Myths about human papillomavirus (HPV)
The most common myths about human papillomavirus.
Myth 1 The HPV virus is common in African countries where the standard of living is low.
Human papillomavirus does not choose a continent or country.
It can infect any sexually active person in any part of the world. Today it is one of the most common pathogens transmitted through sexual contact or skin and mucous membranes. Even four out of five sexually active people become infected with this virus at least once in their lives. Myth 2 Only women are infected with HPV.
Any sexually active person can be infected with the HPV virus, even if they have only one partner.
Men face the same or higher risk of acquiring HPV and can become carriers and spreaders of the virus. During their lifetime, 4 out of 5 sexually active people will become infected with HPV at some point in their lives. Although the body of most infected people clears the virus on its own, the possibility of reinfection with this or another virus remains for life. If the human body does not remove the virus and it remains in the cells, the risk of developing the cervix, vagina, vulva, anus, penis, mouth, pharynx, larynx, and root of the tongue increases. Long-term low-risk HPV infection causes warts on these organs. Myth 3 Among my friends, I am the only one who has been diagnosed with this virus, so I don't think it is that common.
The vast majority are unaware of the virus.
It is not surprising that they may simply not know about their disease. Research shows that one in four women of reproductive age is infected with HPV, and even four out of five sexually active people will become infected with HPV during their lifetime. This virus can disappear from the body on its own, so a woman is sometimes unaware of a possible HPV infection if she has not been tested at this stage of life, especially since a temporary infection does not cause any symptoms of the disease. Men are generally not tested for HPV infection, although they can carry and spread the virus. Myth 4 HPV is only transmitted through casual sex or multiple sexual encounters.
It is true that the transmission of STIs is higher when there are multiple sexual partners, but the belief that infection only affects those with many casual relationships is inherently false. In fact, HPV also threatens those who are involved with one long-term partner. Even if your sexual partner is your first and only sexual partner, you can still become infected with HPV if he or she had contact with someone infected with HPV in the past and became a carrier. Myth 5
If I was diagnosed with HPV, then my partner was unfaithful to me.
A diagnosis of HPV does not mean your partner is unfaithful.
This myth causes anger, confusion, anxiety and fear. The virus lurks in a latent, asymptomatic state in the patient's body for weeks, months and years. Then they talk about a chronic infection. Obvious symptoms sometimes take time (months, years). If you are confirmed to have the virus with one regular partner, this means that your friend may have had sex with someone who was infected with HPV at some point in their life before you. Myth 6 All types of HPV cause cancer.
Not true.
HPVs are classified into high- and low-risk types (genotypes). Cancer is caused by high-risk HPV genotypes. The International Agency for Research on Cancer has confirmed that papillomavirus type 14 has a high risk of developing cancer. The oncogenicity of other viruses is being studied. The highest oncogenic risk is for types 16 and 18 of HPV. Low levels of HPV, for example 6 and 11, do not cause cancer. Myth 7 Genital warts will immediately become cancer.
Warts localized in the genital area are benign in almost all cases.
There’s a reason why these types of HPV are called “low-risk.” Low-risk HPV types may cause temporary changes in cervical cytology; however, these changes are not cancerous. If you find cytological changes, you should make sure that there are no high-risk human papillomaviruses, which are the biggest factor in the development of cervical cancer. Myth 8 If I get HPV, I will feel some signs of infection.
Most people infected with HPV do not feel any symptoms. A temporary infection is unlikely to cause warts or cancer. In nine out of ten people who are infected, the infection clears up within two years. Although they do not feel any symptoms, they can infect their sexual partners. Myth 9 An "abnormal" cytological change in the cervix is cancer.
Cytological changes in the cervix are caused not only by HPV infections.
These cellular changes can occur due to microdamage, bacterial infection, a low-risk HPV type, or even inadequate tissue collection and evaluation studies. For these reasons, repeating the test several months later will usually not detect cytological changes. The doctor will most likely recommend a colposcopy, take a tissue biopsy, may suggest assessing the type of HPV infection for high risk, and only then will be able to say Are these changes truly precancerous and should they be treated at this time, or can they be observed until they may go away on their own? In all cases, women should take responsibility for their own health and be checked at intervals recommended by health care professionals. Myth 10 If I was diagnosed with HPV, the disease will recur again and again.
In some cases, if the HPV infection persists in the body for a long time and the person's immune system is weak, warts or precancerous genital changes may appear several times during a given period of life.
The good news is that most people do not have an infection after two years. The bad news is that one in five sexually active people can become infected with the same HPV virus every year. The human immune system is weakened by chronic diseases, certain medications, injury, stress, anemia, various infections and other factors. We cannot determine how long the HPV infection will remain in the body. Each individual case is individual. Myth 11 For older women, cytological examination of the cervix is not required.
Cancerous changes take time.
This may take a year, ten years or more. If HPV infection occurs in old age, the virus is released from the body more slowly, and the longer it remains in the human body, the higher the risk of precancerous changes and cancer. At older ages, latent infection may reactivate. The decision not to get tested can be fatal: one in four women diagnosed with cervical cancer are 65 years of age or older. More than 40% of deaths from cervical cancer also occur in women of this age. Myth 12 If I cure my warts, I will no longer pose a threat to my partner.
Removing warts does not mean the HPV infection is completely gone. Visible warts are usually treated with medications or surgically removed.
The risk of wart transmission after HPV treatment is likely to be reduced by destroying the cells in which the virus was found. However, the virus can also remain in surrounding cells that do not show any changes visible to the eye, so transmission of infection is possible. Myth 13 I don't have to worry about HPV because my partner doesn't have genital warts.
The absence of warts on the genitals does not necessarily mean that your partner does not have HPV.
Often the HPV virus is physically invisible, so you cannot tell by sight whether your partner has the infection. Myth 14 If a woman is diagnosed with cervical lesions, her partner should be tested for HPV infection.
It is now generally accepted that if female cervical lesions are detected, there is no need to identify sexual transmission of HPV infection. The partner likely had an HPV infection for some time in his life, although no signs of infection were diagnosed or vice versa. Of course, if a woman is diagnosed with genital warts, her partner is also advised to get tested because most people do not even notice very small warts in their genital areas.
Myth 15 I have no risk of contracting HPV because I use condoms.
When using condoms, the likelihood of contracting HPV is reduced, but using a condom can sometimes only help “get rid of existing HPV infections faster.” Proper and timely use of condoms can prevent diseases that are transmitted through body fluids (gonorrhea, trichomoniasis, etc.), in while human papillomavirus, herpes infection is spread by contact of skin and mucous membranes.
The condom does not cover the entire perineal membrane, so the vulva, anal, perianal areas, base of the penis, and scrotum remain open to contact and transmission of HPV. Myth 16 I don’t have sex, so I can’t get HPV.
HPV viruses can be transmitted during any sexual relationship, as well as through direct contact with skin or mucous membranes.
HPV infection can be transmitted to a newborn from the mother. Myth 17 HPV can be cured.
Cancer caused by warts or precancerous lesions can be cured, but there is no vaccine or drug for all types of the virus. Each body has the ability to destroy this virus on its own.
The spontaneous disappearance of the virus depends on the strength of the body's immune system, the aggressiveness and quantity of the virus. It is also true that a person's immune system can suppress the aggressiveness of the virus so that it does not compromise health until it disappears completely. Myth 18 HPV infection can cause infertility.
HPV infection does not affect women's fertility. If a woman is pregnant and infected with HPV, she may develop warts or precancerous lesions, but regular checkups help ensure timely treatment. However, women can pass HPV infection to their newborns during childbirth.
Treatment
There is no way to recover from the virus. But if the body has a strong immune system, then within 6-12 months it gets rid of it on its own. Therefore, if a woman is found to have a positive result when taking a PCR test for HPV, then she is only observed first.
A year later, the analysis is retaken. If it is negative, then there is no danger. If the result is positive, you should be examined by a gynecologist every six months so as not to miss the appearance of changes in the cervix or the formation of condylomas. Getting rid of them is done only surgically; there is no other treatment: laser, electric cauterization, low-cryogenic method and radio wave knife.
The medical specialist performs removal of genital warts using the Surgitron device, as well as conization of the cervix. Here you can submit a smear for oncocytology, which will be ready within 3-5 days. As well as PCR analysis for HPV detection.
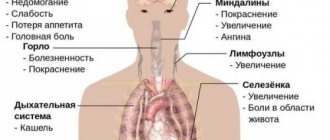
High-risk HPV: no symptoms
Unfortunately, most people who have the high-oncogenic risk type of HPV do not show symptoms or signs until it has already caused serious health problems. This is why regular checkups are so important. In many cases, examination can identify atypical cells at an early stage.
Penile cancer - may present with symptoms such as changes in the color or thickness of the skin of the penis, or the development of a painful ulcer on the penis.
Anal cancer may cause anal bleeding, pain, itching or discharge, or changes in bowel habits.
Vulvar cancer - may present with symptoms such as changes in skin color/thickness in the vulvar area. There may be chronic pain and itching.
Throat cancer can cause a sore throat, ear pain that doesn't go away, a persistent cough, pain or trouble swallowing or breathing, and weight loss.
General characteristics of condylomas
Condylomas can be pointed or flat. Typically, condylomas are found only on the skin and mucous membranes with transitional epithelium. Condylomas are not found in the internal organs. Their favorite places to localize are the perineum, genitals, anus and oral cavity. Condylomas usually occur in groups. In the presence of reduced immunity, skin moisture and poor hygiene, condylomas can merge with each other, forming tumor-like growths from condylomatous masses. In appearance, condylomas resemble cauliflower due to the granularity of the surface. Fresh condylomas have a soft pink color and are easily vulnerable, while older formations often show signs of keratinization and are rough to the touch. The disease is asymptomatic from 4 weeks to 3 months. In the absence of a regular sexual partner, the carrier of the virus may not remember when he became ill.
Papilloma virus and intimate life
Many patients ask the same question: is it possible to have sex with HPV?
Experts who deal with this type of disease answer: yes, you can have sex with HPV.
Whether to engage in sex or avoid sex altogether if you have HPV is a person’s decision for himself.
It must be taken into account that with an active intimate life, the problem of HPV is already more serious.
It is not possible to cure HPV; there are only some ways to eliminate the infection and send it into a dormant state.
But there are times of relapse, repeated outbreaks of papillomatosis, and the patient turns to the doctor again and again.
How does the vaccine work?
“We must understand that the vaccine does not contain the virus itself, only its shell. But the body perceives it as a foreign agent and develops immunity to this virus.
However, the vaccine does not cure. If a woman is already infected with a certain type of HPV, it means that the p53 protein has already been destroyed, and if she is re-infected, the cells will still change. But you can get a vaccine against other types of HPV.
For example, a woman is infected with type 16 virus. She must regularly undergo screening control, but no one forbids her to get a vaccine against types 6, 11, 16 and 18. She will gain immunity to all types except type 16.
Signs
If HPV does not manifest itself in formations (warts, papillomas and condylomas), then without special tests the patient usually does not know that he is infected. In this case, the symptoms of the human papillomavirus are precisely the neoplasms - they can be accompanied by itching and discomfort.
If formations appear in the genital area, they can also manifest as painful and unpleasant sensations during or after sexual intercourse.
Are you experiencing symptoms of human papillomavirus?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call