Trichophytosis
The symptoms of trichophytosis depend on the form of the disease, the type of pathogen and the characteristics of the patient’s body, although the superficial, infiltrative and infiltrative-suppurative forms represent the sequential development of one pathological process. And in the absence of adequate treatment, the superficial form of trichophytosis can turn into infiltrative-suppurative.
Superficial trichophytosis occurs on the scalp and on smooth skin, externally manifested by rounded lesions, sharply limited from healthy skin. The incubation period is about a week, after which clinical manifestations begin - small areas of grayish-pink skin with uneven outlines and slight peeling. In the lesions, most of the hair is broken off at the level of the skin or 2-3 mm from it; if the hair on the head is dark, then you can see dark spots - hair stumps. Sometimes the hair in the area affected by trichophytosis curls and bends; in some cases, the hair is covered with a grayish-white coating, which consists of fungal spores. There is no itching or any other subjective sensations. On the periphery there are blisters, purulent nodules and crusts in the form of a border. Pityriasis peeling is most intense in the center of the lesion, and is practically not observed closer to the periphery. If there is no peeling or intense hair breakage, but there are stumps characteristic of trichophytosis, then it is necessary to conduct an additional examination to exclude or confirm the diagnosis of “Trichophytia.”
Chronic forms of superficial trichophytosis begin in childhood and its difference is that it does not go away by puberty, although it is caused by the same pathogen. The pathogenesis of chronic trichophytosis is a lack of vitamin A in the body, endocrine dysfunction of the gonads and other endocrine glands and autonomic nervous disorders (vegetative-vascular dystonia), which reduce the body's protective reactions. The lesions are localized in the occipital and temporal areas of the head; there is fine focal or diffuse peeling. There are areas with broken hair; with long-term trichophytosis, areas of skin atrophy with small, delicate scars appear. Sometimes barely noticeable scales on the scalp, the color of which acquires a lilac tint, are practically unnoticeable; black dots from broken hair are also revealed only upon careful examination.
Smooth skin affected by chronic trichophytosis is bluish with the presence of gray thin scales. Most often, the skin in the buttocks, inner thighs, forearms and elbows is affected; trichophytosis is less common on the face and upper body; widespread distribution of trichophytosis throughout the body is observed in isolated cases. The skin pattern is pronounced; the stratum corneum may thicken, causing furrows to appear on the palms and soles of the skin; the furrows eventually turn into cracks. When affected by trichophytosis of the palms and soles, blisters never form. Bubbles, crusts and nodules are also not typical for chronic trichophytosis.
Sometimes the infection spreads to the nails, although trichophytosis of the nails can occur without affecting the skin. The nails thicken, become lumpy, rough to the touch, and grayish-white spots and stripes can be seen on the free edge of the nail. The supracungual plate is not inflamed, there is no itching or discomfort.
Infiltrative-suppurative forms of trichophytosis are caused by a zoophilic type of fungus; such forms of the disease are more common in people living in rural areas. A bluish-red infiltrate with a diameter of up to 8 cm appears on the scalp, protruding above the skin level; if there are several infiltrates, then when they merge, they form an extensive purulent conglomerate of bizarre shapes. In this case, the inflammation has clear boundaries and does not spread to neighboring areas of the skin; the inflammation site is usually round or oval in shape.
The surface of the trichophytosis infiltrate is often ulcerated. Around it there is a roller consisting of plaques, small bubbles and dried crusts. After some time, a pustule forms around each hair, after the final formation of which, the hair in the affected area becomes loose and begins to fall out. From the dilated hair follicles, when pressed or accidentally pressed, droplets and sometimes streams of pus are released; the area affected by trichophytosis is very painful when touched. In the infiltrative-suppurative form of trichophytosis, vellus hair is also involved in the process, but unlike long hair, it does not break off. The surface of the scalp with trichophytosis is similar to a honeycomb, and if the suppurative-infiltrative form of trichophytosis is observed in the area of the beard and mustache, then the affected areas resemble wine berries. After 7-10 days, the infiltrate begins to soften.
Suppurative forms of trichophytosis may be accompanied by symptoms of intoxication: general weakness, elevated body temperature, enlarged and painful regional lymph nodes, loss of appetite. In the absence of treatment, suppurative forms of trichophytosis resolve on their own, since the developed suppuration is detrimental to the mycelium of the fungi, but mycotic cells remain on the periphery and in scales along the edge of the lesion. In some cases, suppurative forms of trichophytosis are complicated by abscesses.
Epidemiology of the disease
The most common trichophytosis in the Russian Federation is caused by anthropophilic fungi Trichophyton tonsurans and Trichophyton violaceum (the most common). The fungus causes sporadic outbreaks of mycosis in families, schools, kindergartens and boarding schools. More often children get sick who become infected from sick adults (mothers, grandmothers) suffering from chronic forms of the disease. When infected, a superficial form of the disease develops.
Zoophilic trichophytons Trichophyton mentagrophytes v.gypseum and Trichophyton verrucosum are the cause of the development of infiltrative-suppurative trichophytosis. The source of pathogenic fungi is animals.
Sources of infection
- Anthropophilic trichophytosis: a sick person.
- Zooanthroponotic trichophytosis: the source of Trichophyton verrucosum is large domestic animals (cattle, horses, calves, donkeys and goats, as well as wild animals), Trichophyton mentagrophytes is small animals (mouse-like rodents, gophers). Transmission of infection from a sick person is possible.
Transmission factors
- Anthropophilic trichophytosis: hair of the patient, skin scales and crumbling nail plates of the sick person.
- Zooanthroponotic trichophytosis: hay, straw, dust (in autumn during field work), wool of sick animals.
Transmission routes
- Anthropophilic trichophytosis: the patient’s clothes, his personal belongings (towels, combs, razors, scissors, hats, scarves, bed linen, etc.). Wrestling athletes are affected by contact from patients with trichophytosis of smooth skin (lichen of the trunk of gladiators).
- Zooanthroponotic trichophytosis: by contact through objects contaminated with sick animals (brushes, bedding, feeders, etc.).
Incubation period
- Anthropophilic trichophytosis (superficial) - 1 week.
- Zooanthroponotic trichophytosis (infiltrative-suppurative) - 1-2 weeks - 2 months.
Rice. 2. Calves are often the source of Trichophyton verrucosum.
Main forms of the disease
There are superficial and chronic forms of trichophytosis, caused by anthropophilic fungi of the endothrix type Trichophyton tonsurans and Trichophyton violaceum, and deep infiltrative-suppurative form, caused by zoophilic fungi of the exothrix type Trichophyton mentagrophytes v.gypseum, Trichophyton mentagrophytes var. interdigitale and Trichophyton verrucosum. The disease affects the scalp, smooth skin (superficial and deep layers), nails (in the chronic form of the disease) and internal organs.
The incubation period for the superficial form of the disease is 1 week, for the infiltrative-suppurative form - from 1 week to 2 months.
Skin damage, weak immunity, prolonged contact with infection and the presence of endocrine pathology contribute to the development of mycosis.
Rice. 14. Trichophytosis on the face of a child.
Ringworm in children: features of the disease
Ringworm occurs in almost 90% of children, affecting the skin of both infants and older children. Occurs in adolescence. There are many types of disease, and accurate differentiation allows for the most appropriate therapy. The help of a doctor (pediatrician, mycologist, dermatologist) in this case is irreplaceable: firstly, the doctor will make the correct diagnosis by conducting the necessary tests (lichen rashes are similar to many other skin lesions), secondly, he will prescribe appropriate treatment taking into account all indications, severity and age of the child. Each type of lichen requires a different approach and duration of use of certain means. Therefore, before treating lichen in a child, the correct diagnosis should be made. It is almost impossible to do this on your own.
The symptoms of all types of disease are similar. Ringworm in children manifests itself as scaly spots, barely noticeable at first, then more pronounced. Their color ranges from light pink to bright red, and may turn brown over time. The spots are itchy, the scales look like whitish flakes. Children, especially younger ones, may have a fever; lymph nodes enlarge. Spots appear on the neck, chest, back, shoulders, stomach and thighs; some types of fungi “live” on the head and nails.
Diagnosis of the disease
Diagnosis of trichophytosis is carried out on the basis of the clinic, microscopic and microbiological examination data. Skin flakes, nail plates and affected hair are subject to examination. Serological studies are carried out in the chronic form of the disease. Intradermal tests are performed with allergens such as trichophytin. There is no glow in the rays of a Wood's lamp (with microsporia the glow is emerald in color).
Rice. 36. Trichophyton verrucosum under a microscope (photo on the left). Growth of a Trichophyton mentagrophytes colony on a nutrient medium.
Rice. 37. Microscopy of hair determines the tissue form of trichophyton. Endothrix (photo on the left), when fungal spores are located inside the hair. Ectotrix (photo on the right), when fungal spores are located on the surface of the hair.
Prevention
The basis of preventive measures is:
- Strict adherence to the rules of personal hygiene: do not use other people’s personal hygiene items, underwear, clothes, wash your hands thoroughly after contact with animals.
- Early (timely) identification of patients with trichophytosis with their isolation and quarantine of contact persons.
- Identification of animals with trichophytosis, carrying out deratization work.
- Carrying out current/final disinfection at infection sites (in schools, kindergartens, at home, bathhouses, hotels, hairdressers, medical institutions, dormitories, etc.).
List of sources
- Leshchenko V. M. Fungal skin diseases. In the book: Skin and venereal diseases (a guide for doctors). Ed. Yu. K. Skripkina, V. N. Mordovtseva. M., 1999. T. 1. P. 257-311.
- Kubanova A.A., Potekaev N.S., Potekaev N.N. Guide to practical mycology. – Moscow, Financial Publishing House “Business Express”, 200 p.
- Bayazitova A.A., Bayazitova A.A., Kupriyanova-Ashina F.G., Khaldeeva E.V., Ilyinskaya O.N. Primary pathogens - Pathogens of superficial mycoses // International Journal of Applied and Basic Research. – 2015. – No. 11-2. – pp. 241-248.
- Medvedeva T.V. Trichophytosis: modern ideas about the etiology, clinical picture, features of diagnosis and therapy / T.V. Medvedeva, V.B. Antonov, L.M. Leina, T.S. Bogomolova // Klin. dermatology and venereology. - 2007. - No. 4. - P. 70–74.
- Rodionov A.N. Fungal skin diseases (Guide for doctors) St. Petersburg: Peter. 1998. – 288 p.
Methods for eliminating fungal infections
Treatment of trichophytosis requires the attention of a qualified specialist. In most cases, therapy is carried out at home. To successfully combat fungus, an integrated approach is essential: medications for external and internal use, and physiotherapeutic methods are used.
Treatment of trichophytosis with medications
Modern medicine offers the dermatologist a wide selection of antifungal agents. The pathogen is usually treated in a complex manner: ointments are applied topically, and drugs are taken orally in the form of tablets or capsules.
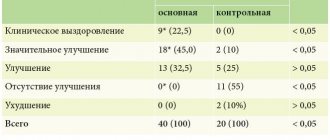
Local and general treatment of trichophytosis - table
| Preparations for external treatment of trichophytosis | Systemic treatment of trichophytosis | ||||
| Name of medicine | Active substance | Release form | Name of medicine | Active substance | Release form |
| Exoderil | Naftifin | Solution | Itrazole | Itraconazole | Capsules |
| Keto plus |
| Shampoo | Sangviritrin |
| Pills |
| Oflomil varnish | Amorolfine | Nail polish | Exifin | Terbinafine | Pills |
| Fungoterbin | Terbinafine |
| Mikosist | Fluconazole | Pills |
| Sangviritrin |
|
| Orungal | Itraconazole | Capsules |
| Mikoderil | Naftifin |
| Binafin | Terbinafine | Pills |
| Lamisil | Terbinafine | Cream | Rumicosis | Itraconazole | Capsules |
| Exifin | Terbinafine | Cream | Diflazon | Fluconazole | Capsules |
Antifungal agents - photo gallery
Exoderil is available in the form of a cream for external use.
Oflomil is available in the form of nail polish
Lamisil is an antifungal agent for external use.
Exifine contains terbinafine
Orungal is a drug for the systemic treatment of trichophytosis
Diflazone contains fluconazole
In addition to antifungal agents, a number of additional drugs are prescribed for the treatment of trichophytosis:
- antiallergic medications (Zodak, Loratadine, Suprastin);
- drugs that improve blood circulation (Troxevasin, Trental);
- antioxidants that improve the healing of damaged skin (Actovegin);
- immunomodulators that activate the body's defenses (Thymogen, T-activin).
Thymogen improves immunity
Physiotherapy
Physiotherapy is an effective method of treating many diseases, including superficial and deep trichophytosis. Specialists prescribe the following types of procedures:
- electrophoresis with iodine allows you to disinfect the lesion;
- iontophoresis with iodine can successfully replace the previous procedure;
- inductothermy (magnetic field treatment) improves blood circulation in problem areas of the skin;
- Ultrasound therapy in the area of the nearest lymph nodes leads to the activation of one’s own immune mechanisms to fight the fungus.
Household recommendations
Treatment of trichophytosis is often a long and difficult process. The patient must follow a number of recommendations that will speed up recovery and prevent the spread of infection:
- for trichophytosis of the head, the hair is shaved once a week until complete recovery;
- if the feet are affected, it is necessary to disinfect the inner surface of the shoes once a week with a cotton swab soaked in a solution of Chlorhexidine;
Chlorhexidine solution perfectly disinfects shoes - it is necessary to use individual personal hygiene items - a comb, a towel and other linen, manicure accessories;
- shoes must be chosen that are comfortable, fit, made from natural materials, and well ventilated.
Treatment of trichophytosis in children is the task of an experienced specialist. The principles of therapy are similar to those in adults. Doses of antifungal agents used orally are calculated depending on the age and weight of the child.
Folk remedies are not used in the treatment of trichophytosis because they have not proven their effectiveness.
Pathogenesis
The pathogenesis of dermatophytosis is based on the virulence factors of fungi, due to their ability to secrete enzymes that destroy keratin (keratinolytic activity). The enzymes secreted by dermatomycetes and their metabolic products, as well as the contents of destroyed cells, cause an inflammatory process in the lesion, manifested by redness of the skin, itching and hair breaking. Keratinases have the ability to decompose not only keratin, but also other proteins (collagen and elastin), and it is the severity of keratinase activity that determines the characteristics of the manifestation of diseases when infected with various types of fungi. An important role in the spread of dermatomycetes is played by the presence of a specialized apparatus (perforator organs) for the directed growth of hyphae (the filamentous structure of the fungus). Thanks to this feature, the fungus grows in the direction of the intercellular junctions, which are the points of least resistance. Dermatomycetes, as a rule, do not penetrate deeper than the granular layer of the epidermis, since specific protective factors are activated at a deeper level.
The process of fungal invasion begins with the burrowing of hyphae into the skin and the release of keratinases (enzymes for the breakdown of keratins), which leads to irritation of nerve endings and, accordingly, the occurrence of itching. Dermatomycetes, loosening the cortex, cause acanthosis, parakeratosis, serous inflammation in the skin with the formation of blisters. Further, swelling occurs in the papillary/subpapillary layer, the vessels dilate, which leads to the development of polymorphic perivascular infiltration. The mycelium is usually located between the horny plates. Threads and spores of fungi can also be stuffed with hair follicles, which also undergo inflammatory changes.
Differences from microsporia
Quite often, trichophytosis is confused with microsporia.
But these diseases are characterized by the presence of certain distinctive features. Trichophytosis is popularly called lichen. During the pathological process, hair breaks off. This is why it feels like the hair has been cut. Trichophytosis and microsporia are fungal diseases. The distinctive features between them are fungi, which cause a pathological process . Ringworm occurs due to exposure to trichophyton fungi, and microsporia occurs due to microsporum. Since these diseases are characterized by almost the same symptoms, they are both called ringworm.
Trichophytosis and microsporia are quite difficult to distinguish. That is why, to determine ringworm, the patient is recommended to undergo appropriate laboratory tests.