadvantages and advantages of the method
The analysis does not require special preparation from the patient, the study is absolutely painless.
The only relative disadvantage is that dermatoscopy subjectively evaluates the appearance of blackheads.
The result largely depends on the experience of the medical expert.
However, a modern dermatoscope with the ability to connect to a computer allows you to share the results with other doctors.
This increases the likelihood of correct diagnosis and accurate diagnosis.
Special computer programs are being developed that should facilitate the differentiation of benign and dangerous lesions of the epidermis.
Dermatoscopy is a simple, non-invasive and widely available diagnostic method.
Does not expose the patient to harmful radiation and provides valuable information for the evaluation of skin lesions of unknown origin.
However, the most informative method for diagnosing moles/nevi remains histopathology (histology).
Histopathological examination represents the gold standard for diagnosis in dermatology.
Dermatoscopy is an additional tool that allows you to assess the condition of the epidermis.
It should be taken into account that the effectiveness and information content of this method also depends on the specialist - the diagnostic accuracy of dermatoscopy correlates with the doctor’s experience.