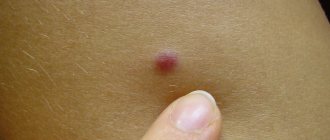
It often happens that we injure moles. Rip off completely or slightly tear off from the skin. It happens that the bleeding is quite strong, but it is still possible to stop it. Here the mole is covered with a band-aid and everything seems to be fine. Here we remember that in childhood our mother told us: “Don’t pick at a mole - you can die from it.” With an unpleasant feeling somewhere in the upper abdomen, we begin to search on the Internet for the eternal answer to the question “What to do?” After half an hour or an hour we understand that in a couple of days death from melanoma will occur and it’s time to look for a place in the cemetery...
Later in this article I will try to interrupt the endless stream of hysteria that has been copied from site to site for many years
Sign up for the webinar “Carcinogens in cosmetics: truth, lies and... marketing”
Is mole injury really dangerous?
In RuNet, the danger of traumatizing moles is given excessive, in my opinion, importance. Is there any justification for this point of view? Absolutely, but I think it's quite shaky.
Indeed, there are several studies on this issue, mostly conducted in the 60s–80s of the last century. They show that 30–50% of patients in whom melanoma developed against the background of a nevus noted single or repeated trauma to the mole.
There are several arguments against these studies:
- Just because melanoma develops after trauma to a nevus does not necessarily mean that the two are related. Melanoma could develop both before trauma and much later for other reasons .
- A 2010 meta-analysis (summarizing data from 9 studies) showed that performing an incisional biopsy does not affect the prognosis of melanoma. In other words, if a piece is cut off from melanoma (for diagnostic purposes), this will not negatively affect the patient’s chances of living 5 years or more.
- The conclusions of the authors of several studies (55, 115, 147 and 498 patients) agree on one thing - incomplete removal of nevi, except for dysplastic ones with severe dysplasia, does not lead to the development of melanoma.
Here the corrosive reader will say: “Aha! Still, incomplete removal (you can read “trauma”) causes the development of melanoma!” No. A dysplastic nevus with severe dysplasia itself has a high chance of becoming melanoma in the future. The connection between incomplete removal and the development of melanoma from such nevi has not been proven .
- My experience. Almost every day people write to me who have injured a mole and are now preparing to “die” because they have read too much on the Internet. Almost any person who has a mole protruding above the skin has injured it in one way or another at least once in their life. If trauma to a mole were really a risk factor, in our country with a population of 146,000,000, the diagnosis of melanoma would be made much more often than 8,000 times a year.
Main causes of peeling
Itching, inflammation, and peeling of the surface of the nevus cannot be ignored. In some cases, they become the first symptoms of melanoma - a very dangerous disease with a high probability of death. Concomitant manifestations of the disease may include:
- rapid growth and deformation,
- fuzzy contours and asymmetry,
- color change - with malignancy, tissues may lighten or darken, inclusions of a different shade may appear in them,
- bleeding,
- appearance of cracks.
Peeling moles are also sometimes provoked by damage to the skin by clothing or accessories, and some dermatological diseases.
What will happen to the mole next?
After trauma, as in any other place, the mole will hurt a little and turn slightly red - this is normal. Gradually, after 2-3 weeks, these phenomena should go away on their own. The only situation in which medical intervention may be required is the suppuration of a mole after a severe injury. This means that if after a few days a viscous white (not yellow) liquid begins to come out from the site of injury, you need to be examined by a surgeon. After 1-2 days, a crust will appear at the site of the injury, which will fall off on its own after 1-2 weeks.
Why do nevi disappear?
The disappearance of a long-existing nevus may be a consequence of natural aging of the body, changes in melanin concentration due to dermatological diseases, exposure to ultraviolet radiation, or trauma. In most cases, such depigmentation is safe for humans, but still requires consultation with a specialist. In rare cases, fading of a pigment spot may indicate malignancy of its cells. Do not delay visiting your doctor if:
- the mole has peeled off and almost disappeared,
- its surface has lightened or darkened, become uneven in color,
- the skin around it is lightened, red, or inflamed.
Only an experienced dermatologist can determine the exact cause of such changes.
How to properly monitor a mole after an injury?
To objectively track changes in a mole, after the inflammation has subsided, you can take a photograph of it against the background of a ruler and compare the original image with subsequent ones. In order for the photo to be of high quality and comparison possible, the following rules must be observed:
- The photo must be taken with a camera, not a phone.
- The photo should not be a “selfie”. In such photographs, the mole is usually out of focus.
- A light source or camera flash should be directed at the mole.
When the sun is the enemy
Probably everyone already knows that a chocolate tan has little to do with health. Ultraviolet radiation causes DNA damage and is the main cause of malignant skin tumors. The more time a person spends exposing his body to the rays, the higher the likelihood of unpleasant consequences. The activity of the sun is also important. It is no coincidence that dermatologists strongly advise not to be on the beach between 11 and 16 hours of the day, when it is most aggressive.
By the way, many scientists associate the risk of developing melanoma with the fact that in childhood and adolescence a person often received sunburn. They cause changes in melanocytes, the pigment cells of the skin, which over time lead to malignant conditions. This also explains the fact that in almost 50% of cases, melanoma develops on the legs - they are always open in children in the summer and are most exposed to solar radiation.
Lately, there has been more and more talk about the dangers of “artificial sun” – solariums. According to some reports, one session here (which is usually 5-10 minutes) is equal to a whole day on the beach! Some European countries (Germany, France and Austria) and the state of California (USA) have even banned the use of solariums for children under 18 years of age.
Of course, the sun is a source of vitamin D and a remedy for depression, but in large quantities it is the real enemy. Otherwise, the World Health Organization would not recognize ultraviolet radiation as a carcinogen on a par with arsenic, smoking and asbestos.
Briefly about the main thing:
In my opinion, there is currently no convincing evidence that trauma to a mole can lead to the development of melanoma. Besides me, oncology associations such as NCCN and ESMO also think the same. However, I don’t know if everything was fine with your mole BEFORE the injury. That is why, after the inflammation has subsided, I recommend contacting an oncologist, especially if this specialist has not looked at all of your moles before. If pain, redness, and swelling do not go away within a month, you need to see an oncologist as quickly as possible.
If you still have questions, the following will help you:
- In-person appointment with an oncologist
(St. Petersburg) - Mole removal
with histology (St. Petersburg) - My Online consultation (from anywhere in the world)
What to do if the nevus begins to grow after removal?
Why did it happen?
Maybe I should have chosen a different removal method? Maybe you need to change doctor? First of all, contact the doctor who performed the mole removal procedure. It is he who has the most reliable information about the nevus itself and his actions with it. What to do next? This is already a matter of trust. If trust in the doctor is retained, correct him; if not, you need to choose another specialist. But any intervention, especially a surgical one, should be approached soberly, balancedly and without unnecessary emotions.
With laser or radio wave removal, the risks of relapse arise not so much because of the lack of nevus cells horizontally, but because of the lack of vertical removal, that is, deep into the skin.
In different types of moles and in different areas of the skin, nevus cells can lie deep enough in the dermis and at different levels, which can cause local relapse.
If a mole recurs, you can resort to excision of the scar with recurrent growth, but in my opinion this is an overly aggressive approach. It should only be used if histological examination was not performed at the time of removal, and the recurrence looks suspicious regarding the growth of melanoma.
Is it dangerous for moles to appear at the site of removal?
No, it's not dangerous!
This is not my subjective opinion, this is data from many studies conducted. There is no evidence of an increased risk of melanoma at the site of a removed nevus. Another thing is that the removal of the mole itself was carried out as a preventive measure against the formation of melanoma, which means that if a local relapse occurs, this risk remains. Since the desired result has not been achieved, it is necessary to carefully remove the nevus.
Typically, additional removal is carried out using the same method that was used during the patient’s initial treatment. That is, as a rule, resurfacing of a recurrent nevus is carried out using a laser or radio wave method.
Is it necessary to perform a histological examination of recurrent nevus?
This can be done, but is not always necessary.
If a removed nevus has been examined histologically, then a recurrent one should be examined only if there is a suspicion of malignancy. If histology of the removed nevus was not carried out, and the primary removal was not carried out in our clinic, we will definitely send the material for histological examination. In conclusion, I want to say that, of course, the occurrence of a recurrence of a mole is an unpleasant situation for both the patient and the doctor. But it is very simple to correct this situation without any harm to health and appearance - contact a specialist to remove the recurrence of the nevus.
We professionally care about the beauty and health of your skin. If you are concerned about the appearance of moles after removal, make an appointment with an oncodermatologist
by phone, +7 (812) 318-59-90, and we will help you solve this problem.
Where to run?
If you notice an unusual mole on your body, be sure to go to a dermato-oncologist. If this doctor is not available, you can consult a dermatologist, surgeon or oncologist. An experienced specialist can visually determine the nature of the nevus. A special device called a dermatoscope helps him with this. Essentially, this is a powerful magnifying glass; by examining a mole through it, the doctor can notice the smallest details that are simply impossible to see with the naked eye. If there is doubt about the diagnosis, the doctor will conduct a histological examination to determine the characteristic signs of benign, premalignant and malignant neoplasms.
By the way, if you want to remove a mole for aesthetic reasons, then the decision should also be made by a dermato-oncologist after dermatoscopy, which allows you to choose the optimal method, determine the boundaries and depth of removal.
Even if degeneration into melanoma has not occurred, for medical reasons those moles that are subject to constant friction, pressure, and injury are removed. And also those that are in the groin area and under the arms, under the chest, on the belt, and in men - on the face at the shaving site.
If a mole that has degenerated into melanoma is removed at an early stage, the probability of complete recovery reaches 95%; if time is lost, it is only 20%.
Diagnostics
There are a number of signs of malignant degeneration of a mole:
- in the area of the mole there are signs of a violation of the skin pattern, peeling;
- the color of the mole changes from black to pale pink;
- uneven coloring of the mole;
- the formation of an inflammatory corolla around the mole;
- changing boundaries;
- increase in size, thickening of the mole;
- vertical or horizontal growth.
The appearance at the base of a mole of nodes with areas of decay, cracks, ulcers, bleeding, the presence of itching, burning, tingling should also be alarming.
The first signs of melanoma are an increase in the size of the mole. Discoloration, bleeding, ulceration and pain appear much later.
Diagnosis also consists of a thorough examination of the skin, including the armpits, scalp, interdigital folds, genitals, perianal area and oral mucosa, as well as palpation by the doctor of the lymph nodes and liver.
For unambiguous confirmation, an ultrasound examination (to determine the thickness and depth of invasion), ultrasound of the lymph nodes and abdominal organs, chest x-ray, biopsy and computed tomography (if metastases are suspected) are performed. A biopsy is indicated in some cases - when the thickness of the tumor is from 1 to 4 mm and if the entire range of diagnostic measures did not make it possible to verify the diagnosis.
Dermatological diseases and peeling moles
A very large group of reasons for peeling skin over moles.
The most common:
- allergic processes;
- genetic – ichthyosis;
- psoriasis;
- pityriasis versicolor;
- seborrhea;
- contact dermatitis.
The list can be continued for a very long time.
It is important to remember one thing: if dermatological pathology manifests itself as peeling and affects areas of the skin with moles, then this is a reason to consult a dermatologist and undergo a course of treatment.
Problems usually arise among those who do not want to be examined by a specialist and try to cure themselves.
Allergies
are a very common cause in modern civilization.
Character traits:
- the skin turns red;
- small urticaria-type rashes or large, dense papules appear;
- the involved areas itch, itch unbearably;
- As the allergy resolves, fairly large areas of peeling may remain at the site of the rash, including moles.
The beginning of the process after contact with an allergen (which one is an individual matter) indicates in favor of an allergic component.
Ichthyosis
This genetic pathology is not that uncommon.
There are cases in dermatological practice when large areas of the dermis of children peel off along with the moles located on them.
External signs depend on the severity of the disease: from dry skin to deep cracks.
Psoriasis
Another common reason for peeling.
Moreover, such a process is a characteristic sign of this disease.
The scales peel off almost like flakes.
But since only the epithelium of the stratum corneum (which is continuously renewed) disappears, the moles located deeper (nevi) do not disappear anywhere.
True, they can hide under plaques and become invisible.
Pityriasis versicolor
This is a fungal disease, the sign of which is a limited area of peeling, as if consisting of several spots.
The shape is round, the edges are uneven, scalloped.
The formation is painless, but in some people it itches.
Naturally, the focus of pityriasis versicolor can occur above the mole.
If it is also small in size, then sometimes it seems as if a mole is peeling off.
Although this is not true.
Seborrhea
A common phenomenon is when sebum synthesis is too active.
Quite often such problems arise on the head.
Foci of different sizes are formed, covered with loose yellowish scales, which literally peel off in layers.
Seborrhea occurs in children and adults.
The affected surface shines and peels, which is why it becomes a frequent reason for contacting dermatologists.
Contact dermatitis
Most often, these will be local allergic reactions in response to contact with allergenic fabric, detergent residue, grass, and so on.
They differ in that itching, redness and peeling occur to a limited extent.
Only on the surface of the body that came into contact with the allergen.
Beware, provocateurs!
What provokes the process of degeneration of moles? First of all, insolation (stay in the sun). It is useless to protect moles from the ubiquitous sun's rays with a towel, a Panama hat, and even more so by covering them with a band-aid - the greenhouse effect deals a double blow. Solarium is no less dangerous; it is absolutely contraindicated for those who have many moles on their body.
Any injury to a mole can give impetus to the development of a tumor. Therefore, if you hit it with your fingernail or inadvertently damaged it with some sharp object, be sure to see a doctor.
By the way, those who have many moles on their body should wash only with a soft sponge, not a hard washcloth, and especially not rub their back with a brush. Moles that protrude above the surface of the skin are best washed carefully by hand.
How to reduce the risk of damage and malignancy of moles?
Every damage to a red or brown mole increases the risk of it becoming cancerous. That is why experts recommend removing benign tumors that constantly rub against clothes and interfere with shaving. You can only trust the removal of vascular tumors to a qualified dermatologist. The doctor will choose a method that will avoid excessive bleeding when blood vessels are damaged, and will develop a program to prevent complications. Modern techniques allow you to remove any mole without a trace. After the wound heals, no scars form.
Are you looking for where to remove a mole on Bratislavskaya? Contact our clinic. To carry out such procedures, our doctors use the Surgitron radio wave knife. The dermatologist will tell you more about the benefits of its use at a preliminary consultation.
All articles
5% discount Print coupon from our website
Ask your question on the website Get professional advice!
Possible complications and precautions
Moles vary in appearance and can transform into melanomas. After detachment, nothing bad will happen. To be sure of determining the malignancy of a tumor, you should consult your doctor. The main complication is the spread of a cancerous tumor, in advanced situations with a fatal outcome.
In some situations, the malignancy of a detached growth is determined by the following factors:
- by gender – women are less likely to experience degeneration of education;
- direction of nevus growth: hanging growths are often examined more closely.
To prevent the development of cancer, you should carefully monitor all formations: flat birthmarks or raised moles located throughout the body. If the formation begins to bleed or peel, you need to go to the clinic, do not wait until the problem goes away.
What to do if you have a problem like this
If the formation has disappeared, first aid should be provided. It consists of stopping bleeding and treating the wound with peroxide. Apply a sterile bandage or adhesive plaster to the wound. Then go to the hospital. If possible, place the fallen part in saline solution for examination. If a piece is lost, you can take the biomaterial from the wound.
During the diagnostic process, the malignant or benign nature of the formation is revealed. A dermatologist examines the formation through a dermatoscope, determines its origin, and prescribes treatment. After examination, the doctor prescribes a treatment method - surgery or laser therapy. You will need to consult an oncologist to determine the nature of the tumor. A plastic surgeon will remove traces of growth if the tumor is in a noticeable place.
At an appointment with an oncologist, tests are prescribed, the medical record is examined, the presence of complaints, and a hereditary tendency to oncology. Visual presence of symptoms – darkening, redness, peeling of the skin. A biopsy of the lesion is performed and a histological analysis of the biomaterial is performed to final confirm the diagnosis. To identify metastases affecting lymphatic vessels and distant organs, X-rays, MRI and CT are prescribed.
Timely detection and treatment of cancer in the initial stages will lead to success. The operation is performed under local anesthesia and is irradiated with high-frequency X-ray radiation. The therapy makes it possible to stop the atypical division of degenerated cells and to carry out a successful intervention to remove the cancerous tumor and the adjacent healthy epidermis.
The tumor is eliminated using a laser or liquid nitrogen. The procedures are painless, leaving a slight scar after burning or freezing. If metastases spread, chemotherapy is prescribed.