mole, pixabay.com There are no people in the world who do not have at least one mole on their body.
The only thing is that statistics say that the Negroid population has much fewer moles than white people. A mole is a pigmented formation. It can be congenital or acquired. They differ from each other in color and size. Over time, the formation may become larger, more convex, or, conversely, disappear. This often happens in children who are born with birthmarks - the children grow up, and the mark disappears.
Some have more moles, some have fewer, but the most dangerous and unpleasant thing is injury. Traumatizing the spot can cause severe bleeding. Moreover, constant trauma to the mole may lead to the development of various diseases. Most often they are dangerous to human life. This statement is controversial. Many scientists and doctors are still arguing about how much birthmarks can affect the body.
To understand this topic in more detail, we have compiled a series of questions.
- A mole is puffed up, what does this mean?
- There is a lump under the mole, what symptoms and diseases may occur?
- Bad moles - what are they?
- What to do if a mole bursts?
- The mole is swollen and itchy, what does this symptom indicate?
If you notice the symptoms from our series of questions, do not panic. Use the information provided in this article and be sure to consult a doctor!
Support the publication
- Join the CLAN
Or
The good and the bad
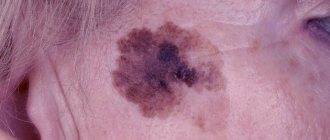
Moles can be very different - light or dark, flat or “rising”, superficial or embedded in the thickness of the skin, in a word, all sorts: both beautiful and ugly. What about the danger of their degeneration, which of them are the “bad”?
Doctors believe that the potential for degeneration into a malignant formation is much higher not in those moles with which we are born, but in those that appear on the skin later. And these are not necessarily raised or hairy moles, which most of us consider the most “bad” ones. Most often, it is flat formations that can be dangerous. Moles located on the soles, palms, inner sides of the shoulders and thighs, and especially in places with an increased risk of injury - for example, if a mole on the neck is often touched by a collar, etc., also degenerate.
The size of moles also matters: medium, large and giant moles can more often degenerate into melanoma. Therefore, even if such moles “live” in an inconspicuous place and do not cause much trouble, you still need to consult dermatologists-oncologists about them once a year.
Types of moles
Science identifies several types of moles:
- Dark spots
. Usually chocolate color, sometimes black. The color depends on the presence of melanin in the blood. - Vascular moles
. Usually red, sometimes bluish. Refers mainly to cosmetic defects. - Teratomas
. Such spots appear due to surges in hormone levels in the body.
Moles are usually small in size, but can be large. There are convex, flat, and smooth ones, less often covered with hairs.
Moles can be located in different parts of the body. Sometimes a mole forms on the mucous membrane. The appearance of such neoplasms on the tongue, choroid of the eyes, and genitals is becoming more common. This mainly happens to women.
Moles are not transmitted by airborne droplets.
Beware, provocateurs!
What provokes the process of degeneration of moles? First of all, insolation (stay in the sun). It is useless to protect moles from the ubiquitous sun's rays with a towel, a Panama hat, and even more so by covering them with a band-aid - the greenhouse effect deals a double blow. Solarium is no less dangerous; it is absolutely contraindicated for those who have many moles on their body.
Any injury to a mole can give impetus to the development of a tumor. Therefore, if you hit it with your fingernail or inadvertently damaged it with some sharp object, be sure to see a doctor.
By the way, those who have many moles on their body should wash only with a soft sponge, not a hard washcloth, and especially not rub their back with a brush. Moles that protrude above the surface of the skin are best washed carefully by hand.
Briefly about the main thing:
Itching alone is EXTREMELY rarely a sign that a mole has turned into melanoma. Most often it is caused by other reasons. In addition, the malignancy of the mole should be accompanied by symptoms other than the feeling that the mole itches
.
If you still have questions, the following will help you:
- In-person appointment with an oncologist
(St. Petersburg) - Mole removal
with histology (St. Petersburg) - My online consultation (from anywhere in the world)
Don't miss the threat
There are five signs that everyone needs to know about. They are the ones who can signal the first “bad” symptoms. Self-examination is easy:
● Mentally draw an axis through the center of the mole. Normal moles are “divided” into equal halves. Asymmetry is a danger signal. ● Examine the contours of the mole - with malignant degeneration, the edges become jagged. ● Check whether the mole changes color: there are no inclusions or veins. ● Monitor the size of “suspicious” (especially large moles). Periodically measure their diameter with a ruler and record the readings. ● Control any changes: size, volume, texture. If a mole suddenly begins to bleed or becomes painful, consult a doctor immediately! ● Once a year, a “technical examination” by a dermatologist-oncologist should also be done by those who have many moles and if they are large. It is advisable to see a doctor even after vacationing in hot regions.
How to recognize dangerous moles in time
What skin tumors in most cases turn into a malignant tumor, why this happens and how to save your life.
Melanoma is the most dangerous skin cancer. Under different guises, it is born from a nevus (mole, birthmark). During the development process, the tumor rapidly grows through the skin, then, by lymph and blood, it is transferred to other organs. Its new foci arise there. The result is death. None of the patients with late-diagnosed melanoma exceeded the five-year survival mark. Elena Ivannikova, chief physician of the Naja clinic, talks about how to properly use the life-giving rays of the sun.
— Elena Nikolaevna, everyone knows that the sun is the basis of life, it gives us strength. Warm days have arrived and northerners, hungry for the revitalizing rays of the sun, are taking sunbathing. Tell me, perhaps the talk about the unsafeness of spending time on the beach is greatly exaggerated?
— Of course, in moderate doses, sunlight gives us not only joy and good mood, but also health. It is also a good preventive and therapeutic agent for rickets, stimulates the production of vitamin D, strengthens the immune system, and is beneficial for some chronic skin diseases. Ultraviolet light for 10-15 minutes a day is beneficial.
However, the health hazard lies in excess sun exposure. And thermal burns, heat stroke, high blood pressure and photoaging are not the biggest problem.
According to the Moscow Research Oncological Institute named after. P. A. Herzen, in the 21st century, the incidence of melanoma in Russia has increased and continues to grow. The incidence of melanoma ranks third among all cancer incidence in Russia. On the first and second lines are lung cancer and breast cancer in women. Meanwhile, this type of skin cancer is often the downside of a beautiful tan.
— Now many people know that skin cancer can grow from a special mole. How to distinguish such a dangerous mole?
— There are no people without moles. If a mole suddenly changes shape, becomes asymmetrical, has uneven edges, is mottled, or turns black, show it to your doctor. If it starts to hurt, itch or bleed, this is also a cause for concern. Throughout life, nevi change throughout life. If a nevus appeared in childhood and has not changed at the age of 30-40, you should show it to a doctor.
A harmless spot is distinguished from melanoma by five signs, which are encoded in the word “ACORD”:
- A - asymmetry. Using an imaginary axis, the safe mole will be divided into two equal parts.
- K - edge, normally smooth and even.
- O - coloring. There should be no variegation.
- R - size. If the mole is larger than 5 mm, observe carefully. The danger increases if it is located on an open area of the body.
- D - dynamics. If wounds appear, increase in size or other changes, consult a doctor.
The presence of hair in a mole is more likely to indicate that it is benign, but if hair loss suddenly occurs, you should rush to see a dermatologist or oncologist.
In men, “bad” nevi are more often localized on the back. For women - on their feet. Dangerous moles are located on the palms, feet and in places of friction with shoes and clothing.
— What is the most common cause of a mole turning into cancer? And who is at greater risk of getting sick?
- Pigment formation can become cancer after injury or sunburn from radiation. The presence of such a terrible diagnosis in relatives increases the danger.
Moles turn into tumors when exposed to ultraviolet radiation in those who have:
- light skin (poor adaptation)
- light eyes
- blond and red hair
- many moles (over 50) and freckles
- elderly age.
The risk of developing melanoma in adulthood increases among those who were sunburned in childhood or more than three times during their lives.
— How to stop melanoma?
— Everyone should be wary of cancer.
Protect exposed skin from the sun. Once every 3-6 months, examine moles using mirrors and a camera, remember their appearance. If you find suspicious moles, immediately contact a dermatologist to examine the formation using dermatoscopy.
A dermatoscope is an optical device that magnifies the image tens of times. The doctor examines the mole using these optics and assesses the degree of danger. And in his conclusion he gives recommendations for treatment or removal. The study is non-traumatic. Safely. It is carried out within 10-15 minutes. Timely dermoscopic examination of moles and detection of melanoma at an early stage in most cases helps prevent further development of the tumor and save human life.
— Doctors do not recommend sunbathing from noon to 4 pm. But the northern sun is not as active as the southern one. Perhaps you can give more specific recommendations for our readers?
“Our fellow citizens joke that June is not yet summer in our city, August is not summer anymore, and July is depending on your luck. Indeed, sunny days in our region do not happen as often as we would like, but there are no concessions for us. Exposure to the sun during peak hours should be avoided.
— Elena Nikolaevna, I know that you worked as a dermatologist for many years. Your spouse is also a doctor. Does your family like sunbathing? Tell me, perhaps you don’t allow your children to sunbathe and avoid beach holidays?
- Not at all. After all, we are ordinary people. Sometimes, like everyone else, we vacation in the south. But we never forget about protection. When in the sun, we wear hats with wide brims or “visors,” sunglasses, and light, light-colored clothing made from natural materials. We do not visit the beach from 11.00 to 16.00. And if we happen to spend time on the beach, we apply protective agents to exposed skin. And children know the rules of caring for their health from childhood. Therefore, they are rather surprised why so many people neglect the simple rules of being on the beach.
— What should be the signal in order to understand that it is worth hiding in the shadows?
— Any changes in normal health are a reason to stop sun exposure and seek medical help.
— Pharmacy counters, like television advertising, are replete with a large number of skin protection products from UV rays. How to choose the right product that is suitable for your skin?
— It is better to use sunscreens that contain both UVA and UVB filters. In the first days, it is necessary to select a filter that will maximally protect the skin from the harmful effects of the sun (SPF 90+, 60+, 50+). Next, choose a sun protection factor that matches your skin type (SPF 30+, 15+).
Remember to apply the product 30 minutes before going out into the sun and additionally during prolonged sun exposure, as well as after swimming and drying.
The SPF number does not show the quality of protection, but the time that you can stay in the sun without getting burned.
I would like to add that a reasonable attitude towards the sun preserves not only health, but also youthful skin. After all, skin aging in 80% of cases is premature aging (photoaging). Intense tanning is a damaging factor for the skin, leading to dehydration,
coarsening, loss of elasticity and the appearance of stains, which are not easy to get rid of later.
Basic rules for preventing skin cancer:
- don't be a tanner
- Always protect your skin from active sun
- do not injure moles
- Once a year, come for an examination to a dermatologist-oncologist
- As recommended by your doctor, examine and remove suspicious skin lesions.
Healthy skin is a sign of beauty, be careful with it and monitor its condition!
Goodbye problem!
Where to go, what to do if you want to remove a mole? Definitely - not to a beauty salon, but only to a dermatologist-oncologist.
An experienced specialist will determine the condition of the mole visually. In some cases, special equipment is used for diagnosis, which makes it possible to make an accurate diagnosis. If “bad” suspicions arise, histology is required - examination of the removed tissue.
Which method is better: electrocoagulation, laser or cryodestruction?
Cryodestruction (burning out formations with liquid nitrogen) is used only to remove warts or papillomas - that is, formations of viral origin, since this is not a radical removal. A mole often lies deep in the tissue, and if it is not completely removed, it can “sprout” again. The laser excises the mole, but this is a more traumatic operation.
The most preferred method is electrocoagulation: its main advantage is that after surgery the tumor can be sent for histological examination (neither laser nor liquid nitrogen provide this opportunity). During electrocoagulation, local anesthesia is performed, and the operation itself lasts from 5 to 20 minutes.
What can cause discomfort?
Do you occasionally want to scratch a mole? This desire may be caused by:
- carcinophobia - people who are very afraid of getting skin cancer often feel that their nevi are growing, inflamed or itchy,
- other psychological factors - every person regularly experiences causeless, mild itching of certain parts of the body or face,
- an insect bite or an allergy - normally, nevus cells are almost no different from the surrounding epidermis, so they can react with itching to contact with aggressive substances,
- skin disease - eczema, psoriasis, various skin infections can cause an indomitable desire to scratch,
- damage to the upper layer of the epidermis - abrasions and rubbed areas often cause discomfort when touched.
What then?
After removing a mole, a mini-scar remains in its place, then a crust forms. For 1–2 weeks, until the wound heals, it will need to be lubricated several times a day with a strong solution of potassium permanganate or other antiseptic and healing-accelerating agents. At this time, it is forbidden to visit the bathhouse or swimming pool, or take a shower - the wound must not be wetted. If the mole was on your face, you should not wash your face - wipe the skin with a cotton pad soaked in cleansing lotion, carefully apply the cream, but it is better to avoid decorative cosmetics for a while.
You should not try to get rid of the scab until it falls off on its own, otherwise healing will slow down. It is advisable to come for a follow-up examination with a doctor 7–10 days after the operation.
What to do if a mole is swollen
When a hanging nevus swells, it is forbidden to apply a cotton swab soaked in alcohol or iodine to the inflamed area. If itching and burning occurs on a swollen mole, you should avoid contact of the mole with external irritants and do not scratch. If severe itching is present, you can relieve the condition with a vinegar solution. To do this, soak a cotton swab in a weak vinegar solution and apply it to the itchy area for 5 minutes. If the mole is swollen and painful, it is not recommended to press on it while wetting it with a vinegar solution. After applying the tampon, lubricate the bladder with three percent hydrogen peroxide. This will reduce the risk of infection getting inside the growth.
Other dangerous symptoms
If a mole begins to transform into melanoma, that is, become malignant, redness of the skin is not a single symptom; it is accompanied by some other negative manifestations. The presence of at least one of them should already serve as a signal to contact a specialist, and the combination of several factors literally obliges you to do this in the near future. Symptoms of nevus malignancy include:
- pain, itching, bleeding;
- change in color, structure, outline, shape;
- the appearance of asymmetry;
- the appearance of cracks on the surface;
- the appearance of black or red dots;
- thickening of the mole and the skin around it;
- inflammatory process;
- appearance of a white halo.
If such symptoms occur, only a qualified specialist can help. You cannot self-medicate, giving preference to cheap pharmaceuticals or traditional medicine recipes, since melanoma can only be removed surgically. All other methods will only damage it, but the infected cells will continue to spread throughout the body at a faster rate, which will very soon cause complications.
What to do if redness and inflammation appear
If you notice that the skin around one of your moles is red and inflamed, you should contact a dermatologist or oncologist for advice without panic. There is no need to be afraid of this, because in most cases the examination results can be obtained almost immediately. If the fears are confirmed and the redness turns out to be a symptom of malignancy, the necessary tests and subsequent surgery will be prescribed. If there is no cause for concern, the specialist will prescribe a pharmaceutical remedy that relieves inflammation.
You can find out from your doctor whether certain traditional recipes are suitable for you; it is not recommended to use them without consultation with a specialist in order to avoid complications and side effects.
If the initial visual examination of the nevus is insufficient to make an accurate diagnosis, the doctor may prescribe additional tests - dermatoscopy and siascopy. These are absolutely painless procedures that are performed non-invasively, that is, without damaging the skin. Dermatoscopy allows you to look at the tumor under magnification using a device that operates on the principle of a microscope. Siascopy is performed with a special scanner, which allows you to study the composition of the mole in more detail. In particularly difficult cases, a biopsy is prescribed, which involves taking a certain amount of nevus tissue for subsequent analysis of the nature of its occurrence.