Is it worth worrying if black dots appear on a baby’s face, or is this a physiologically based phenomenon? For many new mothers, these rashes on the baby’s face at 2-3 weeks of life are like a bolt from the blue. They begin to blame themselves for poor care, poor nutrition and other imaginary sins. In fact, it is no one’s fault; this is the child’s body’s reaction to hormonal changes. Mothers should calmly care for the baby, and nature itself will take care of the rest.
Why do blackheads appear in babies?
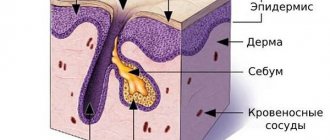
Black spots on the face of an infant are nothing more than comedones. Why they appear in teenagers is clear to everyone - a hormonal explosion. Why in infants? It turns out that for the same reason - an excess of female hormones estrogen, which the baby received from the mother in abundance before birth. This is due to the hormonal changes that occur in the baby’s body. What happens to the skin during this period:
- Spots are not the only problem for infants; often the baby’s skin is covered with acne - blackheads. These pearly papules literally cover the cheeks, nose, forehead, chin and even ears.
- The appearance of comedones and acne in babies in the first week of life is provoked by the maternal hormone estrogen, which narrows the pores and at the same time increases the secretion of secretions from the sebaceous glands of the epidermis. Sebum stagnates in narrowed pores.
- When there is little sebaceous secretion, or sebum, black comedones appear (like small dots), and when there is an excess, acne occurs.
Many people mistakenly believe that acne is caused by allergies, which is not true. Allergies have absolutely nothing to do with it.
Symptoms
Facial skin lesions: comedones, papules, pustules, and in rare cases, cystic nodes.
Neonatal acne is similar to that which occurs in adolescents during puberty. In some cases, they may appear on other parts of the body, such as the neck, ears, or back.
Newborn acne should never be subjected to squeezing. This will not speed up treatment and recovery. You should always remember that there is a danger of introducing an infection into the baby’s body.
Before undertaking any treatment for inflammation that appears in children, it is necessary to clearly determine what exactly you are faced with. Perhaps this is not newborn acne at all, but an allergy. The symptoms may be similar and therefore in this situation it is better to consult a pediatrician and a dermatologist, since only they will be able to distinguish these skin rashes in children.
Juvenile acne represents a global problem for both doctors and patients due to the almost total prevalence of this disease (80-90% or more), long-term course, unpredictability of the outcome with the possibility of the formation of disfiguring scars or transition to adult acne. It is also possible that patients may experience psychological problems associated with the unaesthetic appearance of lesions on the face, which is especially difficult to experience in adolescence. Juvenile acne occurs between the ages of 8 and 21.
The diagnosis is clarified by a dermatologist using: dermatoscopy of rashes; skin pH measurements; bacteriological examination (if there are signs of infection).
Prevention
For children:
- Regular hygiene procedures
- Air and sunbathing
- Do not smear your face with baby creams, oils and lotions
- Keep skin clean and dry
- Do not squeeze pimples, this can cause infection of the sebaceous glands and inflammation.
For teenagers:
- Contact a dermatologist. A dermatologist can prescribe medication to determine the cause of acne.
- Switching to non-comedogenic cosmetics
- Using sunscreen cream
Read more about pediatric dermatology at the YugMed clinic
Features of treatment of infants
Neither acne nor spots on a newborn require any treatment. Hormonal levels will be restored, and the baby’s skin will become soft and clean, just as a baby’s skin should be.
You need to know that the baby himself does not experience any discomfort from the black rashes - they do not hurt, do not itch and go away on their own. There are several tips to help ensure proper skin care for your baby during this period:
- Bathe your child daily, adding decoctions of herbs (chain, celandine, chamomile) and oak bark to the bathtub.
- A concentrated decoction can be prepared for several days and stored in the refrigerator for 3-4 days, adding to the water before bathing the baby.
- Preparing the decoction is very simple: 1 tablespoon of herb per 1 liter of water. Boil over very low heat for 15 minutes so that there is no bubbling when boiling, let it brew and cool for 45 minutes. Be sure to strain through cheesecloth and add to bathing water.
You can make a collection of herbs. But it’s better to try the herbs separately to know how the skin reacts to a particular decoction. The best herb for babies is chamomile. It will relieve inflammation and calm you down. After such a bath, the baby will sleep perfectly.
Black spots on a baby's face do not pose any danger and will soon disappear if the parents do not observe signs of skin inflammation. Facial hygiene, mild detergents that do not dry out the skin, fresh air and a reasonable diet for a nursing mother are the best prevention of dermatological problems.
Acne in newborns does not require any special care products. It is enough to wipe the skin with herbal decoctions, dip a sterile cotton wool in them, and bathe the baby in the evening.
Melanomic nevi
Congenital melanocytic nevus
All congenital nevi are harmless. Among them there are small, medium and giant formations:
1. Congenital small melanocytic nevus (Fig. 2).
Elements of the rash. A spot or plaque raised above the skin measuring up to 1.5 cm. The shape of the nevus is round or oval, the boundaries are clear or blurred. The surface of the nevus is smooth or wrinkled, lumpy, folded, lobed.
Color. Light and dark brown. In rare cases, a depigmented rim is noted.
Localization. Any.
Course and prognosis. The risk of developing melanoma before puberty is virtually non-existent; in later life it ranges from 1 to 5%.
Rice. 2. Congenital small melanocytic nevus
2. Congenital medium melanocytic nevus (Fig. 3).
Elements of the rash. A round or oval plaque raised above the skin from 1.5 to 20 cm. The surface of the formation is smooth or wrinkled, lumpy, folded, lobulated, covered with papillae or polyps.
Color. Light or dark brown, there may be small dark inclusions on a lighter background.
Localization. Any.
Course and prognosis. There is virtually no risk of developing melanoma before puberty. Average congenital nevi change slightly throughout life. Due to the growth of the child, there is a proportional increase in education. It is advisable to remove the nevus before reaching puberty.
Rice. 3. Congenital medium melanocytic nevus
3. Congenital giant melanocytic nevus (Fig. 4).
Elements of the rash. A plaque raised above the skin level measuring more than 20 cm in diameter. There may be satellite lesions along the periphery of the main lesion. A disorder of the skin pattern is characteristic. On the surface of the formation there are nodules, papules and, as a rule, coarse dark hair. The boundaries can be either smooth or uneven.
Color. Darkly pigmented formation.
Localization. Any.
Course and prognosis. According to various sources, the risk of transformation of congenital giant melanocytic nevus into malignant melanoma reaches 5%. Surgical excision of the formation followed by plastic correction should be carried out as early as possible, however, often the operation is not possible due to the size or location of the formation.
Rice. 4. Congenital giant melanocytic nevus
Acquired melanocytic nevus
Acquired melanocytic nevus can be represented by a borderline (transitional) or complex (mixed) nevus. The transition from borderline nevus to complex nevus to intrademal nevus over time demonstrates the normal evolution of neogenesis.
1. Borderline nevus
Elements of the rash. A round or oval spot, sometimes slightly raised above the surface of the skin, up to 1 cm in size, with clear, even boundaries.
Color. Homogeneous (various shades of brown).
Localization. Any.
Course and prognosis. Borderline nevus, which arose in early childhood, becomes mixed as a result of the proliferation of nevus cells and their advancement into the dermis. This usually occurs during puberty. After the disappearance of the borderline component, the nevus becomes intradermal. This natural transformation usually occurs before the age of 30. In some cases, common borderline nevi remain unchanged throughout a person's life.
Rice. 5. Borderline nevus
2. Complex nevus
Elements of the rash. A formation in the form of a papule or node, usually up to 1 cm in size. The surface is smooth, less often warty, often with the growth of bristly hair. In shape, complex nevi are predominantly formations that rise evenly above the skin.
Color. Generally uniform: dark brown.
Localization. Any.
Rice. 6. Complex nevus
Dermal (intradermal, “resting”) nevus
Elements of the rash. A round, dome-shaped formation, usually up to 1 cm in size, rising above the surface of the skin. Over time, the nevus may develop a stalk and may take on the appearance of a warty (papillomatous) nevus. This phenomenon is most typical for formations localized in the torso area.
Color. Yellow-brown, brown or with brown spots, telangiectasias may be observed.
Localization. The most common are the face and neck. Formations of this group on the trunk and limbs are less common.
Course and prognosis. In most cases, intradermal nevi are not treated. Indications for removal of the formation are: localization in which there is permanent injury to the lesion.
Rice. 7. Dermal nevus
Prevention of the occurrence of acquired nevomelanocytic nevi is to reduce exposure to sunlight (especially in the early period of a person’s life). This is achieved by reducing the time spent in the sun (especially during the peak solstice period from 11 a.m. to 4 p.m.) and using sunglasses.
Blue nevus
Blue nevus can be either congenital or acquired; it most often appears in childhood or adolescence. These skin lesions are much less common than nevi of epidermal melanocytic origin. A blue nevus develops from ectopic melanocytes of the dermis. The coloring characteristic of a blue nevus is due to the Tyndall phenomenon - the refraction of light by the pigment of tumor cells located deep in the dermis.
Currently, several types of dermal melanocytic nevi are considered in the nosological form of “blue nevus”: simple blue nevus, cellular, cellular non-pigmented, combined and deeply penetrating.
Rice. 8. Blue nevus
1. Simple blue nevus (blue nevus, Jadassohn–Tiche nevus
Elements of the rash. The nodule, usually up to 1 cm in size, is sharply demarcated from the surrounding skin, round in shape, hemispherically protruding above the skin level, with a smooth surface.
Color. Blue, light blue, dark blue, gray, bluish - black.
Localization. Any type is possible, but the typical location for blue nevi is the dorsum of the hands and feet. A rare arrangement – soft and hard palate.
Course and prognosis. This formation grows quite slowly, often remaining unnoticed for several years. Over time, a blue nevus may acquire a flatter shape and lose pigment. Transformation of a blue nevus into melanoma is extremely rare.
2. Blue cell nevus (proliferating)
Elements of the rash. The development of a nevus begins with the formation of a spot or compaction in the dermis, which then transforms into a node or plaque up to 2.5 cm in diameter.
Color. Blue.
Localization. Any is possible. Quite often the localization of nevus in this group is the gluteal, lumbosacral region, less often on the dorsum of the hands and feet. Rare tumor localizations have been described - the conjunctiva and the scalp.
The diagnosis is made on the basis of clinical and histological signs; immunohistochemical studies are necessary.
Course and prognosis. Depending on the clinical picture, pathomorphological signs, course and prognosis of the process, two forms of blue cell nevus are distinguished: typical (classical) and atypical with uncertain biological potential. Malignant transformation usually occurs over a long period of time in mature or elderly people and is manifested by rapid tumor growth, ulceration and discoloration. With a cellular blue nevus, cells similar to this formation may be observed in the regional lymph nodes. This process is called “benign metastasis.” Treatment is surgical excision with pathological examination.
Spitz nevus (atypical spindle cell, juvenile, benign juvenile melanoma)
Elements of the rash. A small single dome-shaped hairless node measuring up to 1 cm in diameter. Education, as a rule, is singular.
Color. Pink-red with abundant vascularization, yellow-brown, dark brown, uneven coloring possible.
Localization. Any is possible. In children and adolescents, the most common location is the scalp and face.
The diagnosis is made on the basis of histological examination. A quickly growing dome-shaped formation in a child allows one to suspect a Spitz nevus.
Course and prognosis. Spitz nevus is characterized by a sudden appearance. From the moment it appears, the formation is characterized by rapid growth, then it flattens and remains unchanged for years. Some nevi may undergo morphological transformation into dermal melanocytic nevi, and transformation into melanoma is also possible. The risk of malignant tumor degeneration occurs during puberty. Malignant degeneration is rare, but such formations require careful monitoring. This formation must be removed before the end of puberty. Then, in the postoperative period, dynamic observation is advisable.
Rice. 9. Spitz nevus
Halo nevus (Sutton's nevus)
Elements of the rash. A slightly elevated, slightly infiltrated reddish-brown nodule of round or oval shape, with an average diameter of 4-5 mm. The halo nevus is surrounded by a halo of depigmentation. The diameter of the rim, as a rule, is 2-3 times larger than the size of the hyperpigmented nodule. Characterized by multiple skin lesions.
Localization. Any type is possible, but the most common is the back.
Course and prognosis. There are several stages in the course and resolution of halo-nevus:
- melanocytic nevus with a surrounding rim,
- the central element loses pigmentation and acquires a pink color,
- disappearance of the central element,
- complete repigmentation of the entire nevus over several months or years.
No treatment required.
Rice. 10. Halo nevus
What is prohibited to do
Sometimes it happens that acne becomes inflamed. Maybe the baby touched his face with his hands, maybe the mother did, but the child’s blackheads became inflamed and real acne appeared on his face. What should mothers do?
First, let's tell you what you should never do:
- You should not wipe your baby’s face with alcohol-containing lotions, as well as other cosmetics for adults, including black comedones.
- Do not squeeze out blackheads. Some of the pus will go inside, and this can lead to serious complications - boils, boils, phlegmon.
- Do not rub creams, especially oily ones, into the skin. Facial skin does not need any creams. For acne and spots, this will worsen the baby’s condition and lead to inflammation.
The only way to combat inflamed blackheads is to smear them with brilliant green or fucorcin in a spot if self-opening of acne suppuration has occurred.
It is necessary to differentiate between acne and allergic rash. The difference is obvious even to an inexperienced mother:
- With allergies, rashes occur on the body, on the buttocks, on the cheeks. These are usually small rashes that are itchy and annoying. The child is capricious and does not sleep well.
- There may be changes in the consistency and color of the stool.
In case of allergic rashes, you should definitely consult a doctor. Under no circumstances should you give antihistamines without a pediatrician's prescription.
What should you not do for blackheads?
Aggressive agents should not be used to treat an infant. The following rules must be adhered to:
- It is forbidden to squeeze or open blackheads.
- Avoid the use of ointments and fatty creams to eliminate blackheads in infants without consulting a doctor.
- Alcohol solutions should not be used to treat a child.
- The use of powders and talc is contraindicated.
- Without inflammation, do not use iodine, a solution of potassium permanganate or brilliant green.
- It is prohibited to use antiallergic drugs and antibiotics.
The correct treatment will be prescribed exclusively by a doctor after identifying the provoking factor. Self-medication can significantly aggravate the process and cause inflammatory reactions in the form of redness and swelling, drying out the skin. An abscess may also form. His treatment will take longer.
Prevention
Since black spots on the face of an infant arise due to hormonal changes, it is not possible to somehow influence their appearance. Therefore, it is incorrect to talk about prevention. But one condition is always relevant - to avoid pustular inflammation and black comedones, it is necessary to maintain the hygiene of the child’s body, the mother and the baby’s environment.
A child in the first months of life should, if possible, be in conditions appropriate for his maintenance:
- Underwear and bed linen must be washed and ironed;
- diapers should be changed regularly;
- The mother’s hands should be perfectly clean when she is caring for the baby;
- wet cleaning in the room where the baby lives must be carried out daily;
- the rooms are ventilated while the baby is taken out for a walk.
The rules are simple, but the benefits of following them are enormous – the health of the child.