What it is? Terms and Definitions
Skin mycoses
– fungal infections of the skin and its appendages (hair, nails) by pathogenic fungi of various types. In fact, this is a large group of diseases united by a single criterion - the causative agent. Mycoses can manifest themselves in different ways, affecting only the skin or its appendages, some can simultaneously cause systemic lesions, that is, extend their effect to internal organs. Approaches to the treatment of different mycosis also differ: some require the use of local, topical drugs, such as ointments or creams for mycosis, some are supplemented with tablets for mycosis, oral forms of systemic drugs, in some cases doctors are forced to expand the range the drugs used against mycosis in order to first stabilize the patient’s condition and then rid him of the pathogenic fungus.
List of drugs
When choosing drugs for fungus, it is necessary to focus on effectiveness, the presence of side effects, symptoms and course of the disease. It is important to take into account individual intolerance to the components.
Antifungal antibiotics
If the fungal infection is systemic in nature, an integrated approach is required. Deep tissue damage, separation of the nail plates and severe itching of the skin against the background of deteriorating general health suggest the use of not only local remedies, but also tablets.
Among external remedies, it is worth highlighting medications that contain naftifine. This component has an antibacterial and anti-inflammatory effect. When taken regularly and in combination with other therapeutic agents, recovery occurs quickly.
Preparations with naftifine:
| Exostat solution 1% 15ml |
| Mycoderil cream 1% 15g |
| Exoderil cream 1% 15g |
External preparations for dermatomycosis and keratomycosis
Yeast, mold and dimorphic fungi can be cured with Terbinafine-based products. Popular drugs with this active ingredient:
| Lamicide drops for nails 15ml |
| Lamicide spray for legs 15ml |
| Lamisil cream 1% 15g |
| Fungoterbin 1% 15g |
| Exifin gel 1% 15g |
| Terbizil cream 15g |
| Terbix cream 1% 10g |
| Exiter cream 1% 15g |
Medicines containing ketoconazole effectively fight fungal infections of the head and groin area. List of drugs:
| Shampoo Sulsen forte 250ml ketoconazole |
| Shampoo Sulsen mite for dandruff 1% 250ml |
| Sulsen forte paste 2% 75g ketoconazole |
| Sulsen mite paste 1% 75g |
| Shampoo Sulsen mite for dandruff 1% 150ml |
| Shampoo Sulsen forte from perch 150ml |
| Nizoral cream 2% 15g |
| Mycozoral ointment 2% 15g |
| Sebozol shampoo 100ml |
Products based on miconazole, a synthetic substance with an antifungal effect, are effective against dermatomycetes and yeast, as well as the causative agent of lichen versicolor. Preparations containing miconazole:
| Mykozon cream 2% 15g |
| Ginocaps vag caps x 10 |
Antifungal agents for systemic candidiasis
The Candida fungus spreads inside the body: on the respiratory system, in the digestive system, on the genitals. Sometimes it infects the nervous and cardiovascular systems.
Often, with systemic candidiasis, the fungus also affects external tissues - nail plates, skin on the legs and arms. To get rid of the disease, it is important to start therapy in a timely manner. To treat candidiasis, drugs containing clotrimazole are used.
Popular remedies for the treatment of mycotic diseases caused by the Candida fungus:
| Flucorem 0.5% gel 15g |
| Kanizon plus cream 15g |
| Kanizon cream 1% 20g |
| Candide cream 15g |
| Clotrimazole-Akrikhin ointment 1% 20g |
| Clotrimazole-Akos ointment 1% 20g |
| Candide B cream 15g |
| Candiderm cream 15g |
Epidemiology
Fungal infections of the skin and nails
is a common global problem. The high prevalence of superficial fungal infections indicates that 20–25% of the world's population has mycoses of the skin, mycoses of the trunk, and mycoses of the feet, making them one of the most common forms of skin infections. Their distribution depends little on the average temperature or humidity in a particular country, geographical location and other reasons. Mainly - from background or previous diseases, from the state of immunity, including local, from previous treatment, especially antibacterial drugs, from age, personal and public hygiene and some other factors.
Diagnosis and treatment
Self-medicating in this situation is dangerous. Recognizing a fungal disease at the very beginning of the disease is possible only with timely contact with specialists involved in the treatment of affected organs or systems (gynecologists, gastroenterologists, etc.) or mycologists - specialists in fungal infections. Mycological studies make it possible to clarify the nature of the disease and distinguish a fungal disease from a bacterial one.
The doctor will select special antifungal drugs of a new generation, prescribe general strengthening procedures and multivitamin complexes. Enzymes that improve the functions of the digestive system, regulators of intestinal microflora, choleretic agents and medications that protect the liver are often prescribed.
Photo: fahroni / freepik.com
Along with antifungal treatment, much attention is paid to a special “antifungal” diet. This diet involves avoiding foods rich in carbohydrates, since impaired carbohydrate metabolism leads to increased blood sugar levels, and sugar is an excellent environment for mushrooms. Pasta, cereal dishes, as well as anything prepared with yeast are not recommended: beer, kvass, champagne, buns, pastries, cakes. Even bread can only be eaten today, since mold may begin to grow in it on the second or third day.
In order to relieve the liver while taking potent drugs, doctors recommend abstaining from fatty meat (pork, lamb, smoked meats, rich broths, fried foods, as well as duck and goose meat). You can leave veal, beef, chicken, boiled or stewed fish in your diet. It is recommended to consume vegetables, low-fat cottage cheese and sour cream, as well as fermented milk products - kefir and acidophilus.
Causes of the disease
Cause of mycoses
– various pathogenic fungi that can live both on the skin (feet, legs, hands, arms, head, torso) and on its appendages (scalp hair, body hair, fingernails and toenails).
In the host's body during mycosis, various pathological changes occur both due to the presence of the infectious agent and due to the products of its metabolism. All mycoses can be divided into three categories:
| Type of mycosis | Pathogen | Occurrence |
| Dermatophytosis Ringworm of the scalp, skin and nails | Dermatophytes (Arthroderma, Lophophyton, Microsporum, Nannizzia, Trichophyton, Epidermophyton) | Regular |
| Candidiasis of the skin, mucous membranes and nails | Candida, Debaryomyces, Kluyveromyces, Meyerozyma, Pichia, etc. | Regular |
| Dermatomycosis | Nondermatophytic forms of Neoscytalidium, Scopulariopsis | Rare |
Ecology of common human dermatophyte species:
| Kinds | Natural habitat | Occurrence |
| Epidermophyton floccosum | People | Regular |
| Trichophyton rubrum | People | Frequent |
| Trichophyton interdigitale | People | Frequent |
| Trichophyton tonsurans | People | Regular |
| Trichophyton violaceum | People | More rare |
| Trichophyton concentricum | People | Very rare |
| Trichophyton schoenleinii | People | Very rare |
| Trichophyton soudanense | People | Very rare |
| Microsporum audouinii | People | More rare |
| Microsporum ferrugineum | People | More rare |
| Trichophyton mentagrophytes | Mice and other rodents | Regular |
| Trichophyton equinum | Horses | Very rare |
| Trichophyton eriotrephon | Jerzy | Very rare |
| Trichophyton verrucosum | Cattle | Very rare |
| Microsporum canis | Cats | Regular |
| Nannizzia gypsea | The soil | Regular |
| Nannizzia nana | Soil, pigs | Very rare |
| Nannizzia fulva | The soil | Very rare |
| Nannizzia persicolor | Voles and bats | Very rare |
| Lophophyton cookei | The soil | Very rare |
| Lophophyton gallinae | Chickens and other poultry | Very rare |
Causes of mycosis:
The reasons for the increase in incidence are associated with the frequent use of hormonal anti-inflammatory drugs, antibiotics, hereditary factors and occupational risks. The risk of infection increases with the presence of cracks and defects in the skin and high humidity of the skin of the feet. Infection can occur in crowded places with high humidity; classic examples are swimming pools, baths and showers. The listed factors contribute to the development of the disease only if there is a fungus on the skin . Therefore, preventing its occurrence with the help of special drugs reliably protects a person from the disease even in unfavorable external conditions. One of the effective means for preventing infection is “Mikospray” .
Transmission routes
The main source of infection is humans
.
The main route of transmission is contact
. Activation of opportunistic flora is also possible when problems with the immune system occur. Fomites, that is, objects contaminated with pathogenic fungi, can be household items, shoes, clothing, and bedding of the sick person, if people who are sensitive to this fungus actively come into contact with them. Outbreaks are possible in organized groups, mainly in children's and army groups. Among public places, swimming pools, water parks and other structures where people can be barefoot inside are considered a common variant of fungal infection, plus a warm and humid microclimate is formed there, which contributes to the long existence of the pathogen outside the host.
In rare cases, for example, with microsporia, the source of infection can be a street or domestic animal, most often a cat. In common parlance, this disease is called “lichen.” “Ringworm” or, more precisely, “ringworm” in a child is microsporia. It is also possible to become infected with trichophytosis through contact in rural areas with hay or other substrates on which the secretions of sick rodents remain.
Types of disease
In the vast majority of cases, varieties of mycoses are named by the name of the pathogen: trichophyton causes trichophytosis, microsporum causes microsporia.
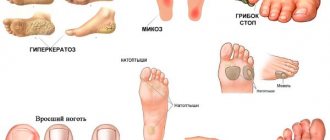
They differ primarily in their characteristic affected areas. Classification of mycoses:
| Type of mycosis | Affected area |
| Tinea pedis, athlete's foot | Feet |
| Tinea unguium, onychomycosis | Nails on fingers and toes |
| Tinea corporis | Skin of hands, feet and body |
| Tinea cruris, jock itch | Inguinal folds, armpits |
| Tinea manuum | Skin of the palms and back of the hands |
| Tinea capitis | Scalp |
| Tinea barbae | Scalp hair, including scalp and face |
| Tinea faciei | Skin on the face |
| Tinea versicolor, pityriasis versicolor, sun fungus | All skin |
Symptoms
The most common symptoms that lead to a visit to a doctor include nonspecific symptoms characteristic of the majority of mycoses. The following early signs may indicate this:
- Peeling and redness of the skin
- Itching, often unbearable
- Wetting in the folds of the skin
- Small vesicles (bubbles) that burst and dry on their own
Other symptoms of fungal diseases depend on the specific pathogen of mycosis.
Tinea pedis
There are four main clinical variants of tinea pedis; sometimes they overlap each other in manifestations. The most common variant is intertriginous, which is characterized by cracking, peeling, or maceration of the interdigital areas; unpleasant odor; itching; and a burning sensation. The infection often affects the lateral webbing of the toes and may spread to the sole or instep of the foot. Warm and humid conditions can worsen skin conditions. The second option is the chronic papulosquamous type, which often occurs on both feet. This type is characterized by mild inflammation and scattered peeling of the skin on the soles of the feet. The third option consists of small blisters or pustules on the instep and plantar surface. There is peeling of the skin in this area, as well as the membranes of the toes. The fourth option includes macerated, open, weeping ulcers on the sole of the foot with a characteristic odor. This option is often complicated by opportunistic gram-negative bacteria.
Tinea corporis
It can manifest itself in different ways and in different parts of the body. The lesions often appear as small, round, erythematous, scaly areas. In the center, cleansing occurs as the boundaries expand and vesicles or pustules develop. Tinea corporis can occur on any part of the body, depending on the type of dermatophyte infection. Animal-borne zoodermatophytes often infect exposed areas of skin, whereas anthropodermatophytes primarily infect closed or injured areas.
Tinea cruris
Jock itch occurs on the medial and upper thighs and groin area and is more common in men than women; the scrotum often remains intact. Symptoms such as unbearable itching, a feeling of constant weeping and burning are often present. Risk factors for this tinea pedis infection include tinea pedis infection, obesity, diabetes, and immunodeficiency.
Ringworm of the head
The exact incidence pattern of this form is unknown, but it most often occurs in children who come into contact with other children or pets. There are three types of tinea capitis: blackhead, gray spot and favus. Trichophyton often causes black dotted dermatitis on the scalp and is the predominant variant. Gray spotted dermatophytosis on the head occurs in epidemic and endemic forms, but the epidemic form is practically not registered in developed countries. The endemic form, caused by Microsporum, is often spread by cats and dogs. Favus, more common in Eastern Europe and Asia.
The blackhead variant is often asymptomatic at first. The erythematous scaly patch on the scalp enlarges over time and localized alopecia occurs. The hairs inside the spots break and a characteristic black dot appears (caused by the accumulation of detritus in the opening of the follicle). If left untreated, blackhead fungus can cause alopecia and scarring to become permanent. Sometimes the affected area may change and become raised, painful, severely inflamed, with nodules known as kerions. Kerion formation occurs due to an immune response to the fungus. Lymphadenopathy may occur when kerion occurs. The variant with gray plaques on the scalp consists of round patches of alopecia with noticeable flaking. Kerion formation can also occur in this case.
Onychomycosis
This type of mycosis is most often caused by dermatophytes, but it can also be caused by non-dermatophytes and Candida species. Affected nails often become thick, rough, yellow, opaque, and brittle. The nail may separate from the nail bed, and the dermis surrounding the infected nail may be hyperkeratotic. Risk factors include diabetes, trauma, family history, athlete's foot, smoking, prolonged exposure to water, and immunodeficiency.
Diagnostics
The diagnosis is confirmed by the detection of segmented hyphae in skin scrapings from the affected area with potassium hydroxide (KOH). When bubbles form, the top of the bubble can serve as an adequate sample. Alternative diagnostic procedures are dermatophyte culture test medium and culture method.
Patients who have significant erosion, ulceration, or malodor in the affected area should undergo Gram staining and culture to evaluate for secondary bacterial infection.
Differential diagnosis depends on clinical subtype:
Interdigital dermatitis of the foot
- Erythrasma
- Interdigital candidiasis
- Hyperkeratotic (moccasin) dermatitis of the foot
- Atopic dermatitis
- Chronic contact dermatitis
- Chronic palmoplantar (dyshidrotic) eczema
- Palmoplantar psoriasis
- Pitted keratolysis
- Juvenile plantar dermatosis
- Exfoliating keratolysis
- Keratoderm
Inflammatory dermatosis of the foot
- Acute palmoplantar (dyshidrotic) eczema
- Acute contact dermatitis
- Palmoplantar pustulosis
- Scabies
A positive KOH test demonstrating segmented hyphae distinguishes Tinea pedis from nonfungal diseases. With interdigital candidiasis, a test with the drug KOH will show budding yeast, pseudohyphae and hyphal septa.
Treatment and drugs
Treatment of mycoses
recommended to relieve symptoms (itching), reduce the risk of secondary bacterial infection, and limit the spread of infection to other areas of the body or to other people. Local antifungal therapy is the treatment of choice for most patients. Systemic antifungals are primarily intended for patients in whom topical therapy has failed. Also, systemic therapy comes to the fore for Tinea capitis, Tinea barbae, Tinea imbricata.
Topical medications effective for dermatophytosis include azoles, allylamines, butenafine, ciclopirox, tolnaftate, and amorolfine. A meta-analysis of randomized trials published up to February 2005 supports the effectiveness of topical therapy, finding strong evidence of superiority of topical antifungals (azoles, allylamines, ciclopirox, tolnaftate, butenafine, and undecanoate) over placebo. Allylamines may be slightly more effective than azoles; a meta-analysis of data from 11 studies that compared topical allylamines with topical azoles found a slightly higher cure rate for allylamines (hazard ratio for treatment failure 0.63, 95% confidence interval 0.42–0.94). Topical antifungal treatment is usually applied once or twice daily and continued for four weeks. Shorter courses of treatment may be effective; high cure rates were obtained with the use of 1% terbinafine cream for interdigital foot dermatitis for one week.
Patients requiring oral antifungal therapy are usually treated with terbinafine, itraconazole, or fluconazole. Typical treatment regimens for adults include:
- Terbinafine: 250 mg daily for two weeks.
- Itraconazole: 200 mg twice daily for one week.
- Fluconazole: 150 mg once a week for two to six weeks.
Griseofulvin can also be used to treat mycoses of the skin, but is likely to be less effective than other oral antifungals and will also require a longer course of therapy. A systematic review found that terbinafine was more effective than griseofulvin, while the efficacy of terbinafine and itraconazole was similar. Typical adult doses of griseofulvin for tinea pedis are 1,000 mg griseofulvin (microcapsule) per day for four to eight weeks or 660 or 750 mg griseofulvin (ultramicrocapsule) per day for four to eight weeks.
The dosage for children is based on weight, and the duration of treatment is similar to that for adults. Typical pediatric dosages for oral therapy include:
Terbinafine tablets:
- 10 to 20 kg: 62.5 mg per day
- From 20 to 40 kg: 125 mg per day
- Over 40 kg: 250 mg per day
Terbinafine granules:
- Less than 25 kg: 125 mg per day
- 25 to 35 kg: 187.5 mg per day
- Over 35 kg: 250 mg per day
Itraconazole: 3 to 5 mg/kg per day.
Fluconazole: 6 mg/kg once a week.
Griseofulvin (microcapsules) 10 to 20 mg/kg per day or griseofulvin (ultramicrocapsules) 5 to 15 mg/kg per day.
The exact regimens should be selected by the attending physician in accordance with the type of lesion, pathogen and clinical variant of mycosis.
Patients with hyperkeratotic dermatitis of the foot may benefit from combining antifungal treatment with a topical keratolytic such as salicylic acid. Wet Burow dressings (1% aluminum acetate or 5% aluminum subacetate) applied for 20 minutes two to three times daily or gauze or cotton between the toes may be useful as an adjunctive measure for patients with vesiculation or maceration. Interventions that may help reduce relapses include using dehydrating foot powders, treating shoes with antifungal powder, and avoiding tight shoes.
Publications in the media
Fungal infections of the skin and its appendages have been known since ancient times. Doctors gave skin diseases with different symptoms from others separate designations (for example, favus), not yet knowing that they were caused by fungi. The history of the science of dermatophytes began with the discovery of the favus pathogen Achorion schoenleinii in 1839 by Schonlein JL. Schonlein found fungal mycelium in the skin rashes of a patient whom he had mistakenly diagnosed as having impetigo. In 1841, Grubi D. established the relationship between skin diseases and fungi. He described the clinical picture of microsporia and the morphological features of the fungus that causes this disease. As a result of the use of the special nutrient medium proposed by Sabouraud R. for the cultivation of mushrooms, favorable conditions were created for mycological researchers. Relevant clinical and laboratory studies began to be carried out, and the era of discovery of new types of pathogens began. In the field of medical mycology, significant changes have occurred in various directions: dermatophytes, molds, yeast-like fungi, the pathogenesis of mycotic infections were studied and described in detail, the nature of actinomycosis was determined, the treatment of fungal diseases was improved, etc. Russian scientists also made a significant contribution to the development of medical mycology , among whom the most famous are P. N. Kashkin, A. M. Arievich, N. D. Sheklakov, O. K. Khmelnitsky, A. N. Arabian, Z. G. Stepanishcheva, N. A. Krasilnikov, G. O Suteev, V. M. Leshchenko and many others.
Fungal diseases have long gone beyond the specialty of a dermatologist, but dermatologists-mycologists are still doing a lot of work to combat dermatomycosis, which ranks first in prevalence in all countries.
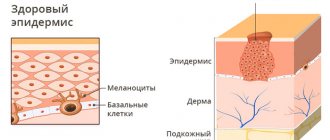
Superficial mycoses (dermatomycosis) include infections that affect the skin, nails and hair. The main pathogens are dermatophytes, fungi that can absorb keratin. These include fungi of the genera Microsporum, Trichophyton and Epidermophyton, which, depending on the source of infection, are divided into anthropophilic, zoophilic and geophilic. The habitat of zoophilic dermatophytes (Trichophyton mentagrophytes v. gypseum, T. verrucosum, Microsporum canis, etc.) is animals, anthropophilic (Trichophyton rubrum, T. mentagrophytes v. interdigitale, Microsporum ferrugineum, Epidermophyton floccosum, etc.) is human, geophilic species ( Microsporum gypseum) live in the soil. Dermatophytes are highly contagious and can be transmitted to humans from humans, animals or soil, causing disease. The main “spreaders” of infection are anthropophilic species.
Superficial mycoses also include keratomycosis: pityriasis versicolor and piedra, which affect the most superficial areas of the stratum corneum and hair cuticle. The causative agent of pityriasis versicolor and seborrheic dermatitis, the yeast-like fungus Malassezia furfur, lives on the skin of humans and animals and, under favorable conditions, can affect the stratum corneum of the epidermis and the mouth of the follicles. The disease in most cases is not contagious. White and black piedra are usually found in countries with hot and humid climates. The diseases are less contagious. The causative agent of black piedra, Piedraia hortae, is found only on hair. Trichosporon beigelii is widespread in the environment and, in addition to white piedra, can also cause skin and nail lesions.
In addition to true dermatophytes, which infect only the skin and its appendages, superficial mycoses can also be caused by other fungi, isolated from a variety of localizations during systemic mycoses. Candida spp. - the second most common discharge in dermatomycosis and onychomycosis after dermatophytes. Up to 40% of cases of onychomycosis of the hands are caused by Candida. Lesions of yeast-like fungi on the scalp with a clinical picture of seborrheic eczema were noted. Superficial forms of candidiasis also include lesions of the mucous membranes of the oral cavity and genital organs.
In cases of onychomycosis caused by molds, there is still doubt about the ability of these opportunistic pathogens to independently infect nails due to their weak proteinase and keratinase activity. It is known that mold fungi can manifest themselves as a secondary infection, penetrating into tissues already affected by dermatophytes. However, as a result of many years of research, it has been proven that some molds can penetrate into the intercellular nail space using perforating organs. The most common causative agents of mold lesions of the skin and nails are Scopulariopsis brevicaulis, Pyrenochaeta unguis-hominis, Aspergillus spp., Fusarium spp., Alternaria spp., Cladosporium spp. and etc.
There are numerous options for the classification of fungal infections, which to a greater or lesser extent take into account the etiology, pathogenesis, clinical picture and features of the epidemiology of diseases. In domestic dermatology, the classification of N. D. Sheklakov is most often used:
- Keratomycosis (lichen versicolor, piedra, imbricated mycosis).
- Dermatophytosis (athlete's foot, trichophytosis, microsporia, rubromycosis, favus, etc.).
- Candidiasis (superficial candidiasis of the skin and mucous membranes, visceral, etc.).
- Deep mycoses (chromomycosis, sporotrichosis, etc.).
- Pseudomycosis (erythrasma, actinomycosis, nocardiosis, etc.).
However, many countries around the world have adopted a classification of fungal diseases according to the localization of the pathological process:
- Tinea pedis - mycosis of the feet.
- Tinea corporis is a mycosis of the smooth skin of the trunk.
- Tinea cruris - inguinal mycosis.
- Tinea capitis is mycosis of the scalp.
- Tinea unguim - onychomycosis.
- Tinea manum - mycosis of the hands.
- Tinea barbae is mycosis of the face.
This classification is convenient from a practical point of view, but does not take into account the etiological features of dermatophytosis, which can determine the nature of epidemiological measures and treatment features.
Main clinical features of fungal infections
Mycoses of the feet (Fig. 1). The interdigital folds and soles are mainly affected. In the interdigital folds, slight peeling with minor inflammatory phenomena, moderate maceration, cracks, and blisters are observed. On the sole there is thickening of the stratum corneum, flour-like peeling in the skin grooves, small cracks on a slightly hyperemic background. In the dyshidrotic form, numerous blisters form on the skin of the arch and inferolateral surface of the foot, which then merge to form large blisters. In place of the opened blisters, erosions with an uneven edge remain.
Mycosis of smooth skin of the body (Fig. 2). With tinea versicolor, brownish and white spots are usually localized on the skin of the chest, back, neck and shoulders. Scaly lesions have clear boundaries and are not accompanied by inflammatory phenomena.
When the skin is damaged by other pathogenic fungi, clearly demarcated, round, swollen lesions with a raised ridge are formed. The center of the lesion is flattened, with slight peeling. The lesions increase due to peripheral growth.
Mycosis inguinal. Typical localization is the inner thigh, lower abdomen, buttocks. The lesions are clearly defined, scaly, erythematous, with an inflammatory ridge. Over time, the general moderately erythematous background gives way to a brownish one.
Mycosis of the scalp. Most often observed in children. The disease manifests itself as large, round, clearly demarcated, scaly patches of baldness. Inflammatory phenomena are mild. Discolored hair within the lesion is broken off a few millimeters above the skin level (with microsporia) or, breaking off at the skin level, leaves a stump in the form of a black dot (with trichophytosis). Zoophilic pathogens can cause the development of an infiltrative-suppurative form of dermatophytosis: the lesion protrudes above the surrounding skin, is covered with purulent-bloody crusts, and hair falls out.
Onychomycosis. Various types of fungal infection of the nail plates are characterized by loss of transparency, discoloration (whitish, yellowish), thickening, subungual hyperkeratosis, crumbling or destruction down to the nail fold.
Mycosis of the hands. In the squamous form of palm lesions, the disease manifests itself in fine-lamellar mealy peeling in the skin grooves. Cracks may form, accompanied by pain and itching. In the dyshidrotic form, vesicles form, which often cluster and can coalesce to form blisters.
Mycosis of the face. Most often, lesions are localized in the neck, chin and lower lip. The infiltrative-suppurative form of the lesion manifests itself in the formation of large bluish-red nodes with a bumpy surface. Numerous pustules merge to form abscesses. Changed dull hair in the lesion is removed easily and without pain. The superficial version resembles mycosis of smooth skin.
Laboratory diagnostics
Microscopy of clinical material is a quick and simple method for preliminary diagnosis of the disease. In cases where there is no growth of the pathogen in culture, a positive result of direct microscopy can be an undoubted confirmation of a mycotic infection. In scrapings from skin and nails, dermatophytes are usually represented by thin, 2–4 µm in diameter, straight and rarely branched mycelium. Often in the preparation one can find atypical forms of dermatophyte mycelium - chains of round arthrospores (Fig. 3).
M. furfur, when microscopy of skin scales, is revealed in the form of round cells with a diameter of 3–8 μm, collected in clusters, and short curved mycelial hyphae of a characteristic “banana-shaped” shape. In most cases, the diagnosis of lichen versicolor can be established precisely by microscopy of the native specimen, since culture of the material usually does not give results.
Scopulariopsis brevicaulis in nail scales is represented by characteristic cup-shaped spores with a rough shell.
Fungi of the genus Candida form typical budding yeast cells and pseudomycelia (branching chains of long cells).
Identification of other pathogens in native preparations is difficult.
When hair is damaged by dermatophytes, several tissue forms of the fungus are observed: 1) endoectothrix - spores with a diameter of 2–3 microns are “mosaic” located inside and mostly outside the hair, forming a muff on the root (“Adamson’s sheath”). Inside the hair you can also see mycelium, which, with light pressure on the preparation, comes out of the hair in the form of a fringe - “Adamson's brush”. The causative agent is Microsporum spp.; 2) endothrix - spores with a diameter of 4–6 microns are located inside the hair in longitudinal chains, completely filling it. The causative agent is Trichophyton spp. The final identification of fungi is carried out by cultural studies.
For cultural studies of pathological material, Sabouraud's medium with chloramphenicol and gentamicin is used, as well as for the selective isolation of dermatophytes - with cycloheximide (actidione), to inhibit the growth of fast-growing saprophytic fungi.
Dermatophyte genera are distinguished by the presence and morphology of multicellular macroconidia and unicellular microconidia.
Characteristics of the most important pathogenic fungi
Epidermophyton floccosum. Anthropophil. Affects the skin of the groin folds and legs. Colonies grow slowly, grayish-brown, lemon-olive, later white, folded-lumpy in the center. The surface of the colony is leathery or velvety-mealy. By microscopy: in mature cultures there are chains of intercalary chlamydospores. Macroconidia are 4–5-celled, club-shaped, smooth, with rounded ends. Arranged in bunches of 3–5 pieces. Microconidia are absent.
Microsporum canis (Fig. 4). Zooanthropophil. The most common pathogen of microsporia in Russia. Colonies are fast-growing, flat, radiant-hairy. The mycelium is grayish-white, against the background of a brownish-red or orange reverse side, the general hue of the colony is salmon. Under microscopy: it forms a characteristic bamboo-like mycelium, there are combs, short spirals, intercalary chlamydospores. Macroconidia are fusiform, pointed, spinous, multi-chambered (4–12 cells) with a distinct double-circuited shell. Microconidia are pear-shaped and occur inconsistently.
M. gypseum. Geophilic pathogen. It affects the skin and hair primarily of people who cultivate the soil. The colonies are fast-growing, flat, mealy (powdery), later with a small velvety elevation in the center. The color is yellowish-pink. The reverse side is yellow. Under microscopy: numerous macroconidia (4–6 cells) spindle-shaped, wide, blunt-ended, smooth. Microconidia, if present, are numerous and pear-shaped or oval.
Trichophyton rubrum (Fig. 5). Anthropophil. The most common causative agent of dermatomycosis. Affects toenails, hands and skin anywhere on the body.
The colonies are velvety, white, sometimes waxy at the beginning of growth; later they can acquire a pinkish or purple-red color. The reverse side is yellow, red or cherry red. Under microscopy: abundant microconidia of elongated, drop-shaped or pear-shaped are located on the sides of the mycelium. Macroconidia are 5–6-celled, blunt-pointed.
T. mentagrophytes var. interdigitale. Anthropophil. Affects the nail plates and skin of the feet.
Colonies are fast-growing, velvety, white, sometimes pinkish. With age, the colonies of different strains become fluffy or densely powdery. The reverse side is colorless or brownish. Under microscopy: microconidia are round, located on the sides of the mycelium, singly and in clusters. Cigar-shaped, 3–5-celled macroconidia with a rounded end are rare. In mature cultures there are many whorls and spirals, nodular organs and intercalary chlamydospores are formed.
T. mentagrophytes var. gypseum. Zooanthropophil. Affects skin and hair. In terms of frequency of isolation, it ranks second after T. rubrum.
Colonies are fast-growing, flat, granular-powdery, white, cream, yellowish. The reverse side is brownish-red. Under microscopy: microconidia are abundant, round, located on the sides of the mycelium singly and in the form of clusters. Macroconidia are cigar-shaped, 3–8 cells with rounded ends.
Treatment
Therapy for various mycotic lesions of the skin and nails is carried out with antifungal drugs, which can be systemic or applied externally. In practice, both monotherapy and various combinations of antifungal drugs are used. In most cases, treatment should be comprehensive using external antifungal agents, systemic drugs, and symptomatic treatment. Methods and means of topical therapy are mandatory components of the treatment of various mycotic skin lesions. If the fungal process is in the initial stage and there are minor skin lesions, then it can be cured by prescribing only external antifungal drugs. With a widespread or deep mycotic process, as well as in patients with damage to hair and nails, treatment may be difficult.
Antifungal drugs or antimycotics are specific agents used to treat fungal infections of the skin, nails, hair, etc. They may have fungicidal and fungistatic properties. The fungicidal effect of the antifungal agent leads to the death of fungal cells, while the fungistatic effect stops the formation of new fungal cells. Antimycotics are conventionally divided into 5 groups: polyene antibiotics, azole compounds, allylamine drugs, morpholine derivatives and medications without a clear relationship to any specific group.
When prescribing topical therapy, it is important to take into account the nature of the specific effect of the antifungal agent. It is known that griseofulvin preparations are active only against dermatophytes. External products containing polyene antibiotics - against yeast and mold fungi, preparations of selenium, zinc, benzyl benzoate - fungi of the genus Malassezia and the causative agent of erythrasma Corynebacterium minnutissium. Modern antifungal agents of the azole, allylamine, morpholine series, thiocarbamycins and pyridine compounds have a significantly wider spectrum of antifungal activity, as well as anti-inflammatory and antipruritic properties and are well tolerated.
Onychomycosis is the most treatment-resistant disease. The basis for success is an individually selected treatment regimen. When treating, it is necessary to take into account the patient’s age, concomitant diseases, the number of affected nails, and the degree of involvement of the nail plates in the pathological process.
Currently, mycologists have a large arsenal of agents with a wide spectrum of fungicidal action, accumulation in therapeutic concentrations in the nail plate and nail bed. The greatest preference is given to drugs that meet the requirements for therapeutic effectiveness, as well as aesthetics and ease of use.
Treatment of onychomycosis is divided into local, systemic, and combined.
Local treatment allows you to create high concentrations of the drug on the surface of the nail plate. However, the active ingredients of the antimycotic do not always penetrate into the nail bed, where the most viable fungi are located, in effective concentrations.
Local antimycotics: varnishes - Loceryl, Batrafen; creams - Lamisil, Nizoral, Mikospor, Mifungar, Travogen, Ecozax, Exoderil, Pimafucin, sprays - Daktarin, Lamisil, etc. It is necessary to take into account that they are not intended specifically for the treatment of onychomycosis, but they can be used in the treatment of fungal infections of the skin of the feet, interdigital gaps, often combined with onychomycosis.
To treat nails, local antiseptics are also used - alcohol solutions of iodine and dyes.
Multicomponent preparations contain an antimycotic or antiseptic in combination with an anti-inflammatory agent. In the treatment of skin infections accompanying onychomycosis, the following are used: Triderm, Travocort, Mikozolon, Pimafucort, Lorinden S, etc.
Azole, allylamine, morpholine compounds, as well as mixed group drugs are active against a large number of pathogens. Considering that quite often mycoses of the feet are caused by mixed fungal flora, it is preferable to prescribe these drugs, which are broad-spectrum antimycotics. Most of them damage the cytoplasmic membranes of fungal cell walls, suppressing the synthesis of their main components, in particular ergosterol.
Currently, the mycologist has highly effective systemic antimycotics: itraconazole (Sporonox, Orungal), fluconazole (Diflucan, Forkan), terbinafine (Lamisil), the antifungal effect of which is reflected in the table.
One of the important principles of topical therapy for mycotic skin lesions is the alternation of external antifungal drugs, which avoids resistance of dermatomycetes to them.
For squamous-keratotic forms of skin lesions, keratolytic agents are used as part of collodion peels or ointments: Arabian, Arievich, Andriasyan ointment or 5-10% Salicylic ointment. For candidal lesions, use Nystatin, Levorin, Amphotericin ointments, Pimafucin 1-2 times a day for 10-15 days. As a result of treatment, foci of candidal intertrigo, interdigital candidal erosions, and paronychia are resolved.
For acute skin mycoses with a pronounced inflammatory component, treatment begins with the elimination of swelling, hyperemia, exudation, eczematization, and allergic rashes. Lotions and wet-drying dressings with disinfectant and astringent compositions are prescribed: tannin, ethacridine, boric acid, etc. Then 2–5% boron-naphthalan paste, 5% ASD paste, as well as combinations of antifungal and corticosteroid agents in creams are used: Mycozolon, Travocort, Triderm. At the same time, acute inflammatory phenomena are quickly eliminated, which makes it possible to subsequently switch to treatment with fungicidal agents. It is recommended to use external agents with corticosteroids for 7–8 days to avoid activation of the mycotic process.
After acute inflammatory phenomena have subsided or after detachment of the stratum corneum in hyperkeratosis, azole antimycotic drugs can be used: Canesten, Clotrimazole, which are used 1 to 3 times a day, applying a thin layer to the lesions.
External dosage forms of terbinafine have high therapeutic activity: Lamisil (1% spray, cream), Lamisil Dermgel (gel). All forms have pronounced antimycotic and antibacterial properties. The presence of three dosage forms allows the mycologist to use the drug with the greatest benefit. Thus, Lamisil spray is indicated for acute mycoses with hyperemia, swelling, and rashes. The areas irrigated with the spray are covered with a thin film and isolated from the environment. Lamisil spray does not cause irritation and leads to a rapid resolution of mycosis areas: pain, itching, burning disappears, the lesions turn pale and dry out. With the help of Lamisil spray, foci of erythrasma are cured within 5 days. Within 7–10 days, recovery occurs in patients with various forms of lichen versicolor. Lamisil Dermgel, like the spray, is more indicated for acute mycoses, as it has a pronounced cooling effect and is easily applied to the affected areas. For erythematous-squamous and infiltrative manifestations of skin mycoses, the use of Lamisil in the form of a cream is indicated. The gel and cream of this drug are also effective for microsporia, lichen versicolor, candidiasis of large skin folds and periungual ridges. When using Lamisil cream for one week, a concentration of the drug is created in the skin that retains its fungicidal properties for another week after its discontinuation. This circumstance justifies short courses of treatment with Lamisil compared to other local antifungal agents.
Therapy for mycoses of the scalp, as well as in the treatment of smooth skin, is carried out with systemic and external antimycotics. Apply 2–5% tincture of iodine to the foci of mycosis and apply antifungal ointment in the evening. In cases of significant inflammation, combination drugs are used that contain, in addition to antimycotics, corticosteroid hormones. During an infiltrative-suppurative process, remove crusts with 2-3% Salicylic ointment and use disinfectant solutions (Furacilin, potassium permanganate). To increase the effectiveness of treatment, it is recommended to shave the hair on the head every 10 days.
I. V. Kurbatova , Candidate of Biological Sciences G. A. Plakhotnaya , Candidate of Medical Sciences
IMPiTM im. E. I. Martsinovsky, MMA named after. I. M. Sechenova
Prevention and hygiene
If anyone in your home has or has had a fungal skin infection:
- Get rid of combs, brushes, clips or other hair products that may have fungus on them. Do not use other things of the sick person that may have come into contact with his skin.
- Make sure your doctor checks everyone in the house for fungal infections.
- If the fungal infection may have been caused by a pet, contact your veterinarian.
Here are some more general tips to prevent fungal infections:
- Do not share unwashed clothing, sports equipment, or towels with other people.
- Always wear slippers or sandals when in the gym, swimming pool or other public places. This includes public showers.
- Wash with soap and shampoo after sports or exercise.
- Change your socks and underwear at least once a day.
- Keep skin clean and dry. Always dry yourself well after swimming or showering.
How to protect yourself from mold infection?
- Care must be taken when dismantling old, dilapidated dachas and when using stale building material. Fungi that have settled on a tree are especially dangerous.
- Although fungi on food products are less aggressive, nevertheless, a small spot of mold on bread must be carefully cut out, and if mold has appeared in several places, it is better not to eat the bread.
- Rotting places on an apple can be removed, but moldy juicy fruits and vegetables - tomatoes, pears, peaches, apricots, especially if mold has appeared around the seed - will have to be thrown away.
- Without hesitation, pour out compotes, juices and syrups with mold stains, but in confitures and jams with a high sugar content, it is enough to remove the top thick layer.
- You should not eat moldy nut kernels with a bitter, musty aftertaste. You should avoid cottage cheese and other moldy dairy products.
- Small spots of mold on the cheese can be removed, but if the mold has formed inside the head, it's not worth the risk. True, there are cheeses, for example, Roquefort, to which mold gives a special piquant flavor, but if you have a fungal infection, you will have to give up such a favorite delicacy for many gourmets for a while.
conclusions
Superficial fungal infections are most often caused by dermatophytes from the genera Trichophyton, Epidermophyton and Microsporum. These organisms metabolize keratin and cause a number of pathological clinical manifestations, including tinea pedis, dermatophytal dermatitis, dermatophytosis, etc. Based on clinical findings, the diagnosis of cutaneous dermatophyte infection can be strongly suspected. To confirm the diagnosis, potassium hydroxide should be used. Most dermatophyte infections can be managed with topical treatment. Examples of effective topical antifungal agents include azoles, allylamines, ciclopirox, butenafine, and tolnaftate. Oral antifungal therapy is used for widespread infections or infections that are resistant to topical therapy. Nystatin is not effective against dermatophyte infections.
List of literature / References
- Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide // Mycoses. 2008 Sep;51 Suppl 4:2-15. doi: 10.1111/j.1439-0507.2008.01606.x. Erratum in: Mycoses. 2009 Jan;52(1):95. PMID: 18783559.
- Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide // Mycoses 2008; 51 Suppl 4:2.
- Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections // Mycopathologia 2008; 166:335.
- Ameen M. Epidemiology of superficial fungal infections // Clin Dermatol 2010; 28:197.
- El-Gohary M, van Zuuren EJ, Fedorowicz Z, et al. Topical antifungal treatments for tinea cruris and tinea corporis // Cochrane Database Syst Rev 2014; :CD009992.
- Alston SJ, Cohen BA, Braun M. Persistent and recurrent tinea corporis in children treated with combination antifungal/ corticosteroid agents // Pediatrics 2003; 111:201.
- Greenberg HL, Shwayder TA, Bieszk N, Fivenson DP. Clotrimazole/betamethasone diproprionate: a review of costs and complications in the treatment of common cutaneous fungal infections // Pediatr Dermatol 2002; 19:78.
- Rosen T, Elewski BE. Failure of clotrimazole-betamethasone dipropionate cream in treatment of Microsporum canis infections // J Am Acad Dermatol 1995; 32:1050.
- Hawkins DM, Smidt AC. Superficial fungal infections in children // Pediatr Clin North Am 2014; 61:443.
- Crawford F, Hollis S. Topical treatments for fungal infections of the skin and nails of the foot // Cochrane Database Syst Rev 2007; :CD001434.
- Korting HC, Tietz HJ, Brautigam M, et al. One week terbinafine 1% cream (Lamisil) once daily is effective in the treatment of interdigital tinea pedis: a vehicle controlled study. LAS-INT-06 Study Group // Med Mycol 2001; 39:335.
- Gupta AK, Cooper EA. Update in antifungal therapy of dermatophytosis // Mycopathologia 2008; 166:353.
- Bell-Syer SE, Khan SM, Torgerson DJ. Oral treatments for fungal infections of the skin of the foot // Cochrane Database Syst Rev 2012; 10:CD003584.
- Adams BB. Tinea corporis gladiatorum // J Am Acad Dermatol 2002; 47:286.
- van Zuuren EJ, Fedorowicz Z, El-Gohary M. Evidence-based topical treatments for tinea cruris and tinea corporis: a summary of a Cochrane systematic review // Br J Dermatol 2015; 172:616.6.
- Bourlond A, Lachapelle JM, Aussems J, et al. Double-blind comparison of itraconazole with griseofulvin in the treatment of tinea corporis and tinea cruris // Int J Dermatol 1989; 28:410.
- Cole GW, Stricklin G. A comparison of a new oral antifungal, terbinafine, with griseofulvin as therapy for tinea corporis // Arch Dermatol 1989; 125:1537.
- Panagiotidou D, Kousidou T, Chaidemenos G, et al. A comparison of itraconazole and griseofulvin in the treatment of tinea corporis and tinea cruris: a double-blind study // J Int Med Res 1992; 20:392.
- Faergemann J, Mörk NJ, Haglund A, Odegård T. A multicentre (double-blind) comparative study to assess the safety and efficacy of fluconazole and griseofulvin in the treatment of tinea corporis and tinea cruris // Br J Dermatol 1997; 136:575.
- Elewski BE, Hughey LC, Sobera JO. Fungal diseases. In: Dermatology, 3rd ed, Bolognia JL, Jorizzo JL, Schaffer JV (Eds), Elsevier Limited, Philadelphia; London 2012. Vol 2, p.1251.
- Voravutinon V. Oral treatment of tinea corporis and tinea cruris with terbinafine and griseofulvin: a randomized double blind comparative study // J Med Assoc Thai 1993; 76:388.
- Farag A, Taha M, Halim S. One-week therapy with oral terbinafine in cases of tinea cruris/corporis // Br J Dermatol 1994; 131:684.
- Smith KJ, Neafie RC, Skelton HG 3rd, et al. Majocchi's granuloma // J Cutan Pathol 1991; 18:28.
- Gill M, Sachdeva B, Gill PS, et al. Majocchi's granuloma of the face in an immunocompetent patient // J Dermatol 2007; 34:702.
- Cho HR, Lee MH, Haw CR. Majocchi's granuloma of the scrotum // Mycoses 2007; 50:520.
- Tse KC, Yeung CK, Tang S, et al. Majocchi's granuloma and posttransplant lymphoproliferative disease in a renal transplant recipient // Am J Kidney Dis 2001; 38:E38.
- Kim ST, Baek JW, Kim TK, et al. Majocchi's granuloma in a woman with iatrogenic Cushing's syndrome // J Dermatol 2008; 35:789.
- Akiba H, Motoki Y, Satoh M, et al. Recalcitrant trichophytic granuloma associated with NK-cell deficiency in a SLE patient treated with corticosteroid // Eur J Dermatol 2001; 11:58.
- Ilkit M, Durdu M, Karakaş M. Majocchi's granuloma: a symptom complex caused by fungal pathogens // Med Mycol 2012; 50:449.
- Novick NL, Tapia L, Bottone EJ. Invasive trichophyton rubrum infection in an immunocompromised host. Case report and review of the literature // Am J Med 1987; 82:321.
- Feng WW, Chen HC, Chen HC. Majocchi's granuloma in a 3-year-old boy // Pediatr Infect Dis J 2006; 25:658.
- Gupta AK, Prussick R, Sibbald RG, Knowles SR. Terbinafine in the treatment of Majocchi's granuloma // Int J Dermatol 1995; 34:489.
- McMichael A, Sanchez DG, Kelly P. Folliculitis and the follicular occlusion tetrad. In: Dermatology, 2nd ed, Bolognia JL, Jorizzo JL, Rapini RP (Eds), Elsevier Limited, St. Louis 2008.
- Gupta AK, Groen K, Woestenborghs R, De Doncker P. Itraconazole pulse therapy is effective in the treatment of Majocchi's granuloma: a clinical and pharmacokinetic evaluation and implications for possible effectiveness in tinea capitis // Clin Exp Dermatol 1998; 23:103.
- Burg M, Jaekel D, Kiss E, Kliem V. Majocchi's granuloma after kidney transplantation // Exp Clin Transplant 2006; 4:518.
- Liao YH, Chu SH, Hsiao GH, et al. Majocchi's granuloma caused by Trichophyton tonsurans in a cardiac transplant recipient // Br J Dermatol 1999; 140:1194.
- Bonifaz A, Vázquez-González D. Tinea imbricata in the Americas // Curr Opin Infect Dis 2011; 24:106.
- Cheng N, Rucker Wright D, Cohen BA. Dermatophytid in tinea capitis: rarely reported common phenomenon with clinical implications // Pediatrics 2011; 128:e453.
- Romano C, Rubegni P, Ghilardi A, Fimiani M. A case of bullous tinea pedis with dermatophytid reaction caused by Trichophyton violaceum // Mycoses 2006; 49:249.
- Al Aboud K, Al Hawsawi K, Alfadley A. Tinea incognito on the hand causing a facial dermatophytid reaction // Acta Derm Venereol 2003; 83:59.
- Veien NK, Hattel T, Laurberg G. Plantar Trichophyton rubrum infections may cause dermatophytids on the hands // Acta Derm Venereol 1994; 74:403.