Acne in children is one of the most common skin diseases, especially in adolescence. We are talking about a violation of the hair follicles and sebaceous glands, which become clogged, leading to the formation of pimples and cysts.
Acne or Acne vulgaris by its medical name is defined as inflammation of the sebaceous glands. Most often this occurs during puberty, as a result of hormonal activity. In addition to pain and discomfort, acne in boys and girls is fraught with social isolation, the constant need to hide damage, low self-esteem, and in some cases even the development of anxiety and depression. That's why it's so important to understand what acne is and what the most effective ways to treat it are.
Acne classification
When classified by age group, there are mainly two types of acne:
- In newborns and young children. The belief that acne only affects teenagers and adults is wrong. Infants, children of preschool and early school age, although not often, also suffer from acne. Newborns face this problem because their mothers transfer hormones to them shortly before birth. Acne also occurs when the stress of childbirth causes the baby's body to release these hormones.
- Teenagers and adults. Acne affects 80% of people aged 11 to 30 years. Usually occur during pubertal changes in hormonal levels. Increased production of sex hormones during puberty makes the sebaceous glands more active.
Table - Classification of childhood acne by age
| Form | Child's age |
| Neonatal | from birth to 6 weeks |
| Infantile (early childhood) | from 6 weeks to 12 months |
| Middle childhood | from one to 7 years |
| Pre-adolescent | from 7 to 12 years (for girls before menarche) |
Neonatal acne develops during a period of hormonal changes. In all forms of acne, additional provoking exogenous factors play a significant role.
Hormonal ointments for diathesis
A special group of local drugs used for diathesis are hormonal ointments. They are used if non-hormonal drugs do not help. Hormonal drugs have a more serious composition, including hormonal components - glucocorticoids. These are steroid hormones synthesized by the adrenal cortex. The most common among them are:
- Natural glucocorticoids: cortisol, hydrocortisone. Their effect lasts for 8-12 hours.
- Synthetic analogues: prednisolone, prednisone, methylprednisolone, mometasone, clobetasol. The substances act within 12-36 hours.
- Synthetic analogues containing fluoride: dexamethasone, betamethasone, paramethasone, fluprednisolone. The effect of the substances lasts up to 3 days.
Such substances have the following effects:
- Antiallergic. Hormones reduce the level of basophils - substances activated during allergies.
- Anti-inflammatory. Substances reduce the level of inflammatory mediators in the blood.
Hormonal drugs have a faster effect, but also have a more impressive list of side effects. For this reason, few hormonal ointments are approved for children, and they try to resort to them in extreme cases, when the child’s condition is advanced and he suffers from itching, large lesions and other unpleasant symptoms.
The list of hormonal drugs used for diathesis includes:
- Advantan (methylprednisolone) – from 4 months;
- Lokoid (hydrocortisone) – from 6 months;
- Afloderm (alclomethasone) – from 6 months;
- Beloderm (betamethasone) – from 6 months
- Dermovate (clobetasol) – from 1 year;
- Elokol (mometasone furoate) – from 2 years.
What are the dangers of using hormonal ointments for diathesis?
Because children have a larger surface area to weight ratio than adults, they are at greater risk for side effects from hormonal medications. With long-term use there is a risk of growth and development disorders. For this reason, children are prescribed minimal doses of ointments, as well as short courses. For example, Advantan cannot be used for longer than 4 weeks.
There are other features of the use of hormonal ointments associated with the small surface area of the child’s body. For example, Beloderm ointment is used very carefully and should never be applied under a diaper, since due to the increased absorption of the active components, the risk of developing serious side effects increases.
It is equally important to apply hormonal ointment with caution in the area of body folds. In these places, the ointment is absorbed more actively and can have a systemic effect on the body, that is, enter the bloodstream and influence from the inside.
In the case of hormonal ointments, it is also important:
- do not exceed the prescribed dosage;
- use the amount of ointment prescribed by the specialist;
- do not extend the period of use (in most cases no longer than 5 days);
- Apply only to the affected areas.
Causes and risk factors of acne
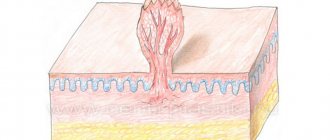
Acne develops around the hair follicles and is caused by excessive sebum production. Increased secretion of sebum in combination with the presence of dead skin cells on the epidermis leads to clogging of the follicles of the hair shaft, which is accompanied by the appearance of comedones.
Comedones are the same tiny sores with a white tip that turn black when exposed to oxygen. Exacerbation of acne is caused by the involvement of an infectious process. A moist and oily environment is a favorable substrate for the proliferation of acne bacilli (Propionibacterium acnes).
When the bacteria is present, an inflammatory reaction develops, with pimples forming a red plaque on the top of the skin. The final sign of acne is nodular acne, characterized by large inflammatory lesions that can hurt and even leave scars after recovery.
There are several factors that increase the likelihood that a child will develop acne:
- using skin and hair care products that contain chemicals that irritate the skin;
- using alkaline soap and very hot water;
- squeezing pimples and scratching affected areas of the skin;
- frequent stressful situations or constant nervous tension;
- excessive sweating and dandruff.
Learning what causes acne in children can help find ways to prevent and treat the disease. This allows the child to overcome the stress and depression that he experiences due to acne on his skin.
Endocrinopathies can be the cause of childhood acne. That is why, if you have acne, you should definitely consult a doctor to rule out such severe pathologies as congenital adrenal hyperplasia, malignant testicular tumors and polycystic ovary syndrome.
Hives
- Symptoms
Your baby may develop a rash in the form of blisters ranging in size from a few millimeters to several centimeters. Against the background of an acute allergic reaction, swelling may develop. Sometimes individual blisters merge with each other and affect large areas of the skin.
- Treatment
The doctor chooses a course of treatment depending on the cause of the condition. Thus, urticaria often appears as a reaction to insect bites, medications, pollen, foods, etc. This condition can be closely associated with systemic diseases, and sometimes occurs spontaneously. The basis of therapy is the exclusion of the factor that provokes this specific reaction. Your doctor may recommend a hypoallergenic diet even if your hives are not caused by food. If a reaction to cold, heat, or ultraviolet radiation occurs, the baby’s skin must be reliably protected from this factor. The doctor may prescribe antihistamines to treat allergies on the child's cheeks.
Symptoms of acne in children
Pimples appear on any part of the body. However, most often they appear in places where there is a high concentration of sebaceous glands.
The most commonly affected areas in children with acne include:
- Ears. Acne in a child's ears is localized behind the auricle, along the edge and on the lobe, closer to the temporal region at the upper base. Acne looks like blackheads or inflamed papules.
- Face. Acne on the face of a child is characterized by a few individual closed or open comedones. Closed ones are represented by yellowish or pearly-white papules, the size of which varies from 1 to 2 mm. Over time, they turn into open comedones, which look like blackheads.
- Nose. Acne on a child's nose appears as isolated pustules or papules - surrounded by a pink rim. Characterized by rapid (1-2 weeks) spontaneous resolution.
Also, acne in children can be localized on the chest, upper back and neck. After acne disappears, there are usually no traces left on the skin. The situation is complicated by infection - signs of inflammation appear (swelling, redness along the periphery). The elements transform into pustules with purulent discharge, which is yellow in color. In this case, it is quite difficult to avoid marks on the skin.
One of the methods of treating diathesis is local therapy.
The complex treatment of diathesis includes local therapy in the form of ointments and gels. They should only be prescribed by a specialist, and he takes this issue very seriously, since the main role in the appearance of signs of diathesis is given to allergens that affect the child’s skin.
What drugs are often included in the list prescribed by a doctor:
- To soften and quickly heal the skin: Bepanten, zinc ointment, Desitin (zinc-based ointment).
- For disinfection, softening and prevention of the formation of new crusts: Diaderm, Glutamol.
- To suppress an allergic reaction: Fenistil, Vibrocil, Cetrin.
It is worth considering that ointments are not the main way to treat diathesis, since they do not affect the cause in any way. Local therapy is used as an auxiliary method. The basis of treatment should be diet, proper care, and avoidance of contact with allergens.
How is this treated?
Traditional drug treatment includes the use of topical ointments as prescribed by a doctor, along with oral antibiotic therapy or internal medications.
External therapy most often involves the use of retinoid ointments, which reduce inflammation and help exfoliate the top layer of skin. Topical ointments can be used without a prescription. These drugs contain a small amount of active substance and are therefore safe.
In addition to medical attention, it is important to remember that acne develops in moist areas of the skin, so maintaining proper hygiene is important. Timely and thorough cleansing of the skin can significantly reduce inflammatory processes. It is important to give preference to the prescribed care products and not to rub or scratch the wounds, as this will cause additional irritation and worsen the inflammatory process.
You can use drugs with antibacterial action that will help eliminate the inflammatory reaction. You should never squeeze the blackheads because this will spread the bacterial infection and may also cause scarring on the skin.
Extra hydration and protection
Many people make the mistake of thinking that acne-prone skin does not need additional moisturizing. The truth is that adjusting your moisturizing emulsion can help balance sebum production throughout the day. Moisturizing emulsions are easily absorbed, helping to balance moisture levels and prevent aggravation or irritation.
Skin affected by acne needs constant protection from solar radiation, since exposure to direct ultraviolet rays promotes the secretion of sebum. You need to choose sunscreen according to your age and skin type. It is recommended to give preference to products that do not contain parabens.
Nutrition and lifestyle
Lifestyle also influences acne. Diet, stress and hours of sleep also negatively affect the condition of the skin. It used to be that certain foods contributed to acne. Today, a personalized diet is being promoted:
- It is recommended to reduce the consumption of sweet or spicy foods;
- reducing foods that are not beneficial mitigates damage.
In addition to dietary recommendations, you should also use Omega-3 supplements. These are polyunsaturated fatty acids that the body cannot produce on its own, and they are found in sea fish oil or plant products. Their presence will help mitigate inflammatory processes in the body, which means it will have a beneficial effect on all skin diseases and acne in particular.
Food allergies
Can you be allergic to breast milk? Alas, even a newborn baby is not immune from this. If we omit hereditary factors, an allergy to breast milk is most often associated with the diet of a nursing mother. Therefore, the basis of treatment in this case is a thorough analysis and adjustment of the mother’s menu. First of all, potential allergens are excluded: cow's milk (the baby's immune system views cow protein as foreign), chicken eggs, fish and seafood, mushrooms, nuts, honey and brightly colored vegetables and fruits. In the first 2–3 months of life, the baby’s digestive tract is just forming and there are no protective enzymes, so the young mother must be extremely attentive to what she eats. Even better, at the first sign of an allergy, start writing down your daily menu. This will greatly facilitate your further work with an allergist when making a diagnosis and prescribing treatment.
A doctor's help is also necessary if the baby is on artificial nutrition and the mother suspects that an allergic reaction is caused by components of the infant formula. In this case, after the examination, the allergist will prescribe a hypoallergenic diet for the child.
What are the symptoms of allergies in an infant? The entry of a foreign antigen into the baby’s body can be expressed in different ways:
- various rashes;
- peeling skin on the cheeks;
- diaper rash;
- constant nasal congestion;
- excessive regurgitation;
- vomiting and loose stools;
- difficulty breathing;
- Quincke's edema (in extremely rare cases).
Agree, some of these symptoms are extremely similar to prickly heat and diathesis. How to correctly identify them? Miliaria in the form of small blisters in the folds of the skin and on the neck usually does not cause discomfort to the baby and goes away without a trace after 2-3 days (provided there is no overheating in the future). Diathesis is nothing more than the first bell, forcing the mother to seriously think about the child’s tendency to allergies. It is directly related to the baby’s adaptation to the external environment and the formation of its gastrointestinal tract. The most common causes of diathesis are dry air, chlorinated water, washing powders and, of course, the mother’s improper diet. Diathesis is manifested by loose stools, a bright rash, red cheeks, but with proper therapy it disappears without a trace in the first years of life.