Skin melanoma treatment stages 1, 2, 3. Symptoms, signs, metastases, prognosis.
Content:
- General information about melanoma
- What are the different forms of melanoma? Superficial spreading melanoma
- Nodular melanoma
- Malignant lentigo melanoma
- Acral melanoma
- Atypical (dysplastic) nevi
- Primary metastatic melanoma
- Surgical treatment of skin melanoma
Why is it worth treating melanoma in Israel, at the Ichilov Cancer Center?
- Diagnostic accuracy. The oncology center employs the best pathologists in the world with extensive experience in diagnosing melanoma, so an error in diagnosis is excluded here.
- World-renowned oncologists and oncosurgeons. At the Oncology Center you will have the opportunity to undergo treatment for metastatic melanoma with Professor Yakov Schechter. The professor heads the Institute for the Study of Melanoma, where unique methods for treating this disease in late stages are being developed.
- Modern methods of treatment. The oncology center uses:
- TIL protocol for the treatment of metastatic melanoma (tumor infiltration with lymphocytes).
- targeted therapy with BRAF inhibitors;
- immune therapy with drugs based on monoclonal antibodies (ipilimumab, tremelimumab, pembrolizumab, etc.);
After this treatment, many patients with stage 4 melanoma live for many years.
General information about the origin of melanoma
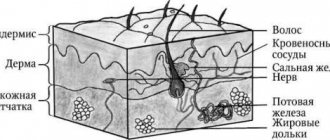
Melanoma is a malignant tumor formed during the degeneration of melanocyte cells, which in the normal state are located mainly in the skin and produce a coloring substance, the pigment melanin, under the influence of ultraviolet radiation.
The number of these cells and the pigment they produce determines the color of a person's skin. Melanocytes are contained in large numbers in pigmented (melanocytic) nevi, called moles in everyday life, so melanoma can also develop from these fairly harmless formations, which most people have.
The term "melanoma" comes from the Greek word "melanos" (dark, black). However, it is rare to see non-pigmented melanoma variants. The tumor is overwhelmingly found on the skin, but can also be located on the mucous membrane of the oral cavity, female genital organs, gastrointestinal tract, eyeball, etc.
Causes of melanoma
Melanoma develops as a result of atypical reproduction and malignant degeneration of melanin-producing skin cells (melanocytes), which are normally responsible for the color of the skin.
Normally, skin cells develop in a controlled and orderly manner: new healthy cells push old ones to the surface, where they die and eventually slough off. But when DNA damage occurs in some cells, new cells can begin to grow uncontrollably, leading to tumor formation.
It is currently unclear what exactly damages DNA in skin cells and how exactly this leads to melanoma. This is believed to be the result of many environmental factors. However, doctors believe that exposure to ultraviolet (UV) radiation from the sun, tanning lamps and tanning beds is one of the key causes of melanoma.
However, ultraviolet rays are not a trigger for all melanomas, especially those that occur on covered areas of the body that are not exposed to sunlight. This indicates that other factors may also influence tumor development [3].
Who is at risk?
Although the exact causes and mechanisms of melanoma development are still being studied, risk factors that are associated with malignant degeneration of skin pigment cells have already been clearly identified.
Among them [3]:
- Bright skin. Less pigment (melanin) makes the skin more susceptible to ultraviolet radiation. People with blond or red hair and blue eyes are thought to be more likely to develop melanoma than people with dark skin color.
- Previous sunburn. One or more severe sunburns that cause blistering may increase the risk of melanoma.
- Excessive exposure to ultraviolet radiation. UV radiation from the sun and tanning beds increases the risk of skin cancer.
- Accommodation in the equatorial zone. People living closer to the Earth's equator receive higher doses of ultraviolet radiation than residents of northern or southern latitudes.
- A large number of moles (nevi). Having more than 50 common moles on your body indicates an increased risk of developing melanoma.
- Family history of melanoma. The likelihood of developing melanoma is higher in people who have close blood relatives who have experienced this pathology.
- Frequent traumatization of nevi. These could be injuries sustained during shaving, as a result of wearing jewelry, underwear or other items of clothing (for example, backpack harnesses). In such cases, the risk of malignant degeneration reaches 90%2.
- Weakened immune system. People with compromised immune systems have an increased risk of melanoma and other skin cancers. Most often this is associated with taking medications to suppress the immune system, for example, after organ transplantation or in autoimmune pathologies and HIV infection.
What are the different forms of skin melanoma?
The main clinical forms of melanoma are:
- superficial spreading (39-75%);
- nodal;
- malignant lentigo melanoma;
- acral melanoma.
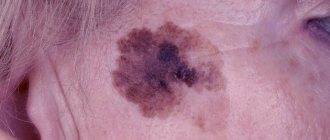
Superficial spreading melanoma (flat, radially growing melanoma)
The tumor develops equally often both on unchanged skin and from a pigmented nevus. It can be localized on open and closed areas of the skin, mainly on the lower extremities in women and the upper half of the back in men. It is a plaque of irregular configuration with a scalloped outline, areas of regression and discoloration, mosaic coloring, and keratosis on the surface. On average, after a few years, a node appears on the plaque, indicating the transition of horizontal growth to vertical.
Nodular melanoma
Nodular melanoma, accounting for 10-30% of all skin melanomas, is the most aggressive type of tumor. The neoplasm usually appears on unchanged skin. Clinically it is a node, less often a polyp-like formation on the skin. Patients note a rapid, within several months, doubling of the node's volume, its early ulceration and bleeding. The most common localization is the skin of the back, neck, head, and limbs. Histologically, invasion of atypical melanocytes to different depths of the dermis and subcutaneous fat is revealed.
Malignant lentigo melanoma
Melanoma of the lentigo maligna type accounts for about 10-13% of all melanomas and is characterized by a long horizontal growth phase. In typical cases, it occurs in older people on open areas of the skin of the face and neck in the form of black-brown spots or plaques. This type of melanoma is less aggressive than other flat melanomas.
Acral melanoma
Acral melanoma occurs in the nail bed and accounts for about 8% of all skin melanomas. It usually appears as a dark spot under the nail, which makes its timely diagnosis extremely difficult.
Relapse groups
In 1985, the domestic oncologist Anisimov proposed, for the convenience of describing the clinical picture, to divide recurrent tumors into six groups:
- The first - round and few formations, often outside the scar and mainly subcutaneously - in the fatty tissue, often fall under the criteria of “transit” metastasis according to Wagner.
- The second is multiple irregular cutaneous and subcutaneous infiltration accompanying vessels and nerves; it is assumed that the external picture of relapse is formed by tumor cells that have taken root in small vessels.
- The third is nodules directly associated with the operation area that have grown from malignant cells remaining in the skin.
- The fourth is polycyclic multiple formations.
- The fifth is a lot of bulging nodules, often on a stalk, like morel mushrooms.
- The sixth is a combination of all five options.
Classification is rarely used in clinical practice, because the assessment of treatment results is based solely on the size of the nodes, and not on their appearance.
Some epidemiological aspects (statistics) of skin melanoma
Melanoma occurs approximately 10 times less frequently than skin cancer and accounts for 1–4% of the total structure of human malignant neoplasms. This tumor is one of the most malignant and is characterized by rapid growth and early rapid lymphogenous and hematogenous metastasis.
About half of melanoma cases occur in people aged 30–50 years. It is extremely rare that a tumor can develop in children. Melanoma can develop on the skin of any area of the body, but its favorite localization in women is the lower extremities (lower leg), and in men - the torso (back). In older people, the tumor is somewhat more often localized on the skin of the face.
Over the past ten years, the annual number of cases of skin melanoma in Belarus has increased 1.5 times: from 461 cases in 2001 to 676 in 2010. In general, every 6-8 years the number of patients with melanoma doubles in the world.
In approximately half of the cases, melanoma develops on apparently healthy skin, in other cases - on the site of congenital or acquired pigmented nevi and Dubreuil's melanosis.
How does the quality of drugs affect the cure for melanoma?
Current treatment for advanced melanoma often includes targeted and immune-based drugs. Their cost is usually quite high, so it is important that the authenticity and high quality of these medicines are guaranteed. This is why they are worth purchasing in Israel:
- Israeli drugs are reliably protected from counterfeiting. The guarantor of the authenticity and high quality of medicines in Israel is the Ministry of Health, which exercises strict control over the production and sale of medicines.
- New medicines are being rapidly introduced in Israel. In this country, approval of a drug does not require a lengthy bureaucratic procedure.
- The Israeli pharmaceutical company TEVA is one of the most advanced in the world. Medicines from this company are prescribed in 60 countries.
Risk groups and factors predisposing to the development of skin melanoma.
Individuals at increased risk of developing melanoma include:
- with white skin, red hair, blue, gray or green eyes;
- constantly sunburned;
- those who have suffered sunburn and have been exposed to the sun for a long time, especially under the age of 20;
- having close relatives with melanoma (other skin cancer);
- having more than 100 moles on the body or more than 50 before the age of 20;
- having Dubreuil's melanosis (precancerous skin disease).
There are well-known cases of melanoma being diagnosed after injury to a pigmented nevus of the skin (mole). Melanoma often occurs after accidental or intentional (cutting, burning) injury to a mole. Sometimes 1-2 injuries are enough for melanoma to occur.
Trauma to the nevus can be chronic and occur unnoticed. For example, a well-starched shirt collar can injure moles on the neck, and bras can injure moles on the torso. Moles localized on the soles of the feet, palms, and perineum are chronically injured.
The influence of certain hormones on the development and clinical course of melanoma is assumed. Puberty, pregnancy and menopausal changes are regarded as risk factors for the development of melanoma from pigmented nevi.
Genetic predisposition plays a role (familial cases of melanoma).
Melanoma survival prognosis
Survival rates for melanoma, depending on race, are presented in the table:
| Race | Five-year survival rate |
| white | 93% |
| African | 69% |
| all races | 93% |
The probability of developing skin melanoma according to statistics depending on age and gender:
| Age | from birth to 49 years | from 50 to 59 years old | from 60 to 69 years old | from 70 years and older |
| Floor | ||||
| male | 0,50% | 0,40% | 0,90% | 2,5% |
| female | 0,50% | 0,40% | 0,50% | 1,0% |
Clinical manifestations of skin melanoma
Melanoma is one of the most dangerous types of malignant tumors. The insidiousness of melanoma is that, once it occurs, it can develop unnoticed in the superficial layers of the skin for several years, and then quickly spread through the lymphatic and blood vessels to other organs (lymph nodes, lungs, brain, liver), where they arise. new foci of its growth (metastases).
Melanoma usually appears as a painless, flat skin growth or nodule. Melanoma can vary in color: black-blue, brown or pink. Sometimes the tumor can have several shades at once (uneven distribution of pigment).
Thin melanomas without ulceration have a more favorable course. With nodular forms and the presence of ulceration on the surface of the tumor, the risk of developing metastases is very high.
At an early stage (thin and flat tumors), surgical excision can get rid of the tumor for a period of 5–10 years in more than 90% of patients. On the contrary, for tumors more than 4 mm thick and especially ulcerated, the five-year survival rate without recurrence of the disease is no more than 50%.
The chances of cure sharply decrease if you try to remove the tumor yourself (cutting, tying the “leg” of the tumor, burning with various chemicals, etc.).
Preventive measures
In its early stages, melanoma is highly treatable. However, the success of therapy primarily depends on the timely detection and treatment of cancer.
If you notice a new mole or suspicious spot on your skin, you need to go to a dermatologist for examination as soon as possible. Timely diagnosis is especially important if your immune system is weakened by HIV or another infectious disease.
Consistent use of sunscreen is one of the best ways to prevent skin cancer. It is also advisable to wear clothing that protects from solar radiation, for example, T-shirts made of special material that does not transmit ultraviolet rays.
You should definitely familiarize yourself with the classic method for diagnosing melanomas called “ABCDE”. It will help you determine how dangerous a particular mole may be.
How is skin melanoma diagnosed?
The most effective method for early detection of skin melanoma is periodic self-examination of the skin. There is a kind of “melanoma alphabet” that describes a number of signs of degeneration of a mole, indicated by the first four letters of the Latin alphabet:
- A (asymmetry) - asymmetry: the shape of “good” moles is often symmetrical;
- B (border irregularity) - the edges of the mole are usually smooth and clear. An uneven, scalloped outline is more characteristic of melanoma;
- C (color) - benign nevi are colored more or less evenly. The unequal color of different parts of the neoplasm is more characteristic of a degenerated mole;
- D (diameter) - the diameter of a mole is more than 6 mm: the larger the mole, the greater the likelihood of its degeneration. Malignant degeneration is indicated by various kinds of changes in a pre-existing mole. It was found that pigmented formations on the skin that regularly changed shape and color turned out to be melanoma 4 times more often than those whose appearance remained unchanged. Therefore, to the first four letters of the “alphabet of melanoma,” a fifth was added;
- E (evolving) - the appearance of any external changes in the mole, which most often are: change in color (decrease or sharp increase in pigmentation); violation or complete absence of skin pattern in the area of the nevus, “varnish” surface or peeling; the appearance of an inflammatory areola around the mole (redness in the form of a corolla); change in configuration along the periphery, blurring the contour of the nevus; an increase in the size of the nevus (especially over the age of 30) and its compaction; itching, burning, tingling in the mole area; the appearance of cracks, ulcerations in the mole area, bleeding; loss of existing hairs on the mole; sudden disappearance of a mole (especially after tanning in the sun or in a solarium).
Very valuable additional clarifying information can be obtained by performing a dermoscopic examination of a pigmented skin tumor, which allows for a visual assessment of the tumor at 10-40x magnification.
Can melanoma be prevented?
The most important way to reduce your risk of melanoma is to reduce your exposure to intense sunlight.
Stay in the shade. The simplest and most effective way to limit your exposure to ultraviolet rays is to minimize your exposure to sunlight. This is especially important from 10 a.m. to 4 p.m., when the effects of ultraviolet rays are most pronounced. Remember that the sun's rays can be reflected from water, clouds, sand, cement and snow.
Protect your skin with clothing. You can protect most of your skin with clothing, such as long-sleeve shirts and a wide-brimmed hat. Thick, dark-colored fabric usually works well to provide the best protection for the skin.
Use of protective creams. Use protective creams, especially in cases where sunlight is intense. Use creams even on cloudy and cloudy days because ultraviolet rays penetrate clouds and fog.
Sunscreens should be applied to unprotected areas of the skin 20-30 minutes before going outside so that the skin absorbs the cream. Apply a thick layer to face, ears, arms, legs and neck. Remember that skin treatment must be repeated every 2 hours. It is also recommended to treat the lips.
Protective creams and products are not used to keep you in the sun for a longer period of time. These products do not prevent melanoma, they only reduce the intensity of exposure to ultraviolet rays.
Wearing sunglasses. Sunglasses provide 99-100% protection to the eyes and the skin around them from exposure to ultraviolet rays.
Avoid other sources of ultraviolet radiation. The use of ultraviolet lamps is hazardous to health, as their light can damage the skin, so their use is not recommended. These lamps increase the risk of melanoma.
Protecting children from the sun. Children deserve special attention as they spend a lot of time outdoors and get sunburned quickly. Older children should be aware of the dangers of prolonged sun exposure and the possibility of melanoma. In high mountain areas and areas with intense sun exposure, the use of protective equipment should become a habit for you and your children.
Identification of altered moles (nevi) and their removal. The presence of certain types of moles (nevi) is accompanied by an increased risk of melanomas. Depending on the appearance of these moles, your doctor may recommend careful monitoring or removal if malignant degeneration is suspected. Routine removal of multiple moles as a preventive measure for melanoma is not recommended. If you have multiple moles, regular monitoring by a dermatologist is recommended, as well as monthly self-examination. If you discover an unusual mole or its change, you should immediately contact a specialist.
Genetic counseling. If more than one member of your family has had melanoma, if you have had multiple melanomas, or if you had melanoma at a young age or dysplastic nevi, you may have a gene mutation(s). In this regard, genetic counseling is necessary. In some families with a high frequency of melanomas, a mutation of the CDKN2A gene has been found.
Prevention and early detection of skin melanoma
Reducing the risk of developing melanoma:
- regular self-examination of the skin. Particular attention should be paid to moles at the beginning and end of summer. If there are any signs of their degeneration, you should consult a doctor;
- if there are a large number of moles, large pigment spots or atypical nevi, excessive solar insolation should be avoided and examined by specialists annually;
- exposure to ultraviolet radiation on the skin, both solar and artificial (solariums), should be limited;
- You should not sunbathe between 10 a.m. and 3 p.m. This is the most dangerous time, when the sun is most active and the likelihood of quickly getting burned is highest. At this time, sunscreens are also ineffective. They protect the skin from burns, but do not reduce the risk of melanoma and skin cancer;
- Do not stay in the sun without protective equipment for no more than 30 - 40 minutes. The most reliable and simplest way of protection remains our clothing, hats that protect the skin of the face, and scarves that cover the neck. In this case, preference should be given to cotton and loose-fitting clothing.
In approximately half of cases, melanoma develops from pigmented nevi. The true incidence of melanomas from nevi has not yet been established. However, as practice shows, melanoma can develop from any type of pigmented nevus. Therefore, when removing them, postoperative histological examination is mandatory.
The greatest dangers for the development of melanoma are giant pigmented nevi, atypical (dysplastic) nevi, and limited precancerous melanosis of Dubreuil.
A giant pigmented nevus can be localized on any part of the body, but most often on the limbs and torso. Sometimes satellite nevi may be observed. The neoplasm is a highly pigmented congenital spot of large size, the color of which varies from gray to black, often covered with hair, its surface may be uneven, warty with cracks. Malignancy is observed in 1.8-13% of cases.
Atypical (dysplastic) nevi
Atypical (dysplastic) nevi occur at different ages. The average size of the neoplasm usually exceeds that of ordinary acquired nevi (more than 5 mm). Atypical nevi can be single or often multiple. The shape of the neoplasm is irregular (ovoid), the surface is usually flat, the contours are not clear with a blurred edge.
An atypical nevus has uneven pigmentation (the center of the nevus is one color, the edges are another) and wide variations in color (from light gray to dark brown and pink). Atypical nevi are the most common precursors of melanoma and are clinical markers of high risk of developing melanoma.
Atypical nevus syndrome
Atypical nevus syndrome is a combination of a large number of irregularly shaped nevi, including atypical ones, and cases of familial melanoma. This syndrome requires examinations by an oncologist every 6 months throughout life.
Limited precancerous Dubrey's melanosis (melanosis maligna)
The disease begins with a small brown spot that slowly spreads around the periphery, which can reach a size of 6 cm or more. A characteristic feature is uneven coloring, the presence of areas from light brown to bluish-black.
Initially, a spot with uneven edges does not rise above the surface of the skin, is not compacted, and the skin texture is not changed. Subsequently, small papules and plaques may appear on the surface. Develops mainly in older people.
The incidence of melanoma against the background of Dubreuil's melanosis reaches 30-80% with an incubation period of 3 to 20 years.
Forecast
Every year, melanoma is diagnosed in an average of 15 people out of every hundred thousand adults, approximately 3 patients die, and with a fairly stable mortality rate in the last quarter century, men began to die more often. Gender determines a lot in the prognosis of the disease, other things being equal, but young people experience the disease with less difficulty.
The probability of death with a late relapse is many times lower than with an early relapse. Early detection of progression promises better treatment results.
It is extremely difficult to predict the course of melanoma, because even a common process is not considered absolutely fatal; this malignant disease does not often live up to expectations. Don’t guess “to be or not to be”, contact specialists if you have problems, or better yet, before they appear - we will always help.
| Read more about dermatological studies at Euroonko clinics | |
| Consultation with a dermatologist-oncologist | from 5,100 rub. |
| Skin examination using the German FotoFinder device | RUB 13,400 |
| Diagnosis of melanoma | from 5,100 rub. |
Book a consultation 24 hours a day
+7+7+78
Bibliography
1. Semiletova Yu.V., Anisimov V.V., Vagner R.I. /Treatment of patients with primary skin melanoma. Current state of the problem // Siberian Journal of Oncology. 2010. No. 4. 2. Semiletova Yu.V., Anisimov V.V., Lemekhov V.G. et al./Risk factors for relapse after radical treatment of skin melanoma//Sibir.onko.zhur.; 2012. No. 2 (50) 3. Stroyakovsky D. L., Abramov M. E., Demidov L. V. et al. /Practical recommendations for drug treatment of skin melanoma // Malignant tumors: Practical recommendations RUSSCO #3s2, 2018 (volume 4. de Vries E., Bray FI, Coebergh JW, Parkin DM /Changing epidemiology of malignant cutaneous melanoma in Europe 1953–1997: rising trends in incidence and mortality but recent stabilizations in western Europe and decreases in Scandinavia// Int J Cancer 2003; 107. 5. MacKie RM, Bray C., Vestey J., et al./Melanoma incidence and mortality in Scotland 1979– 2003 // Br J Cancer 2007;96.
/Treatment of patients with primary skin melanoma. Current state of the problem // Siberian Journal of Oncology. 2010. No. 4. 2. Semiletova Yu.V., Anisimov V.V., Lemekhov V.G. et al./Risk factors for relapse after radical treatment of skin melanoma//Sibir.onko.zhur.; 2012. No. 2 (50) 3. Stroyakovsky D. L., Abramov M. E., Demidov L. V. et al. /Practical recommendations for drug treatment of skin melanoma // Malignant tumors: Practical recommendations RUSSCO #3s2, 2018 (volume 4. de Vries E., Bray FI, Coebergh JW, Parkin DM /Changing epidemiology of malignant cutaneous melanoma in Europe 1953–1997: rising trends in incidence and mortality but recent stabilizations in western Europe and decreases in Scandinavia// Int J Cancer 2003; 107. 5. MacKie RM, Bray C., Vestey J., et al./Melanoma incidence and mortality in Scotland 1979– 2003 // Br J Cancer 2007;96.
Diagnosis of skin melanoma
Examination methods before prescribing treatment
The diagnosis of skin melanoma is established on the basis of morphological examination of the removed tumor:
- if there is ulceration on the surface of the tumor, it is possible to perform a cytological examination (imprint smears), which makes it possible to clarify the diagnosis at the preoperative stage;
- an enlarged lymph node is punctured, including under ultrasound control, to clarify the regional spread of the process (metastatic lesion of the lymph node);
- if the diagnosis of melanoma, despite the examination, is in doubt, excisional biopsy is used as the final diagnostic method, including with urgent intraoperative histological examination;
- If the diagnosis of melanoma is confirmed by the results of an excisional biopsy, radical surgery is immediately performed.
In parallel with the general clinical examination, taking into account the tendency of melanoma to early lymphogenous and hematogenous metastasis, an instrumental examination is carried out:
- X-ray examination of the chest organs;
- ultrasound examination of the abdominal organs;
- ultrasound examination of regional lymph nodes;
- if there are clinical symptoms of damage to the skeletal system, osteoscintigraphy or x-ray of skeletal bones is performed;
- If there are clinical symptoms of brain damage, an MRI or CT scan of the brain is performed.
Metastases to the lungs
Treatment of metastatic melanoma in Israel is carried out only after an accurate diagnosis of the disease has been established, including a revision of histology and immunohistochemical tests.
Israeli clinics have unique equipment that allows them to detect microscopic foci of metastasis, accurately determine the genetic form of the disease (on the basis of which certain medications are prescribed) and determine the aggressiveness of the process.
To treat metastatic melanoma in Israel, both immunotherapy and the effect of inhibitors on tumor cells in combination with biological methods are used. When prescribing a treatment program, the form of melanoma, the prevalence of the tumor process, as well as the general condition of the patient’s body are taken into account.
Modern medicine, even in the most advanced cases of metastatic melanoma, is able to stop the development of the tumor process, significantly reduce tumor intoxication, relieve pain, prolong the patient’s life and improve its quality.
Below are the types of treatments for metastatic melanoma.
Stages of skin melanoma
Establishment of the stage of melanoma is carried out on the basis of data from a morphological study of the remote primary tumor focus, regional lymph nodes (if they are metastatic) and data from instrumental examination.
- stage 0 melanoma in situ (I level of invasion according to Clark) (atypical melanocytic hyperplasia, severe melanocytic dysplasia, non-invasive malignant lesion);
- Stage I melanoma less than 1 mm thick and non-ulcerated melanoma up to 2 mm thick;
- Stage II melanoma with a thickness of more than 2 mm and ulcerated melanoma with a thickness of up to 2 mm.
Primary metastatic melanoma
- Stage III - all melanomas with the presence of metastases in regional lymph nodes;
- Stage IV - all melanomas with the presence of metastases in distant organs and tissues.
Melanoma with metastases: prognosis
Why is it important to know the location of metastases? Large-scale studies have shown that survival rates for advanced melanoma are directly related to the location of metastases, which determines the further prognosis of the disease:
| Localization of metastases | Survival periods | ||
| 1 year | 2 years | 5 years | |
| Skin, soft tissue and/or lymph nodes | 62% | 43% | 28% |
| Lungs | 53% | 31% | 15% |
| Visceral organs | 33% | 18% | 9% |
Treatment of skin melanoma
Treatment of melanoma without metastases and melanoma with metastases only in the lymph nodes is surgical. For metastatic forms of the disease, surgical methods, chemotherapy, immunotherapy, general hyperthermia, and photodynamic therapy are used. Treatment of melanoma should be carried out exclusively in a specialized oncological institution.
Surgical treatment of skin melanoma
Surgical excision of melanoma and metastases in regional lymph nodes is currently the mainstay of treatment.
Surgery involves excision of the tumor en bloc with the surrounding skin, subcutaneous tissue and underlying fascia.
A postoperative skin defect is eliminated using one of the following types of plastic surgery:
- free skin flap (if the tumor is localized on the lower limb, a free skin flap is prepared on the thigh of the opposite limb or in other donor areas);
- local tissues;
- combined skin grafting;
- plastic surgery with displaced island flaps or microsurgical tissue autotransplantation.
Removal of lymph nodes is carried out only if their metastatic lesion is confirmed. Standard surgical interventions on the lymphatic system are:
- subclavian-axillary-subscapular;
- ilioinguinal-femoral;
- classic radical cervical (Crile operation);
- modified radical cervical lymph node dissection type III;
- ilioinguinal-femoral lymph node dissection.
Radiation treatment of skin melanoma
Radiation therapy for melanoma can be used if surgical removal of metastases is impossible, as well as after removal of large metastases in order to prevent relapse.
Chemotherapy and immunotherapy for skin melanoma
Unfortunately, there are currently no drugs in the world that could cure melanoma metastases. Prophylactic chemotherapy is not used after surgical removal of melanoma.
The most effective chemotherapy drug for treating melanoma is dacarbazine (DTIC). When metastases develop in the brain, the drug temozolamide and nitrosmethylurea derivatives (NMM), which have the ability to penetrate the blood-brain barrier, are used. Other drugs, as well as their combinations (cisplatin, paclitaxel, vincristine, bleomycin), can be used in the treatment of melanoma.
With a generally satisfactory condition and an LDH level not exceeding 1.5 of the upper limit of normal, chemoimmunotherapy, including the administration of high doses of interleukin-2, is possible.
Other methods are not methods that can cure melanoma. However, their use in some cases can slow down its development, and sometimes reduce the size and number of tumor lesions.
General hyperthermia (GHT)
General hyperthermia (GHT) is used in the treatment of melanoma metastases in internal organs, soft tissues and skin (with a generally satisfactory condition). OHT is not used for metastases localized to the head and neck, as well as in the brain.
OGT consists of heating the human body with an electromagnetic field (under anesthesia) with the introduction of antitumor drugs. In some cases, against the background of OHT, the tumor decreases in size or stops growing even with the use of chemotherapy, to which it was previously insensitive.
Photodynamic therapy (PDT) is used to treat small intradermal metastases of melanoma. It does not cure the disease, but can have a pronounced local antitumor effect.
Publications in the media
Melanoma accounts for 1% of cancers. Most melanomas develop de novo, but about 15% arise from existing pigmented (melanoma-prone) nevi. These include: nevus of Ito, nevus of Ota, blue nevus, borderline nevus, Dubreuil's melanosis. Frequency . Incidence: 4.5 per 100,000 population in 2001. The incidence of melanoma has been growing rapidly over the past few decades and accounts for 2.5 10% of all newly diagnosed skin tumors. Melanoma most often affects people aged 30–50 years. Risk factors : insolation and hereditary burden. Genetic aspects . Burden: • 155601, CDKN2A, MTS1, P16, MLM, CMM2, 600160, 9p21; • CDK4, 123829, 12q14; • D2S448, MG50, 600134, 2p25.3; • Malignant skin melanoma, CMM, MLM, DNS, 155600, 1p36.
Clinical picture . Melanoma is a tumor consisting of cells that produce the pigment melanin, so in most cases it is dark in color • In 20–30% of cases, the localization of melanoma is the head and neck, but it can occur on any part of the skin, including the palm and sole, nail bed . Frequent localization of the tumor in men is the back, chest and upper limbs, in women - chest, lower limbs (places of frequent trauma - the area of shoe straps, bra straps). Occasionally, melanoma occurs on the mucous membranes of the oral cavity, nasopharynx, vagina, anal canal, esophagus, bronchi and biliary tract. In approximately 1/3 of patients with a disseminated process, it is not possible to determine the primary focus, despite a thorough clinical examination • Melanoma can be suspected if the color, size or shape of the nevus changes • Variegated (red, pink, blue) coloring of a brown pigmented nevus or discoloration, ulceration - highly suspicious for the development of melanoma • Multiple primary tumors can arise synchronously or metachronously, so it can be difficult to distinguish the primary tumor from epidermotropic metastases • Malignant melanoma metastasizes frequently and widely. The usual type of metastasis is the appearance of intradermal and subcutaneous “satellites” along the lymphatic vessels, multiple damage to distant organs and tissues (especially the liver, bones, lungs and brain).
Classification (criteria - histological variant and tumor extent) • Superficial melanoma (70% of all melanomas). Most often located on the back and legs. The average age of patients is 50 years. A tumor with uneven edges, color varies. Atypical cells are localized in the upper layers of the dermis, spreading in the lateral direction. The prognosis is usually favorable • Nodular melanoma (15%). The tumor is blue in color, without a specific localization, and occurs in old age. Tumor cells spread vertically with rapid invasion of the dermis. Prognosis is poor • Acrolentigoid and mucinous melanoma (10%). A tumor with uneven edges, black in color, may be without pigment. It grows slowly in a radial direction, usually in the upper layers of the dermis (on the palms, soles). The prognosis depends on the degree of infiltrating tumor growth • Lentigo maligna (melanotic freckles) is the rarest form. Develops at 60–70 years of age. Nodules in the form of spots from yellow-brown to almost black, with a diameter of 1.5–3 mm, form in smooth freckles. Tumor growth is slow, in a radial direction in the upper layers of the dermis. The prognosis is favorable.
Stages • Tumor size as a criterion for prognosis, unlike all other tumors, is unacceptable for melanoma. The thickness of the primary tumor matters. Based on this, determining the T category is possible only histologically (pT), i.e. excision of the tumor is necessary, and scrapings and puncture biopsies cannot be used (if melanoma is suspected) • Histological staging is based on microscopic measurement of tumor thickness using two systems: •• Absolute tumor thickness (Breslow) •• Depth of invasion (in relation to structures skin) according to Clark • For different values according to different systems, use the largest T category in any of them.
• Levels of melanoma invasion according to Clark •• I – tumor growth within the epidermis •• II – tumor penetrates the papillary dermis •• III – tumor within the papillary dermis, does not penetrate the reticular layer of the dermis •• IV – tumor penetrates the reticular layer layer of the dermis •• V - invasion of subcutaneous tissue • Thickness of the primary lesion according to Breslow - a method for determining the degree of malignancy of a tumor: measuring the depth of invasion in mm •• Low risk of metastasis - tumors of levels I, II, III according to Clark and depth of invasion less than 0.76 mm •• High risk of metastasis - tumors of levels IV, V according to Clark and invasion depth of more than 1.5 mm.
• TNM classification (used only for skin melanoma, see also Tumor, stages) •• pTis - melanoma in situ - atypical melanocyte hyperplasia, severe melanocyte dysplasia (I level of invasion according to Clark) •• pT1 - tumor up to 0.75 mm thick , extending to the papillary layer (II level of invasion according to Clark) •• pT2 - tumor with a thickness of more than 0.75 mm, but less than 1.5 mm and/or infiltrating the papillary layer (III level of invasion according to Clark) •• pT3 - tumor thicker than 1.5 mm, but less than 4 mm and/or infiltrates the reticular layer (IV level of invasion according to Clark) •• T3a - tumor up to 3.0 mm thick •• T3b - tumor up to 4.0 mm thick •• T4 - tumor with the presence of the following signs: the thickness of the tumor is more than 4 mm or the tumor infiltrates the subcutaneous tissue (V level of invasion according to Clark) - T4a •• there are “satellites” within 2 cm of the primary tumor - T4b •• N1 - metastases up to 3 cm in the greatest dimension in any of the regional lymph nodes •• N2 - metastases more than 3 cm in greatest dimension in any of the regional lymph nodes and/or transient metastases.
• Grouping by stage • Stage 0: TisN0M0 • Stage I: T1–2N0M0 • Stage II: T3N0M0 • Stage III •• T1–4N1–2M0 •• T4N0M0 • Stage IV: T1–4N0–2M1.
TREATMENT • The leading method of treatment is surgical. Once the diagnosis is established, a wide excision of tissue is performed, departing from the edge of the tumor by 3–3.5 cm (at least 1.5 cm on the facial skin). It is possible to perform laser or cryodestruction •• For melanomas in situ, excision of healthy skin at a distance of 0.5–1.0 cm from the edge of the tumor is acceptable •• For tumors less than 0.75 mm in thickness, it is sufficient to excise 1–2 cm of healthy skin along the periphery of the tumor •• For tumors greater than 0.75 mm in thickness, excision of 3 cm of healthy skin is indicated.
• Lymphadenectomy •• Lymphadenectomy is performed only if there are clinical signs of metastatic lesions of regional lymph nodes •• Prophylactic and/or diagnostic removal of clinically unaffected lymph nodes is indicated only in the following cases ••• The location of the tumor above a group of lymph nodes at the V level of invasion ••• Depth invasion of more than 0.75 mm for tumors of levels III–V •• Recently, the “sentinel node” technique has become widely used to clarify the indications for lymphadenectomy.
• When the process is generalized, chemotherapy is administered (dacarbazine, platinum drugs). Endolymphatic administration of drugs into the corresponding limb is often used (for melanoma of the skin of the extremities). Regional hyperthermic perfusion • Immunotherapy is effective in the treatment of cutaneous metastases • Radiation therapy is a palliative treatment for brain and bone metastases.
• Chemotherapy is rarely used for adjuvant purposes, mainly in cases of poor prognosis; immunotherapy is often preferred.
Forecast. Melanoma is the least predictable type of malignant tumors • “Thick” (>1.5 mm) tumors and/or lymph node involvement are a factor predicting the occurrence of distant metastases. However, some “thin” (<0.76 mm) melanomas metastasize primarily to the visceral membranes. Sometimes metastases remain clinically occult for a significant period (up to 30 years) after diagnosis • With a localized tumor, the 5-year survival rate reaches 80–90% • With damage to regional lymph nodes, the rate decreases to 30–50% • Patients with distant or visceral metastases die within up to 12 months, but at the same time, spontaneous regression of the process is also possible.
ICD-10 • C43 Malignant melanoma of the skin • D03 Melanoma in situ
Observation and examination after treatment
After radical surgery, local tumor recurrences are extremely rare. However, given that melanoma metastases can develop many years after removal of the primary tumor, lifelong monitoring by an oncologist is necessary.
Therefore, patients who have completed treatment must undergo an examination, which includes:
- examination of all skin;
- palpation of regional lymph nodes;
- X-ray examination of the chest organs;
- Ultrasound of the abdominal organs;
- general and biochemical blood test;
- determination of the level of lactate dehydrogenase (LDH) in blood serum (for melanoma with metastases).
In some cases, it is necessary to use other examination methods (MRI of the brain, CT of the abdominal and thoracic cavities, osteoscintigraphy, etc.).
During the first two years, control examinations are carried out every 3-6 months. During the third year every 4-12 months, then annually.