Everyone experiences the onset of puberty differently, it can start at 8 years old, 15 years old and continue until 18 years old and even 19 years old. Therefore, it is extremely important for parents to pay attention to the physical and psychological state of their child. It is important that his life includes physical activity, a balanced diet, enough vitamins and minerals, and no stress.
The disease code according to ICD 10 in children is No. 62. Juvenile gynecomastia can be either unilateral or bilateral - in any case, it is necessary to determine the cause and prescribe treatment.
Description of the disease
Atheroma is one of the relatively harmless tumors due to the fact that it does not transform into a malignant neoplasm.
However, there is a risk of significant increase in size, so medical attention is required in all cases. Teenage children are more likely to experience this problem. Boys and girls get sick about the same. The main reason why parents first turn to a surgeon is the presence of a visually noticeable tumor.
The atheroma itself is a small capsule filled with pasty contents. It is sebum, which, due to blockage of one or more glands, did not come out, but remained in the subcutaneous tissue.
Symptoms of atheroma in children
In 80-85% of cases, apart from the visual defect, children do not present any other complaints. Uncomplicated atheroma is characterized by:
- painlessness;
- mobility;
- elasticity upon palpation.
The skin over the surface of the tumor is smooth and does not fold. The clinical picture may change when the contents of the atheroma become inflamed against the background of the addition of bacterial flora. In this case, patients may note:
- pain when pressed;
- redness and increase in size of the tumor itself;
- local increase in body temperature.
If the above symptoms occur, you should immediately seek help.
This situation threatens the penetration of infection into nearby tissues and blood with the spread of microorganisms to distant areas of the body and can cause a deterioration in the general condition of the child. Atheromas occur in areas of the skin that are rich in sebaceous glands. Therefore, they especially often have the following localization:
- scalp;
- face and neck area;
- shoulder girdle, armpit area;
- back.
Neoplasms occur less frequently in the groin area and scrotum (in boys). In these areas they have the appearance of a skin growth and require differential diagnosis with other skin tumors.
Main reasons
Let's look at the main reasons that lead to breast enlargement in boys:
- the beginning of the production of male sex hormones, especially testosterone. In a young body, all the mechanisms of work have not yet been adjusted, especially the work of the entire reproductive system. When testosterone is formed, it goes through a stage in which it becomes very similar to estrogen, and estrogen is a female sex hormone, which also affects the growth of mammary glands in girls. So, if the hormonal system is normal, then testosterone goes through all stages and works it’s normal, if a malfunction occurs, then there is little testosterone and a lot of estrogen, as a result - breast growth in a teenager;
- excess weight in a child - contributes to the development of false teenage gynecomastia, can be both a complicating factor for gynecomastia and provoke its development due to a detrimental effect on the hormonal system;
- the presence of pathologies in which the production of estrogen significantly increases. Such diseases include chromosomal abnormalities, liver dysfunction, neoplasms in the genital organs;
- extremely rarely, gynecomastia in boys is caused by injuries and damage to the chest area;
- various genetic anomalies - Reifenstein syndrome, Kallmann syndrome, XX-men, etc.;
- taking certain medications. There is a high probability of enlargement of the mammary glands in adolescents when taking anabolic steroids and other drugs that can make adjustments to hormonal levels.
All causes can be simultaneously or interconnected, so it is necessary to conduct a thorough diagnosis, since the success of treatment will depend on the identified cause.
Causes of atheroma in children
Atheromas in children occur due to a violation of the secretion of sebum by the corresponding glands.
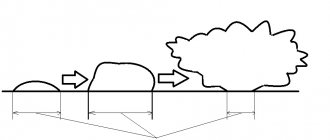
When the excretory duct is blocked, the secretion of the gland has nowhere to go. It is secreted into the subcutaneous space, where a dense capsule is formed around it. Common causes of atheroma development in children are as follows:
- Using children's cosmetics (creams, ointments, moisturizing masks) in excessive quantities. Sometimes parents, in an effort to protect their child’s skin from harmful external factors, use cosmetic products uncontrollably. This leads to dysfunction of the sebaceous glands with blockage of their excretory ducts.
- Hormonal changes in the child's body. Infants and teenage children are traditionally at risk. It is during these periods that changes in the concentration of sex hormones occur. Against this background, acne appears, the function of the sebaceous glands is disrupted, and conditions are created for their blockage.
- Seborrhea. This is a dermatological disease that leads to dysfunction of the sebaceous glands in a certain area of the skin.
- Genetic predisposition or congenital structural features of the skin. Atheromas most often occur in children after 3 years of age. If neoplasms are detected in children immediately after birth, the doctor may assume the presence of problems with the sebaceous glands that developed in utero.
In addition, factors that increase the risk of developing atheromas are poor personal hygiene, metabolic disorders (obesity, diabetes) and frequent mechanical damage to the skin.
Should I worry if my pacifier has become indispensable?
First off: what's the difference?
It's actually simple. A nipple is a product that is shaped like a female nipple and is placed on a bottle. That is, there is a hole in the nipple, and it is intended for feeding the baby. A pacifier is also a product that resembles a nipple, but there is no hole in it, and you cannot feed your baby through it. A child can only suck a pacifier and a pacifier, nothing else. Therefore, I will consider them together.
Now about the myths. There are quite a lot of them on the Internet and I will explain the most common ones about nipples (pacifiers).
The pacifier “spoils” the bite.
True, with one “but”.
A pacifier is one of the reasons for the formation of primary malocclusion pathologies in children if:
- the child is over 1 year old (all primary incisors have erupted, and by 3 years all primary teeth have erupted)
- use of the pacifier is unlimited (24 hours a day)
- with prolonged use of a pacifier, almost 80% of children develop an abnormal primary bite (the primary teeth of the upper jaw move forward)
- weaning from her was quick
For example, if not properly weaned from a pacifier, a child may start thumb sucking. And this is already a bad habit.
According to one study, in children who already have primary malocclusion pathology, with proper and timely weaning from the pacifier, the dental system can recover on its own (65-83%). In addition, the presence of such a bite of primary teeth does not mean that the permanent bite is not formed correctly.
A small conclusion: if you use the pacifier correctly, following the recommendations of doctors, indications and contraindications, you can avoid harmful consequences.
The pacifier calms the baby.
Of course it's true.
The pacifier helps satisfy the sucking reflex, the baby calms down and falls asleep, and sleeps more peacefully at night with it. And mommy can absolutely use this. Of course, you can use it less often during the day.
The pacifier disrupts breastfeeding, problems arise, and a pacifier should not be used at all during breastfeeding.
True in some situations.
Sucking a mother's breast is a serious job for a child: you need to latch onto the breast correctly (the pacifier has a smaller latching area), actively suck on the breast to get enough milk (it is easier to suck on the pacifier, since the hole/s in it are larger and the milk flows faster).
Indeed, when there is not enough milk, the baby is supplemented with formula, then you need to choose the right pacifier (and continue to apply it to the breast in order to normalize lactation), since the child will not want to strain and will suck the breast sluggishly, will receive less milk, and therefore will worry more often. The baby may also bite and cracks may appear on the nipples. In this case, it is recommended not to give a pacifier to a healthy child unless indicated until breastfeeding is established (this is up to 1 month).
The pacifier can be used, but according to indications and for a limited time. Therefore, in the maternity hospital, the mother should consult with a doctor: is a pacifier necessary, how to maintain lactation, how correctly the child should latch onto the breast, what feeding technique and care for the mammary glands.
The risk of developing acute otitis media increases when using pacifiers.
This opinion is based on one study conducted in Finland with children aged 7-18 months, which found that the risk of developing acute otitis media (middle ear infection) was 29% lower in children who did not suck a pacifier. According to some experts, this depends on changes in pressure in the ears and leads to the accumulation of fluid inside the middle ear, the infection of which leads to the development of the disease.
I have a counter question: how long should a child suck a pacifier per day for a pressure shift to occur? To this I can only say one thing: you need to use the pacifier correctly.
A pacifier in the mouth is a source of infection.
Is it true.
It's a matter of hygiene:
- wash the pacifier once a day with baby soap or a special care product
- be sure to sterilize by boiling or in a bottle sterilizer before first use and in subsequent use
- use a container to store it
- If the pacifier falls on the floor, do not lick it! Rinse under running water or rinse with boiling water
- monitor the condition of the pacifier surface (presence of damage). If there is even one small scratch, change the pacifier. Uneven surfaces serve as a breeding ground for germs
A pacifier “slows down” a child’s development.
The sucking reflex is an important stage in the development of a child and, accordingly, it is temporary. In children under one year of age (after the reflex physiologically fades away), problems may arise if the sucking reflex is dissatisfied. But every mother should understand that the breast is the best option for the child, so a pacifier is a backup option.
Also, babies grow up to be more sociable and sociable (unless prolonged pacifier sucking has led to malocclusion and speech impairment).
It is difficult to wean a child off a pacifier, as it is addictive.
Is it true.
A child's sucking reflex is pronounced from birth and only by the age of 3 it fades away completely. At this time, it is important to gradually and with minimal stress for the child wean him off the pacifier, as this can then become a habit.
Some doctors believe that it is easiest to wean a child at the age of 1-1.5 years and does not need to be delayed until 3-4 years. The following is a list of when it is necessary to wean a child off a pacifier:
- child's age 3 years
- the child sucks a pacifier for a long time during the day with breaks for food
- the child does not want to communicate with peers and play interactive games
- The doctor discovered a speech delay in the child
As for the weaning process itself, there are also several rules:
- you need to start during a period of complete health, and in the absence of other stressful situations (kindergarten, potty training, sleeping separately, moving, etc.)
- There is no need to smear the pacifier with something tasteless, spicy or sour - the child can get this product into his eyes and nose, which can lead to an allergic reaction and other undesirable consequences
- Gradually cutting off the rubber part of the pacifier is also not an option, since the child may bite off a piece of it
What should you do then? There are many different methods on the Internet, but they are all divided into quick and gradual methods.
The quick method is tougher, but also the most reliable: at one point the mother simply hides it and doesn’t show it again, doesn’t remind her of the pacifier. This method is difficult, because not only the child sheds tears and throws hysterics, but the parents also suffer while looking at it. Also, parents need to stand firmly on their own and not make concessions to the child.
The gradual method is more loyal and calm. The point is to distract the child as often as possible, keep him busy with activities and games without the presence of a pacifier nearby, leading to the point that the child completely refuses or forgets about it.
When a child needs a pacifier only before falling asleep, you need to choose another way to put the child to sleep: read fairy tales, conduct a dialogue with the child.
Another method is to give it to another small child (baby). Not all, but many children are ready to part with their pacifier for the benefit of another child.
A child's love for a pacifier can develop into bad habits.
Smoking. Some psychologists argue that smoking is a consequence of an unsatisfied sucking reflex. That is, it’s the other way around - insufficient use of a pacifier led to smoking. Or another bad habit - biting your nails.
The habit of biting nails occurs in people who do not tolerate stress, tension and anxiety well. This is their way to calm down and it has nothing to do with the pacifier.
Be healthy!
Sincerely, Oksana Olegovna.
Diagnosis of atheroma in children
It is relatively easy to identify atheroma.
Even at the stage of the initial conversation with the patient or his parents, the surgeon assesses the general well-being of the child, collects anamnesis and analyzes complaints. When examining a neoplasm, the doctor pays attention to its size, location, pain, and the presence of redness. Before surgery, the surgeon prescribes a number of tests to comprehensively assess the child’s condition:
- general and biochemical blood test;
- general urine analysis;
- blood test for infections (HIV, syphilis, viral hepatitis B, C);
- ECG, fluorography.
The child is also examined by an anesthesiologist and pediatrician before the operation. A mandatory diagnostic method is histological examination of tumor tissue after its removal. At this stage, it is possible to determine whether it was an atheroma or a lipoma (a tumor similar in appearance).
Treatment of atheroma in children
The optimal method of treating atheroma in children is its surgical removal.
However, the age of the patient decides a lot here. Thus, most pediatric surgeons, in the absence of severe clinical symptoms, recommend a wait-and-see approach. Sometimes the swelling may resolve on its own. This is especially true for newborns and infants. In such cases, the development of the neoplasm is observed until the age of three, and if it persists, only then is it removed. Surgical intervention can be carried out traditionally using a scalpel or minimally invasively using a laser. In the first case, the surgeon excises the tumor with a capsule, which eliminates the risk of relapse. After this, cosmetic stitches are applied to the tissue to achieve the best aesthetic result.
Laser removal in children is used for small tumors. Using this technique, it is possible to avoid incisions and the formation of postoperative scars. In both cases, a comprehensive examination of the child is first carried out with the selection of the optimal treatment option.
In the postoperative period, the child may be prescribed the following groups of medications:
- painkillers;
- anti-inflammatory;
- antibacterial.
Drug therapy is aimed at eliminating discomfort and preventing infection of the postoperative wound.
Treatment methods for pubertal gynecomastia
After undergoing diagnostic tests and confirming the diagnosis, the endocrinologist will prescribe treatment based on the data obtained.
In most cases, serious treatment of the patient, especially surgery, is not required and when the hormonal system is stabilized, all indicators return to normal. But, if enlargement of the mammary glands in boys continues for a long period of time, then drug treatment or surgery is necessary.
Depending on the root cause of the problem, medications are prescribed. Most often, a teenager must take pills containing male sex hormones, or medications that suppress the secretion of estrogen.
For normal growth and development of the body during puberty, a child needs a sufficient amount of vitamins and minerals. They can be obtained either from food or in the form of special dietary supplements.
During the treatment of teenage gynecomastia, it is mandatory to take vitamin-mineral complexes, or a specialist may prescribe the intake of some individual elements that are in short supply in the patient’s body.
Which doctor should I contact?
I, Romanov Georgy Nikitich, endocrinologist, candidate of medical sciences. For more than two decades I have been helping people with various diseases. I gained my experience not only in our country, but also abroad, both in Russia and in some Western countries. I know modern methods of treating and diagnosing patients with endocrine diseases. For 3 years of work, I had more than one patient with pubertal gynecomastia, which we successfully treated.
Today I work in a clinic and also provide paid online consultations. To get an appointment with me, you need to make an appointment in one of the proposed messengers: Viber, Telegram, Instagram, WhatsApp, Skype, Vkontakte.
I will be glad to see you among my patients.
Questions
- Which doctor treats atheroma in children?
A pediatric surgeon is involved in identifying and treating atheroma in children. - Is it possible to cure atheroma without surgery?
Sometimes in the early stages of the disease the surgeon chooses a wait-and-see approach. In 20-35% of cases, atheroma can resolve on its own. However, if the capsule is formed and the tumor is large, it will not be possible to do without surgical intervention. - How dangerous is atheroma in childhood?
Atheroma is a relatively safe tumor. It does not become malignant, rarely becomes complicated and is not accompanied by the development of permanent defects. However, this does not eliminate the need to consult a pediatric surgeon. Only a doctor can establish the correct diagnosis and select treatment. In addition, atheroma can sometimes become inflamed due to the addition of bacterial flora and cause a deterioration in the child’s well-being. - Is it possible to play sports after surgery?
After surgical removal of atheroma, it is recommended to refrain from active activities for 2-3 weeks. This will allow the tissues to fully heal and recover.