Fungal infections (mycoses) are diseases that are caused by different types of microscopic fungi.
Mycoses of the skin, mucous membranes, and nails are the most common among all human fungal diseases. Systemic mycoses (affecting several body systems) are predominantly found in people with immunodeficiency. Most often these are HIV-infected patients, patients after organ transplantation, cancer patients, etc.
The main causative agents of skin mycoses: trichophyton fungi Trichophyton rubrum, Trichophyton mentagrophytes, var. interdigitale, Epidermophyton floccosum and candida Candida.
Infection with fungi occurs through direct contact with a patient, through shoes, clothing, when using general hygiene products (washcloths, manicure tools), when visiting gyms, baths, saunas, and swimming pools. The main factor of infection is the presence of abrasions and cracks in the skin, which occur with increased sweating, dryness, and poor circulation in the extremities. People with diabetes, immune disorders, blood diseases; Those taking antibiotics, glucocorticosteroids, and cytostatics for a long time are especially susceptible to the development of mycoses.
Most often, microscopic fungi cause damage to the skin of the feet and large skin folds (axillary, groin and others).
Rubrophytia
The cause of rubromycosis (rubrophytosis) is the red fungus trichophyton (Trichophyton rubrum). The fungus got its name for its ability to form a red pigment when growing on Sabouraud's nutrient medium. The widespread distribution of fungi in the environment is the cause of frequent human mycoses.
Rubrophytosis affects the skin of the feet, interdigital spaces on the hands and feet, and nails. The skin of the trunk and large folds is slightly less commonly affected. Even less commonly, the fungus affects the skin of the face and head. A sick person and his personal belongings are a source of infection in public places - swimming pools and baths. The disease is transmitted to all members of his family. Decreased immunity and failure to comply with personal hygiene rules contribute to the development of the disease.
Skin manifestations of rubrophytosis
The disease manifests itself in the form of an erythematosquamous and follicular-nodular form.
Erythematosquamous form
The erythematosquamous form is characterized by the appearance of large spots, on the surface of which papules and vesicles are visible. Dilated capillaries give the lesion a reddish appearance, on the surface of which peeling is noted. The affected area becomes covered with crusts over time. The lesion is surrounded by an intermittent ridge, on the surface of which papules and vesicles are visible.
Follicular nodular form
The follicular nodular form of rubrophytosis is a continuation of the development of the previous form as a result of the lack of proper treatment.
Rice. 6. The photo shows rubrophytia (erythematosquamous form).
Rice. 7. Rubrophytosis of the facial skin (fungus trichophyton rubrum).
Rice. 8. The photo shows rubrophytosis of the skin of the breast (fungus trichophyton rubrum).
Rice. 9. The photo shows rubrophytia (a common form). Fungus trichophyton rubrum.
Prevention and hygiene
If anyone in your home has or has had a fungal skin infection:
- Get rid of combs, brushes, clips or other hair products that may have fungus on them. Do not use other things of the sick person that may have come into contact with his skin.
- Make sure your doctor checks everyone in the house for fungal infections.
- If the fungal infection may have been caused by a pet, contact your veterinarian.
Here are some more general tips to prevent fungal infections:
- Do not share unwashed clothing, sports equipment, or towels with other people.
- Always wear slippers or sandals when in the gym, swimming pool or other public places. This includes public showers.
- Wash with soap and shampoo after sports or exercise.
- Change your socks and underwear at least once a day.
- Keep skin clean and dry. Always dry yourself well after swimming or showering.
Microsporia
The causative agent of the disease is fungi of the genus Microsporum. The source of infection is cats with trichophytosis; less commonly, the disease is transmitted from dogs. Very rarely the disease is transmitted from a sick person. Mushrooms are very stable in the external environment. They live on skin scales and hair for up to 10 years. Children get sick more often, as they are more likely to come into contact with sick stray animals. In 90% of cases, fungi affect vellus hair. Much less often, microsporum affects open areas of the skin.
Skin manifestations of microsporia
The disease is manifested by the presence of round-shaped lesions. Along their periphery there is an inflammatory ridge with blisters and crusts, rising above the surface of the skin. Peeling is observed on the surface of the affected area. More often there is only one focus. Less commonly, multiple lesions no more than 2 cm in diameter appear. The lesions may merge.
Rice. 10. The photo shows microsporia (lesion focus).
Rice. 11. The photo shows microsporia of the facial skin.
Rice. 12. The photo shows microsporia of the skin of the face and neck. Multiple lesions.
Rice. 13. The photo shows microsporia of the scalp.
Rice. 14. The photo shows microsporia of the skin of the hand.
Rice. 15. The photo shows microsporia of the skin of the body (fungus of the genus microsporum).
Rice. 16. The photo shows microsporia of the skin of the face and eyelids.
Rice. 17. The photo shows microsporia of the facial skin. Multiple lesions.
Rice. 18. The photo shows microsporia of the skin of the lower eyelid of the left eye (fungus of the genus microsporum).
Rice. 19. The photo shows microsporia of the facial skin. Characteristic signs.
Transmission routes
The main source of infection is humans
.
The main route of transmission is contact
. Activation of opportunistic flora is also possible when problems with the immune system occur. Fomites, that is, objects contaminated with pathogenic fungi, can be household items, shoes, clothing, and bedding of the sick person, if people who are sensitive to this fungus actively come into contact with them. Outbreaks are possible in organized groups, mainly in children's and army groups. Among public places, swimming pools, water parks and other structures where people can be barefoot inside are considered a common variant of fungal infection, plus a warm and humid microclimate is formed there, which contributes to the long existence of the pathogen outside the host.
In rare cases, for example, with microsporia, the source of infection can be a street or domestic animal, most often a cat. In common parlance, this disease is called “lichen.” “Ringworm” or, more precisely, “ringworm” in a child is microsporia. It is also possible to become infected with trichophytosis through contact in rural areas with hay or other substrates on which the secretions of sick rodents remain.
Trichophytosis
The culprit of the disease is fungi of the genus Trichophyton, which parasitize the skin of humans, cattle and rodents. The disease is most often recorded in the fall, when field work begins. Then the source of the disease becomes hay and straw. In this case, exposed areas of the body are affected. Fungi that parasitize humans can become a source of trichophytosis. The disease is highly contagious (infectious). The person himself and his things are the source of infection. With this form of trichophytosis, open areas of the body are also affected, but with a prolonged course, the skin of the buttocks and knees can be affected.
Skin manifestations of trichophytosis
The affected areas of the skin are round in shape, bright red, similar to those with microsporia, but much larger, with elements of peeling and small nodules. There is an inflammatory ridge along the edges. Fungal infection occurs in the form of 3 forms, which, as the disease develops, replace each other: superficial form, infiltrative and suppurative.
Rice. 20. The photo shows trichophytosis (fungus). The lesion is large.
Rice. 21. The photo shows trichophytosis of the facial skin.
Rice. 22. The photo shows trichophytosis (chronic form).
Rice. 23. The photo shows trichophytosis of the beard and mustache area (fungus of the genus trichophyton).
Rice. 24. The photo shows trichophytosis of the smooth skin of the forearm.
Rice. 25. The photo shows trichophytosis of the skin of the trunk.
Rice. 26. The photo shows trichophytosis of the skin of the face (left) and hand (right).
Diagnostics
The diagnosis is confirmed by the detection of segmented hyphae in skin scrapings from the affected area with potassium hydroxide (KOH). When bubbles form, the top of the bubble can serve as an adequate sample. Alternative diagnostic procedures are dermatophyte culture test medium and culture method.
Patients who have significant erosion, ulceration, or malodor in the affected area should undergo Gram staining and culture to evaluate for secondary bacterial infection.
Differential diagnosis depends on clinical subtype:
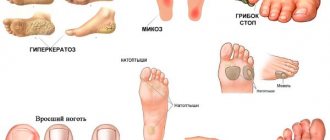
Interdigital dermatitis of the foot
- Erythrasma
- Interdigital candidiasis
- Hyperkeratotic (moccasin) dermatitis of the foot
- Atopic dermatitis
- Chronic contact dermatitis
- Chronic palmoplantar (dyshidrotic) eczema
- Palmoplantar psoriasis
- Pitted keratolysis
- Juvenile plantar dermatosis
- Exfoliating keratolysis
- Keratoderm
Inflammatory dermatosis of the foot
- Acute palmoplantar (dyshidrotic) eczema
- Acute contact dermatitis
- Palmoplantar pustulosis
- Scabies
A positive KOH test demonstrating segmented hyphae distinguishes Tinea pedis from nonfungal diseases. With interdigital candidiasis, a test with the drug KOH will show budding yeast, pseudohyphae and hyphal septa.
Pityriasis versicolor or versicolor versicolor
Tinea versicolor is a fairly common disease. The disease is more common in young and middle-aged people. Fungi parasitize in the uppermost layers of the skin and in the areas of hair follicles. Under certain conditions they can cause disease. It is believed that the cause of the disease is a change in the chemical composition of sweat due to excessive sweating. Diseases of the stomach and intestines, endocrine system, neurovegetative pathology and immunodeficiency are the trigger for the development of pityriasis versicolor. Fungi infect the skin of the body. Lesions are often found on the skin of the chest and abdomen. The skin of the head, extremities and groin areas is much less frequently affected.
Skin manifestations of pityriasis versicolor
With pityriasis versicolor, pink spots appear, the surface of which slightly peels off. The spots tend to merge. Their color changes over time to light or dark brown.
Rice. 27. The photo shows pityriasis versicolor of the facial skin.
Rice. 28. The photo shows facial skin with pityriasis versicolor.
Rice. 29. The photo shows pityriasis versicolor of the skin of the chest.
Rice. 30. The photo shows pityriasis versicolor of the skin of the chest and torso.
Rice. 31. Pityriasis versicolor of the skin of the back.
Rice. 32. Pityriasis versicolor (fungus) of the skin of the hands.
Seborrheic dermatitis
Seborrheic dermatitis is caused by the lipophilic fungi Malassezia furfur (Pityrosporum). Fungi parasitize the skin of many people. The scalp is affected by the fungus Pityrosporum ovale (P. ovale). Fungi Pityrosporum orbiculare (P. orbiculare) infect the skin of the body. Pathogens concentrate in areas of greatest accumulation of sebum, which is produced by the sebaceous glands. The causative agents of seborrheic dermatitis use sebum in the process of their life. The rapid growth of fungi is provoked by neurogenic, hormonal and immune factors.
With seborrheic dermatitis, the lesions are widely localized, but most often the disease affects the scalp. Lesions may appear at the border of hair growth, eyebrows and eyelashes. The skin in the mustache and beard area is affected. Often lesions are recorded in the nasolabial folds, on the skin of the ear canals and behind the ear areas. Less commonly, the skin of the sternum and body folds is affected.
The pathogen can infect the skin around the anus and genitals. In the case of negative developments, the disease becomes widespread.
Skin manifestations of seborrheic dermatitis
Skin manifestations of seborrheic dermatitis are represented by areas of inflammation with elements of peeling. If the process is localized in open areas of the skin, then the inflammatory component becomes less noticeable, and peeling intensifies. Sometimes the lesion becomes covered with hemorrhagic crusts. The disease is sometimes accompanied by itching, which can be quite intense. When a secondary infection occurs, suppuration is noted.
Rice. 33. Seborrhea in the photo. Damage to the scalp.
Rice. 34. Seborrhea in the photo. Damage to the eyelash area.
Rice. 35. The photo shows seborrhea. Damage to the ear area.
Rice. 36. Seborrhea in the photo. Damage to the ear canal area.
Rice. 37. The photo shows seborrheic dermatitis (facial skin lesions).
Rice. 38. The photo shows seborrheic dermatitis (damage to the mustache area).
Candidiasis
The culprit of candidiasis is yeast-like fungi of the genus Candida, which are widespread in the environment. They constantly, starting from the moment of birth, parasitize the skin and mucous membranes. The disease is promoted by a sharp decrease in immunity and the prescription of long courses of broad-spectrum antibiotics. A large number of mushrooms can get on human skin at once. In some professions, the pathogen reaches a person constantly in small portions.
With candidiasis, changes appear primarily on the skin of large and small folds of the body. As the disease develops, the lesions spread to the skin of the body. Somewhat less frequently, lesions are observed on the skin of the palms and soles. The disease often affects infants. Patients with diabetes mellitus and severe somatic pathology are at risk for candidiasis. The disease lasts a long time. Recurs often.
Skin manifestations of candidiasis
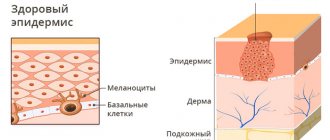
Initially, the affected areas acquire a reddish color, against which multiple small bubbles are visible. The process is spreading very quickly. The reddish color changes to deep red. In place of the vesicles, areas of erosion appear. The boundaries of the lesion are clearly defined. Along its periphery, areas of the exfoliated stratum corneum of the epidermis are visible.
Rice. 39. The photo shows candidiasis (facial skin lesions).
Rice. 40. The photo shows candidiasis (skin lesions on the lower part of the face).
Rice. 41. The photo shows candidiasis (facial skin lesions in a child).
Rice. 42. The photo shows candidiasis of the skin of the body.
Rice. 43. The photo shows candidiasis (common form).
Treatment of skin fungus
Mycoses are difficult to treat due to impaired cellular immunity. When treating them, old proven remedies and modern antifungal drugs are used, which are divided into drugs that stop the growth of fungi and drugs that kill them. Some of these drugs are obtained synthetically, others are natural. There are narrow- and broad-spectrum antifungal drugs. In addition, different forms of the disease have their own nuances of treatment, so only a doctor can choose the right treatment.
The basis of treatment for skin fungus is:
- The use of general and local antifungal drugs.
- Treatment of somatic pathology.
- Antifungal treatment of personal belongings and household items to prevent re-infection and adherence to personal hygiene rules.
Local treatment of skin fungus
Fungal infections (mycoses) are a very common disease. A doctor’s arsenal includes many medications, such as old, well-proven ones, as well as new drugs that are available in the form of ointments, creams, lotions, sprays, drops and powder. They are easily applied to the skin.
- When swelling, skin damage, oozing and secondary infection occur, antifungal drugs with corticosteroids and a broad-spectrum antibiotic (Triderm cream, Mikozolon, Lotriderm, etc.) are used. Triderm cream is available in the form of ointment and cream, which allows it to be used for different types of fungal damage and at different stages of the pathological process. The simultaneous use of Lamisil spray gives a good effect.
- When acute inflammatory phenomena subside, drugs are used that kill fungi or stop their growth and reproduction. The group of azoles for topical use is represented by Clotrimazole, Miconazole, Bifonazole, Econazole, Isocanazole, Ketoconazole, Metronidazole, Fluconazole, etc. The group of allylamine amines is represented by Naftifine and Terbinafine (Lamisil). A group of medications of various chemical groups is represented by preparations of undecinic acid (Undecine and Zincundan), quinosol, urea, acids (lactic, acetic, benzoic), Octicyl, Decamine, Anmarin, aniline dyes, etc.
Some information about Lamisil
- Lamisil is highly active against all types of fungi, including yeast and mold.
- Lamisil exhibits high activity in the treatment of complications of the disease and allergic rashes.
- The drug is available in the form of a spray, gel (Lamisil Dermgel), cream and film-forming solution (Lamisil Uno), which ensures maximum comfort of its use.
- The drug is used to prevent disease and treat shoes.
- Lamisil restores skin pH and skin hydration levels.
- Promotes epithelization of skin lesions with cracks.
- When using Lamisil Uno, the film covering the skin of the feet lasts up to 72 hours, ensuring that the drug reaches the stratum corneum of the skin for a long time.
- The clinical effectiveness of the drug reaches 72%.
Treatment of skin fungus with systemic antifungal drugs
Treatment of fungal infections with tablets and injections (systemic drugs) is used for moderate and severe disease. Taking them increases the chances of cure, but requires constant medical supervision due to a number of side effects.
For the treatment of fungal diseases, 2 groups of antimycotic tablet drugs are used:
- Group 1 of drugs (azoles) is represented by itraconazole (orungal), fluconazole, ketocornazole;
- Group 2 drugs (allylaminamines) are represented by terbinafine and naftifine. Itraconazole and terbinafine quickly penetrate the stratum corneum of the skin and remain there for a long time.
Selection of doses of antifungal drugs and determination of the duration of treatment is carried out only by a doctor
If the disease is combined with skin lesions in other parts of the body, the doctor will decide to prescribe more powerful antifungal drugs.
Pathogenetic therapy
Pathogenetic therapy drugs are prescribed for any pathology. With their help, the effectiveness of treatment increases and the likelihood of adverse reactions decreases.
In case of fungal infection it is necessary:
- correct immunological disorders,
- reduce allergic manifestations,
- make up for the lack of sulfur, which is found in eggs, cottage cheese, herbs, etc.,
- take vitamins of group A.
Timely initiation and correct selection of treatment for fungal infection will allow you to achieve a healthy appearance in the shortest possible time, eliminate the feeling of discomfort and improve your general condition.
Reasons for treatment failure
The main reason for the ineffectiveness of treatment for fungal diseases is the patient’s violation of the treatment regimen.
- More than a third of patients consider their disease not serious and refuse treatment.
- About 70% of patients do not believe that the prescribed treatment will bring a positive result.
- Half of the patients are not satisfied with the previous treatment.
- Up to 70% of patients stop treatment when a positive result is achieved and no longer come to see a doctor to monitor for cure.
conclusions
Superficial fungal infections are most often caused by dermatophytes from the genera Trichophyton, Epidermophyton and Microsporum. These organisms metabolize keratin and cause a number of pathological clinical manifestations, including tinea pedis, dermatophytal dermatitis, dermatophytosis, etc. Based on clinical findings, the diagnosis of cutaneous dermatophyte infection can be strongly suspected. To confirm the diagnosis, potassium hydroxide should be used. Most dermatophyte infections can be managed with topical treatment. Examples of effective topical antifungal agents include azoles, allylamines, ciclopirox, butenafine, and tolnaftate. Oral antifungal therapy is used for widespread infections or infections that are resistant to topical therapy. Nystatin is not effective against dermatophyte infections.
List of literature / References
- Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide // Mycoses. 2008 Sep;51 Suppl 4:2-15. doi: 10.1111/j.1439-0507.2008.01606.x. Erratum in: Mycoses. 2009 Jan;52(1):95. PMID: 18783559.
- Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide // Mycoses 2008; 51 Suppl 4:2.
- Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections // Mycopathologia 2008; 166:335.
- Ameen M. Epidemiology of superficial fungal infections // Clin Dermatol 2010; 28:197.
- El-Gohary M, van Zuuren EJ, Fedorowicz Z, et al. Topical antifungal treatments for tinea cruris and tinea corporis // Cochrane Database Syst Rev 2014; :CD009992.
- Alston SJ, Cohen BA, Braun M. Persistent and recurrent tinea corporis in children treated with combination antifungal/ corticosteroid agents // Pediatrics 2003; 111:201.
- Greenberg HL, Shwayder TA, Bieszk N, Fivenson DP. Clotrimazole/betamethasone diproprionate: a review of costs and complications in the treatment of common cutaneous fungal infections // Pediatr Dermatol 2002; 19:78.
- Rosen T, Elewski BE. Failure of clotrimazole-betamethasone dipropionate cream in treatment of Microsporum canis infections // J Am Acad Dermatol 1995; 32:1050.
- Hawkins DM, Smidt AC. Superficial fungal infections in children // Pediatr Clin North Am 2014; 61:443.
- Crawford F, Hollis S. Topical treatments for fungal infections of the skin and nails of the foot // Cochrane Database Syst Rev 2007; :CD001434.
- Korting HC, Tietz HJ, Brautigam M, et al. One week terbinafine 1% cream (Lamisil) once daily is effective in the treatment of interdigital tinea pedis: a vehicle controlled study. LAS-INT-06 Study Group // Med Mycol 2001; 39:335.
- Gupta AK, Cooper EA. Update in antifungal therapy of dermatophytosis // Mycopathologia 2008; 166:353.
- Bell-Syer SE, Khan SM, Torgerson DJ. Oral treatments for fungal infections of the skin of the foot // Cochrane Database Syst Rev 2012; 10:CD003584.
- Adams BB. Tinea corporis gladiatorum // J Am Acad Dermatol 2002; 47:286.
- van Zuuren EJ, Fedorowicz Z, El-Gohary M. Evidence-based topical treatments for tinea cruris and tinea corporis: a summary of a Cochrane systematic review // Br J Dermatol 2015; 172:616.6.
- Bourlond A, Lachapelle JM, Aussems J, et al. Double-blind comparison of itraconazole with griseofulvin in the treatment of tinea corporis and tinea cruris // Int J Dermatol 1989; 28:410.
- Cole GW, Stricklin G. A comparison of a new oral antifungal, terbinafine, with griseofulvin as therapy for tinea corporis // Arch Dermatol 1989; 125:1537.
- Panagiotidou D, Kousidou T, Chaidemenos G, et al. A comparison of itraconazole and griseofulvin in the treatment of tinea corporis and tinea cruris: a double-blind study // J Int Med Res 1992; 20:392.
- Faergemann J, Mörk NJ, Haglund A, Odegård T. A multicentre (double-blind) comparative study to assess the safety and efficacy of fluconazole and griseofulvin in the treatment of tinea corporis and tinea cruris // Br J Dermatol 1997; 136:575.
- Elewski BE, Hughey LC, Sobera JO. Fungal diseases. In: Dermatology, 3rd ed, Bolognia JL, Jorizzo JL, Schaffer JV (Eds), Elsevier Limited, Philadelphia; London 2012. Vol 2, p.1251.
- Voravutinon V. Oral treatment of tinea corporis and tinea cruris with terbinafine and griseofulvin: a randomized double blind comparative study // J Med Assoc Thai 1993; 76:388.
- Farag A, Taha M, Halim S. One-week therapy with oral terbinafine in cases of tinea cruris/corporis // Br J Dermatol 1994; 131:684.
- Smith KJ, Neafie RC, Skelton HG 3rd, et al. Majocchi's granuloma // J Cutan Pathol 1991; 18:28.
- Gill M, Sachdeva B, Gill PS, et al. Majocchi's granuloma of the face in an immunocompetent patient // J Dermatol 2007; 34:702.
- Cho HR, Lee MH, Haw CR. Majocchi's granuloma of the scrotum // Mycoses 2007; 50:520.
- Tse KC, Yeung CK, Tang S, et al. Majocchi's granuloma and posttransplant lymphoproliferative disease in a renal transplant recipient // Am J Kidney Dis 2001; 38:E38.
- Kim ST, Baek JW, Kim TK, et al. Majocchi's granuloma in a woman with iatrogenic Cushing's syndrome // J Dermatol 2008; 35:789.
- Akiba H, Motoki Y, Satoh M, et al. Recalcitrant trichophytic granuloma associated with NK-cell deficiency in a SLE patient treated with corticosteroid // Eur J Dermatol 2001; 11:58.
- Ilkit M, Durdu M, Karakaş M. Majocchi's granuloma: a symptom complex caused by fungal pathogens // Med Mycol 2012; 50:449.
- Novick NL, Tapia L, Bottone EJ. Invasive trichophyton rubrum infection in an immunocompromised host. Case report and review of the literature // Am J Med 1987; 82:321.
- Feng WW, Chen HC, Chen HC. Majocchi's granuloma in a 3-year-old boy // Pediatr Infect Dis J 2006; 25:658.
- Gupta AK, Prussick R, Sibbald RG, Knowles SR. Terbinafine in the treatment of Majocchi's granuloma // Int J Dermatol 1995; 34:489.
- McMichael A, Sanchez DG, Kelly P. Folliculitis and the follicular occlusion tetrad. In: Dermatology, 2nd ed, Bolognia JL, Jorizzo JL, Rapini RP (Eds), Elsevier Limited, St. Louis 2008.
- Gupta AK, Groen K, Woestenborghs R, De Doncker P. Itraconazole pulse therapy is effective in the treatment of Majocchi's granuloma: a clinical and pharmacokinetic evaluation and implications for possible effectiveness in tinea capitis // Clin Exp Dermatol 1998; 23:103.
- Burg M, Jaekel D, Kiss E, Kliem V. Majocchi's granuloma after kidney transplantation // Exp Clin Transplant 2006; 4:518.
- Liao YH, Chu SH, Hsiao GH, et al. Majocchi's granuloma caused by Trichophyton tonsurans in a cardiac transplant recipient // Br J Dermatol 1999; 140:1194.
- Bonifaz A, Vázquez-González D. Tinea imbricata in the Americas // Curr Opin Infect Dis 2011; 24:106.
- Cheng N, Rucker Wright D, Cohen BA. Dermatophytid in tinea capitis: rarely reported common phenomenon with clinical implications // Pediatrics 2011; 128:e453.
- Romano C, Rubegni P, Ghilardi A, Fimiani M. A case of bullous tinea pedis with dermatophytid reaction caused by Trichophyton violaceum // Mycoses 2006; 49:249.
- Al Aboud K, Al Hawsawi K, Alfadley A. Tinea incognito on the hand causing a facial dermatophytid reaction // Acta Derm Venereol 2003; 83:59.
- Veien NK, Hattel T, Laurberg G. Plantar Trichophyton rubrum infections may cause dermatophytids on the hands // Acta Derm Venereol 1994; 74:403.