For the development of the disease, it is necessary not only to enter the pathogen, but also to have factors that contribute to the further proliferation of the fungus:
- deep skin folds of the feet;
- changes in the chemical composition of sweat;
- endocrine disruptions;
- hyperhidrosis;
- leg skin injuries;
- vegetative-vascular dystonia.
After fungi enter the skin, they can remain in saprophytic form for a long time without causing clinical symptoms. Athlete's disease is characterized by several variants of its course, some of which involve the spread of the process to the nail plate.
Causes
The main causes of athlete's foot:
- infection with the fungus Trichophyton mentagrophytes, which is the causative agent of athlete's foot;
- transmission is flexible through common objects;
- fungal infection in baths, swimming pools, saunas, gyms, showers;
- increased sweating of the feet;
- narrowed interdigital spaces;
- alkaline sweat reaction;
- flat feet.
The fungus gets onto the insoles of shoes, as well as into shower mats and washcloths, where it grows for a long time, since a warm and humid climate is the optimal environment for it.
The development of the disease is facilitated by diseases such as:
- trophic disorders of the lower extremities;
- varicose veins with chronic venous insufficiency;
- atherosclerosis;
- peripheral vascular thrombosis;
- vegetative-vascular dystonia;
- polyneuropathy.
Dermatophytosis
Dermatophytosis of the feet
Damage to the skin of the feet caused by dermatophytes and some other fungi. The disease is manifested by erythema, peeling and keratinization, the formation of vesicles and blisters. Synonyms: tinea pedis, epidermomycosis of the feet, rubrophytosis of the feet, athlete's foot. Classification Interdigital dermatophytosis It occurs most often. It can be acute (the so-called intertriginous form) and chronic (squamous form). The squamous form usually occurs unnoticed by the patient. Plantar dermatophytosis The causative agent is usually Trichophyton ru-brum. People suffering from allergic diseases are more likely to get sick. Characteristic signs are peeling and keratinization, which is why this form of dermatophytosis of the feet is also called squamous-hyperkeratotic. Dyshidrotic dermatophytosis is less common than others. The most common pathogen is Trichophyton mentagrophytes. Characterized by severe inflammation, the formation of vesicles and blisters. The pathogenesis is similar to allergic contact dermatitis (reaction to dermatophyte antigens). Epidemiology and etiology Etiology In chronic cases, the most likely pathogen is Trichophyton rubrum; in acute cases, Trichophyton mentagrophytes. Interdigital dermatophytosis. Dermatophytes: Trichophyton mentagrophytes var. interdigitale, Trichophyton rubrum, Epidermophyton floccosum. Other fungi: Candida albicans, Scytalidium hyalinum, Hendersonula toraloidea. Plantar dermatophytosis. Trichophyton rubrum (the most common pathogen, especially in people suffering from allergic diseases) and Epidermophyton floccosum. Dyshidrotic dermatophytosis. Trichophyton mentagrophytes var. mentagrophytes (the most common pathogen). Deep dermatophytosis. Dermatophytes: Trichophyton rubrum, Epidermophyton floccosum, Trichophyton mentagrophytes. Other fungi: Candida albicans. Age 20-50 years. The disease often begins in teenagers or young adults. Gender Men get sick more often. Risk factors Hot humid climate, closed shoes, sweating. Infection Walking barefoot on a contaminated surface. In human skin scales, spores of pathogenic fungi remain viable for more than 12 months. Course From several months to many years. Complaints: Itching. If a bacterial infection occurs, there will be pain. There may not be any complaints. Physical examination Skin Elements of rash
- Interdigital dermatophytosis. Maceration, peeling, detachment of the epidermis, cracks, weeping, redness of the skin.
- Plantar dermatophytosis. Redness with clear boundaries and small papules at the edges, floury peeling, keratinization. The lesion is limited to the heel, covers the entire sole or extends to the lateral surfaces of the foot.
- Dyshidrotic dermatophytosis. Vesicles and blisters containing clear liquid. The presence of pus indicates superinfection with Staphylococcus aureus. After opening of the vesicles and blisters, erosions with uneven, scalloped edges are formed.
- Deep dermatophytosis. Rashes characteristic of interdigital dermatophytosis spread to the sole and dorsum of the foot. Typically, a bacterial infection is also present.
Color. Red. The scales are white. Localization. Both feet are affected, less often one foot. Interdigital dermatophytosis. Favorite localization is the space between the little finger and the fourth finger. In addition to the interdigital spaces, adjacent areas of the foot may be affected. Plantar dermatophytosis. The sole and lateral surfaces of the foot (the upper border seems to correspond to the edge of a ballet shoe). Dyshidrotic dermatophytosis. Sole, medial surface of the foot, interdigital spaces.
Additional studies Sowing on media for fungi Dermatophytes are detected in 31% of patients with affected interdigital spaces and in 11% of patients without signs of interdigital dermatophytosis. Possible mixed infection (dermatophytes plus Candida spp.). Diagnosis Detection of fungal hyphae when scraping from the skin. Course and prognosis The disease is characterized by a chronic course with exacerbations in hot weather. The affected skin serves as a gateway for bacterial infections; Lymphangitis, erysipelas and phlegmon are common. These complications are especially common in those patients who have undergone surgery on the saphenous veins of the legs (for example, taking a fragment of a vein for coronary bypass surgery). Prevention Primary prevention. In public baths, swimming pools and even at home, you should wear slippers when taking a shower. Patients with diabetes and people who have undergone surgery on the saphenous veins of the legs should be especially careful due to the high risk of complications. Important: timely contact with a dermatovenerologist reduces the risk of complications.
Dermatophytosis of the hands
Dermatophytosis of the hands is chronic and is often combined with dermatophytosis of the feet. Often only one hand is affected (in right-handed people, the right hand). Synonym: tinea manus. Epidemiology and etiology Etiology The same pathogens as for dermatophytosis inguinalis and dermatophytosis of the feet. Most often - Trichophyton rubrum, Trichophyton mentagrophytes and Epidermophyton floccosum. Infection The disease often occurs against the background of dermatophytosis inguinalis and dermatophytosis of the feet. Course: From several months to several years. Complaints: Itching. With cracks and bacterial superinfection - pain. Dyshidrotic dermatophytosis of the hands is characterized by attacks of itching. Physical examination Skin Elements of rash
- Dyshidrotic dermatophytosis. Papules, vesicles, and occasionally blisters (at the edges of the lesion).
- Squamous hyperkeratotic dermatophytosis. Well-defined scaly lesions and erythema; keratinization and peeling in the palmar folds; cracks on the palms. The lesions have clear boundaries, healing begins from the center. On the dorsum of the hands there are papules, nodes, pustules (folliculitis caused by dermatophytes).
Color. Red. Form. Ring-shaped or polycyclic (especially on the dorsum of the hands). Localization. Uniform keratinization of the palms, especially noticeable in the palmar folds, or individual scaly lesions on the dorsum and lateral surfaces of the fingers. In half of the patients, only one arm is affected. The disease is often combined with dermatophytosis of the feet, inguinal dermatophytosis and onychomycosis of the hands. Additional research Sowing on fungal media. Diagnosis Diagnosis is made based on the clinical picture, confirmed by microscopy or culture results. Course and prognosis The course is chronic. Relapses occur until concomitant onychomycosis or dermatophytosis of the feet is eliminated. Cracks and erosions serve as gateways for bacterial infections. Prevention To prevent relapses, it is necessary to cure concomitant dermatophytosis of the feet, inguinal dermatophytosis or onychomycosis (fungal infection of the nail plates).
Dermatophytosis inguinalis
Inguinal dermatophytosis is a subacute or chronic disease affecting the skin of the thighs, pubic and groin areas. Synonyms: tinea cruris, inguinal athlete's foot. Age Adults get sick. Gender Men get sick more often. Etiology of Trichophyton rubrum, Trichophyton mentagrophytes, Epidermophyton floccosum. Risk factors: Hot, humid climate, tight pants, obesity. Long-term treatment with topical corticosteroids. Infection Most cases of dermatophytosis inguinalis occur in patients with tinea pedis. The infection is transmitted through the hands of the patient. Course: From several months to several years. Past diseases A history of dermatophytosis of the feet and dermatophytosis inguinalis is often present. Complaints As a rule, there are no complaints. Some patients consult a doctor because of itching. Physical examination Skin Dermatophytosis inguinalis is usually associated with tinea pedis and onychomycosis of the feet. Elements of the rash. Large scaly plaques with clear boundaries. Healing begins from the center. Color. Reddish, yellow-brown, brown. Form. Arc-shaped, polycyclic. Localization. Groin area and thighs. May spread to the buttocks. The scrotum and penis are rarely affected. Additional research Examination under Wood's lamp, sowing on mushroom media. Diagnosis Clinical picture confirmed by microscopy results. Course and prognosis Until concomitant dermatophytosis of the feet is cured, the disease recurs in 20-25% of patients. Prevention To prevent relapses, it is necessary to achieve cure of concomitant dermatophytosis of the feet and onychomycosis. In public baths, swimming pools and at home, when taking a shower (especially if other family members are sick), you should use slippers. Treatment of the feet and groin area with powder with antifungal components.
THERE ARE CONTRAINDICATIONS. YOU SHOULD CONSULT WITH A SPECIALIST.
Symptoms of athlete's foot
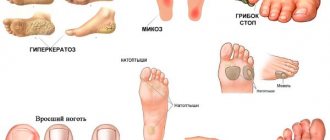
Currently, there are five types of athlete's foot, including squamous, intertriginous, dyshidrotic athlete's foot, erased and athlete's foot.
Forms can flow into one another or be combined. Among the main symptoms of the disease are the following:
- allergic rashes;
- reddish plaques with whitish peeling on the skin of the arch of the foot;
- yellow calluses with cracks on the surface;
- painful itching;
- swelling of the skin;
- erosion;
- inflamed small blistering rashes;
- cracks;
- fragility and rejection of the nail plate;
- bloody and purulent discharge.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
Diagnostic measures
With such problems, the patient should seek professional medical help from a mycologist. During the appointment, the doctor will conduct tests such as:
- Dermoscopic examination
- Scanning a surface using a special type of luminescent equipment.
- Skin pH assessment.
- Scraping test.
- Sowing to check the nutrient medium.
In addition, the expert can refer the patient for a consultation with colleagues in the orthopedic, phlebological, endocrinological and other departments.
Treatment of athlete's foot
Treatment of athlete's foot is carried out in two main stages:
- removal of scales of hyperkeratic layers;
- relief of acute inflammation in dyshidrotic and intertriginous athlete's foot;
- use of keratolytic drugs;
- taking anti-inflammatory and antihistamine drugs;
- surgical removal of a nail affected by fungus;
- after removing the nail, the bed is treated with antimycotic compounds;
- in advanced cases, the patient is recommended to take antifungal drugs.
List of sources
- Sergeev A. Yu., Sergeev Yu. V. Fungal infections (a guide for doctors). M., 2003. 185–193.
- Leshchenko V. M. Fungal skin diseases. In the book: Skin and venereal diseases (a guide for doctors). Ed. Yu. K. Skripkina, V. N. Mordovtseva. M., 1999. T. 1. P. 257–311.
- Sergeev V.Yu., Sergeev A.Yu. Dermatophytes: new in the diagnosis, therapy and prevention of the most common human mycoses. Consilium medicum. – Dermatology. – 2008. – No. 1. – P. 30–35.
- Haldin A.A., Sergeev V.Yu., Izyumova I.M. Modern ideas about inguinal dermatophytosis: etiology, epidemiology, clinical picture and effective therapy. Ross.zhur. leather and veins Bol. – 2005. – No. 5. – S. 43–48.