Diagnosis and treatment of skin lesions on the penis can be difficult due to the lack of knowledge on the subject among doctors and patient embarrassment. Although noninfectious lesions are common, especially in younger patients, they are often associated with infectious causes.
Non-infectious lesions of the penis are clinically classified as:
- follo-exfoliative, for example, psoriasis;
- inflammatory, for example, lichen sclerosus, lichen planus;
- vascular, for example, angiokeratoma;
- neoplastic, for example, carcinoma in situ, invasive squamous cell carcinoma.
For lesions located on the penis, different diagnostic and therapeutic options are usually considered than for lesions located outside the genital area. A biopsy is usually performed when the diagnosis is uncertain or if a tumor cannot be ruled out.
Symptoms and diagnostic measures
Fordyce granules most often affect various parts of the face.
The papules are small in size; palpation reveals their dense structure. They have a light shade. The number of such rashes is numerous; each formation reaches 2 mm in size. These papules do not protrude more than 1 mm above the skin surface. Such formations do not bring significant discomfort to their owner. Because of this, cyst formations are considered only a cosmetic defect. If itching or burning appears in the affected area, experts do not recommend scratching it. This can cause wounds to form, which can lead to the spread of infection.
This is especially important for papules on women’s nipples. To avoid worsening the condition of these rashes, you should consult a specialist as soon as possible.
Often patients with this problem take the wrong action, starting to get rid of tumors at home. It is not recommended to do this yourself, because it is not always possible to clear the nodule of liquid on your own. In this way it is impossible to completely neutralize the granules. This method can provoke bleeding and greatly change the situation for the worse.
Diagnosis is carried out by macroscopic analysis. To get a complete picture of the disease, it is necessary to take biological materials. After laboratory tests, a conclusion is made about the presence or absence of seborrheic cysts. If the diagnosis is positive, the doctor selects the necessary treatment method. If the formation does not cause discomfort, then there is no need for treatment. The medical literature does not describe a single case of granules degenerating into malignant ones or threatening the human body.
Classification and examples of local GCS
| Group | Power of action | Examples |
| 1 | very strong | clobetasol 0.05% |
| 2 | strong | betamethasone ointment 0.05% |
| 3 | strong | triamcinolone ointment 0.1% |
| 4 | average | hydrocortisone 0.2% |
| 5 | average | triamcinolone cream 0.1% |
| 6 | small | betamethasone lotion 0.02% |
| GCS - glucocorticosteroids | ||
Therapy and getting rid of the problem
A dermatologist with practical experience will likely be able to easily distinguish this disease without additional tests. All that is required is a thorough inspection. If the rash is localized on the genitals, it is necessary to conduct a diagnosis to exclude the presence of a sexually transmitted disease.
An experienced specialist will explain to the patient the safety of these rashes. Removal of Fordyce granules is carried out at the request of the patient, but this procedure is not mandatory. Therapeutic intervention cannot prevent or change the course of this process. In adolescents, there is a high probability of complete spontaneous disappearance of these granules after the completion of the formation of secondary sexual characteristics. In adult patients, Fordyce granules disappear during menopause.
In cases where papules cause serious aesthetic discomfort, removal of Fordyce formations is desirable. There are several known methods of getting rid of the disease:
- Through a laser. A fairly popular method that young people resort to. Most often applicable if papules are localized on the penis or labia. This method is painful and requires significant financial expenses.
- Using the electrical coagulation method. This method is quite effective. When it is performed, the patient experiences almost no pain. This method can remove papules on the lips.
- Cryotherapy intervention. In this method, liquid nitrogen is used to remove pimples, after which the granules gradually fall off. Depending on the degree of damage, the required number of sessions is selected. Sometimes scarring may appear after the procedure.
- Surgical intervention. Surgery is performed in very rare advanced cases. Using a surgical instrument, the papules are carefully opened and cleared of contents. After this it is carefully processed.
When choosing a method, you must remember that there is no chance of completely getting rid of the problem. Often the problem may return. Therefore, before the procedure, you need to think carefully about its necessity, because it costs a lot of money, and at the same time does not always give a 100% result.
Should I delete it?
As already mentioned, granules should be removed only if they really cause aesthetic discomfort. It is necessary to understand that removal is not the final measure that can prevent the reappearance of papules. On the contrary, they will most likely appear again in the same or some other place. However, a man can decide to remove these formations by resorting to one of the possible methods, for example:
- electrocoagulation,
- radio wave removal,
- laser excision,
- cryodestruction.
These methods can remove almost any growth or neoplasm on the surface of the skin and mucous membranes. Each method has its advantages, disadvantages and contraindications, so before choosing one of them, you should carefully read each one and consult your doctor.
The most preferable, according to many patients and doctors, is the method of radio wave or laser removal. Both methods are characterized by painlessness, minimal trauma, high accuracy, and absence of scars after removal of the tumor. To date, no effective measures have been developed to prevent the formation of Fordyce granules. Some cosmetics have shown positive results in this regard, but it is still difficult to classify them as recommended preventive agents in the general sense of the word.
Existing treatments
Since papules are benign, treatment is not necessary. Doctors do not recommend it because of possible complications. However, if granules are a source of uncertainty, several removal options are offered.
Less invasive therapies:
- Use of prescription creams and oils: Retin-A, when applied externally, increases cell proliferation in the papillary layer, reduces cell adhesion and helps smooth the skin surface. Jojoba oil - eliminates existing papules and prevents the formation of new ones.
- Cryotherapy - freezing. Liquid nitrogen is used. Cold activates the death of tissue, stimulation of the narrowing of the walls of blood vessels begins, and blood flow to a separate area of the body increases. The method is less accurate and must be performed by a professional. No anesthesia is required, but several procedures will be required. Cryotherapy is contraindicated for diseases of the blood and blood vessels, the acute stage of chronic diseases.
- Trichloroacetic acid. A toxic substance that is rarely used in the treatment of Fordyce granules. A common side effect is a prolonged burning sensation.
- Isotretinoin. Treatment takes several months but produces long-term results. One course lasts 12–16 weeks. Causes the following side effects: increased sensitivity to sunlight; mental disorders, including depression.
Clinics offer to get rid of seborrheic cysts using surgical methods. But, after 3–4 years, a relapse occurs in 90% of cases.
Removal of papules
How to get rid of Fordyce granules:
Excision with a punch. The manipulation is carried out under local anesthesia by a dermatologist or qualified cosmetologist. The device makes holes in the skin with a diameter of 1–2 mm. Fordyce granules are removed by hand and stitches are applied. This is an effective method with a low chance of relapse. The downside is the risk of scarring. Deep heating of tissues with currents. Diathermy is performed by a dermatologist, surgeon or general practitioner. To perform this, the patient is given local anesthesia or an anesthetic cream is applied. Only 1 session is required and there is a high risk of scarring. Healing takes 2 weeks. Laser removal. This method is recommended to remove Fordyce granules on the labia, nipples and foreskin. Laser treatment is effective and painless. It is performed using a local anesthetic. The patient returns to normal life after removal. The focused beam from the laser reacts with the skin tissue, burning out the abnormal bumps. Best results achieved with CO2
The laser is precise, which is important when working with small granules on the lips. Recovery is fast
Laser therapy is contraindicated for oncology, heart disease, and tuberculosis.
Do not try to squeeze out white dots. There is no way to get rid of papules this way. There is a high risk of inflammation and scar tissue formation.
Traditional removal methods
Therapy with home remedies gives excellent results. How and how to treat cystic formations:
- Crush 5 mummy tablets, add 50 ml of warm honey. Place the mixture in a water bath and boil for 2 minutes. Cool. Store in a jar with a tight lid. Apply the ointment after fir oil, apply for 15 minutes, rinse. Treat with the prepared product. Carry out up to 15 manipulations. A repeat course is carried out after 6 months.
- Coat onions with honey and bake. Apply to the granules for 30 minutes. You will need to complete 5 sessions to achieve a positive result. Not suitable for therapy on the penis and lips. Use to remove formations from nipples.
- To get rid of papules from the penis and labia, use 1 tsp. olive oil mixed with 1-2 drops of vitamin E and jojoba oil.
- Positive reviews about propolis oil. It can be applied to any part of the body 2-3 times a day. Sold in pharmacies or prepared independently.
Drug therapy
The most effective antiviral drugs are: Acyclovir tablets.
The optimal dosage of Acyclovir is 200 mg. The tablets should be taken 5 times a day. The duration of therapy takes about 10 days Valtrex tablets. The optimal dose is 500 mg 2 times a day. The duration of treatment is limited to one week. If the drug is used to prevent relapse, then the duration of therapy is reduced to 3 days, and the dosage is reduced to 500 mg per day. Panavir ointment. To remove herpes, you should apply the ointment to the affected area 5 times a day. Duration of treatment is 4-10 days. Zovirax injection solution. When treating herpes, the dosage is calculated based on the patient's body weight (5 mg/kg body weight). The drug is administered by infusion every 8 hours. Antiviral drugs should be used by the man's spouse/mistress, since herpes can be sexually transmitted through unprotected sex. Auxiliary preparations for rashes on the penis. When considering the question of how to cure herpes on the penis, one cannot ignore immunomodulatory drugs. It was already noted above that exacerbation of the disease often occurs during the period of immunodeficiency
If you increase your immunity, it is much easier to transfer herpes into a stage of stable remission. What immunomodulators to use if herpes appears on the head of the penis?
Doctors recommend giving preference to the following drugs: Cycloferon. To get rid of herpetic rashes on the skin and immunodeficiency, it is enough to take 2-4 tablets daily. The basic regimen is 1,2,4,6,8, 11, 14, 17, 20, 23 days. If necessary, several treatment courses are carried out.
Apply a thin layer to affected areas 3-4 times a day. To get rid of herpes and increase immunity, it is enough to use the cream for 10 days. In addition to immunomodulators, the patient should use non-steroidal anti-inflammatory drugs (Ibuprofen, Nurofen, Ibuprom). These medications help relieve pain.
Paracetamol can be used to lower body temperature. When treating male herpes, you should also use multivitamin complexes. They will help strengthen the immune system and saturate the body with essential vitamins and macroelements. For genital herpes in men, preference should be given to multivitamins that include ascorbic acid, vitamin E, vitamin A, and B vitamins.
Penile psoriasis
Psoriasis can appear at any age, with two peaks at ages 16–22 and 57–60. Psoriasis usually appears as red or salmon-colored, scaly, ring-shaped plaques, often accompanied by white or silvery scales.
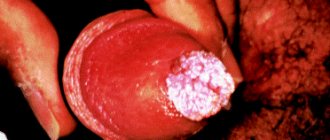
Photo 1. Penile psoriasis
Photo 2. Penile psoriasis
Factors that aggravate the disease include:
- stress;
- alcohol and tobacco abuse;
- acute infections, especially streptococcal infections;
- the use of certain medications, for example, propranolol, lithium salts.
Psoriatic lesions outside the genital area are located on elongated surfaces, which facilitates diagnosis.
Treatment for psoriasis depends on whether it is localized or generalized. First-line treatment for localized penile psoriasis involves the use of low- to moderate-potency topical glucocorticoids once daily.
In general, topical glucocorticosteroids (group 1) at a dose of >50 mg or high-potency glucocorticoids (group 2) at a dose of >100 mg should not be used for long periods of time because their continuous use may cause skin atrophy.
The lesions may reappear after therapy is stopped. In rare cases, when continuous use of local corticosteroids with very high activity is indicated, it should be limited to pulse doses on weekends (use once a day, twice a week).
Intermittent maintenance therapy with topical glucocorticoids (once or twice a week) in areas where exacerbations occur frequently is recommended to prevent relapse and is more effective than emollients alone. Topical vitamin D analogues have comparable efficacy to ShS and should be used separately. If long-term treatment is required, calcineurin inhibitors such as tacrolimus or pimecrolimus may be appropriate, which can help prevent skin wasting but also cause itching.
Biologics are expensive but may be appropriate in patients who do not respond to treatment, have generalized lesions, or have psoriatic arthritis. Biologics for psoriasis may target lymphocyte function-associated antigen-1 (LFA-1), interleukin, interleukin, tumor necrosis factor, or T-cell activation.
Several medications are available to treat psoriasis. including etanercept, infliximab and ustekinumab. Despite limited use in clinical settings, there is evidence for the use of these new biologics in combination with conventional treatments such as methotrexate, cyclosporine, acitretin, or phototherapy in severe, refractory cases.
Symptoms and diagnostic features
The granules themselves are not dangerous, especially if there is no or barely noticeable itching. But you should consult a specialist if you notice such skin signs. It's not just and not so much a matter of aesthetic correctness. Firstly, any rash is a sign of ill health. Secondly, similar skin manifestations may indicate:
- Infectious diseases (lichen planus, molluscum contagiosum).
- Pathologies combined with oncology (“shagreen skin”).
- Dermatitis or neurodermatitis.
And these diseases require serious, sometimes long-term treatment.
As a rule, the diagnosis includes only one stage - a physical examination by a specialist and a survey of the patient. In some cases, when it is externally impossible to distinguish Fordyce granules from the primary elements of the rash in other pathologies, a histological analysis is prescribed - a smear or biopsy.
If the hormonal nature of the disease is suspected, blood tests are taken for biochemistry and the patient is sent for examination to an endocrinologist. After making a diagnosis, the doctor determines the extent of the need for treatment. It depends on how much these rashes spoil the aesthetic appearance of the patient's skin.
Therapeutic options for non-infectious penile lesions
| Diagnostics | The main method of struggle | Alternative Methods |
| Papular and scaly changes | ||
| Psoriasis | local GKS | vitamin D analogues 3, tacrolimus, pimecrolimus |
| Inflammatory changes | ||
| Lichen sclerosus | local GKS | circumcision for lesions limited to the foreskin |
| Ringworm | observation | topical corticosteroids, tacrolimus, pimecrolimus |
| Lichen planus | local GKS | circumcision for lesions limited to the foreskin |
| Vascular changes | ||
| Angiokeratoma | observation | surgery, cryoablation, electrocoagulation, laser ablation |
| Tumor changes | ||
| Cancer is in place | circumcision for lesions limited to the foreskin | Mohs microsurgery technique, topical imiquimod |
| Invasive squamous cell carcinoma | circumcision for lesions is limited to the foreskin; Mohs microsurgical technique for non-isolated lesions | partial or radical removal of the penis, radiation therapy, brachytherapy |
When to see a doctor?
In most cases, papulosis on the penis does not cause its owner any problems other than psychological discomfort. A man should seek professional advice from a specialist if the following alarming clinical signs occur:
- Itching.
- The appearance of bloody discharge from the penis.
- Swelling of the penis.
- Pathological changes in the nodule (color, shape, size).
- Redness of growths on the pubis and genitals.
- Painful sensations.
The patient should also be alerted to multiple neoplasms affecting almost the entire coronary sulcus, especially if they hurt, burst, crack, itch, etc.
In such cases, neoplasms can act as a sign of herpes, syphilis and other infectious diseases that are sexually transmitted and require timely medical attention. Therefore, having noticed the painful signs listed above, a young man should contact a qualified venereologist who will make an accurate diagnosis and prescribe the optimal treatment.
Preventive actions
Due to the lack of consensus on the cause of the cosmetic defect, there are no precise recommendations for its prevention.
But it won’t hurt to follow the classic recommendations for a healthy lifestyle. This is first of all:
- complete renunciation of addictions;
- following the rules of personal hygiene;
- routine examination in medical institutions.
If a man discovers Fordyce rashes on the genitals, then he begins to worry only because of the external defect. But this is unnecessary worry, because first of all it is necessary to find out the root cause of the development of this problem and begin to eliminate the pathology. To do this, it is advisable to contact a specialized specialist.
Reasons for the appearance of Fordyce granules on the foreskin
New growths on the head of the penis are called pearlescent papules. The nodules are whitish or yellowish in color with a pearlescent tint and form groups. They are dense to the touch and resemble millet seeds in appearance. Their size often does not exceed 1 mm in diameter. In women, formations can be localized on the nipples. According to statistics, representatives of the stronger sex are affected by Forks-Fordyce disease twice as often as the fair half of humanity. Even on the lips and in the oral cavity, rashes are more common in men than in women.
Experts have still not come to a consensus regarding the reasons for the appearance of pearlescent nodules on the body. Some are inclined to assume that rashes are provoked by the location of the sebaceous glands too close to the surface of the skin, and the narrowing of the excretory channels leads to the accumulation of sebaceous gland secretions. Other doctors believe that the cause of pearlescent granules is a change in hormonal levels during adolescence during puberty. This opinion is prompted by the fact that the first rashes appear in young men under the age of 20 and miraculously disappear when they cross the forty-year mark. A smaller percentage are those experts who claim that hyperplasia of the sebaceous glands is caused by non-compliance with hygiene rules and the influence of bad habits.
If you find rashes on the genitals, consult a specialist for an accurate diagnosis. Fordyce granules on the penis are very similar to other more serious diseases:
- eczema;
- neurodermatitis;
- secondary period of syphilis;
- molluscum contagiosum;
- lichen planus.
Localization of formations and how to distinguish them from other growths in the groin
Fox Fordyce granules are not dangerous, they look like small yellowish tubercles on the penis with a radius of 1-2 mm, less often they reach 4-5 mm. A cluster of nodules can be localized over the entire area of the intimate organ. More often, formations are fixed under the skin of the scrotum, in the groin.
Fordyce formations are dense to the touch and do not cause discomfort to a man. A person may have a genetic predisposition to the appearance of granules; due to the enlargement of glands under the influence of androgens, growths appear on the penis. Hormonal surges provoke the development of nodular rash in adolescence.
Attributes on the testicles and groin may appear due to pathogenic processes. To distinguish benign Fordyce papules from malignant formations, diagnostics are carried out.
Types of pathologies on the penis and characteristic symptoms of granules:
- Numerous pale pink pimples along the edge of the head are pearlescent formations that appear under the influence of hormonal imbalances. When tissues become inflamed, swelling and redness are observed.
- Acne, similar to granules, discovered by Fordyce, distributed over the surface of the penis, accompanied by painful sensations, may indicate the initial stage of human papillomavirus infection. Over time, condylomas enlarge, forming growths.
- Papillomatosis is a viral disease accompanied by neoplasms on the penis; the nodules are similar to the granules that Fordyce studied, have a soft consistency, and are located along the edge of the head.
- Flat red formations in the groin are often warts. They are characterized by a round apex with a characteristic thickening of the stratum corneum.
- Small bodily rashes on the penis indicate an allergy; the granules look like red spots. The development of formations resembling elements of F. Fordyce is caused by unsuitable detergents or poor personal hygiene. A nagging pain in the lower abdomen, uncharacteristic discharge from the penis that accompanies the appearance of granules may indicate a sexually transmitted disease. A doctor makes a diagnosis, excludes the possibility of pathological processes in the body, and prescribes therapy.
- Fluid-filled papules signal genital herpes; the infection appears within a week after infection. Often a harbinger of the development of water nodules on the penis is severe itching.
- If there are symptoms uncharacteristic of Fordyce granules, make an appointment with a venereologist or dermatologist. The specialist will determine the origin of the formation and prescribe therapeutic methods.
Diagnostics
Only a doctor can determine the nature of the rash and its causes. In addition to the appearance of white rashes, the following accompanying pathological symptoms are the reason for contacting a medical institution:
- discharge from the urethral canal;
- painful sensations in the lower abdomen or in the external genital area;
- discomfort when exposing the head of the penis;
- appearance of blood;
- erosion of the mucous membrane or skin;
- itching and burning of varying intensity;
- urinary disorders;
- swelling of the tissues of the external genitalia;
- cracks in the frenulum and foreskin;
- spots or red spots on the foreskin.
To make a correct diagnosis, the doctor conducts a physical examination and prescribes the necessary laboratory tests:
- general clinical urine and blood tests;
- bacterial culture of urethral discharge and surface of rashes.
In some cases, additional laboratory and instrumental research methods may be required:
- detection of viral DNA in biological fluids or determination of antibodies to them;
- ultrasound examination of the prostate and other organs.
As a result of the diagnosis, the causative agent of the disease will be identified and adequate treatment will be prescribed.
Prevention
To prevent the future appearance of multiple formations in the form of white dots, it is important to follow certain rules of prevention and monitor your lifestyle and diet. The following measures are considered mandatory for all men
- Careful hygiene. It includes cleansing the intimate area and showering twice a day.
- Personal care products. The razor, washcloth, and towel should not be used by other people (even close ones).
- Protected sex. For casual sexual contacts, barrier contraception should be used.
- Cloth. Underwear should be made of natural fabrics, of appropriate size, so that there is always access to air.
- Control of chronic diseases. Involves regular examination and timely completion of a course of treatment.
In addition, you should be careful when visiting tattoo parlors, where infection is possible when using unsterile instruments.
Prognosis for growth on the penis
Sometimes the growths under the head of the penis disappear on their own.
In other cases, they are a sign of a serious illness.
For example, syphilis or a malignant tumor of the penis.
It also happens that the growths do not pose a threat.
But they do not disappear on their own.
They remain on the penis until they are removed surgically.
In any case, if a growth appears on the penis, you should consult a doctor.
Because any rash is just a symptom.
A diagnosis is required to understand:
- will the growth disappear?
- does it pose a health risk?
- does it need to be removed?
- what is the risk of reappearance after removal
Most growths do not pose a significant threat to human health.
Especially if they do not hurt, there are no signs of inflammation or ulceration.
The prognosis will be favorable if the formation appeared a long time ago and does not increase in size.
But sometimes the disease progresses.
This is possible with:
- any inflammatory processes, especially against the background of immunodeficiency (folliculitis, molluscum contagiosum, condylomas)
- tumors (most often they are benign and grow very slowly)
- dermatological diseases
Diseases can occur in waves, with exacerbations and remissions.
Then the patient requires maintenance therapy.
Sometimes it is performed only during the period of relapse of the disease.
A number of situations require surgical removal of growths.
You can delete:
- molluscum contagiosum
- atheroma
- benign skin tumors
- condylomas
- warts
- nevi (moles)
The procedure is painless and quick.
While the growths are small, they can be removed without the risk of scarring.
Sometimes a relapse occurs after removal.
The growths appear again.
This is possible with condylomas, as well as incompletely removed tumors and nevi.
Varieties of Fordyce granules
The properties of the sebaceous glands can be divided by gender:
Pearly papules on the head of the penis do not threaten health and are not transmitted to a partner. Approximately 30% of men experience such features. This does not prevent them from living fully.
Pearly papules appear during the boy’s maturation and are associated with a large amount of androgens in the blood. Among peoples who practice circumcision of the foreskin, cases of rash on the glans penis are rare.
Morbus Fox-Fordyce is a pathology that is classified as a disorder of the ovaries and thyroid gland. Externally, these are small rashes in the armpits, navel, pubic area, perineum and other places. More often it occurs in girls under forty years of age. Much less common in adolescents and women during menopause.
There are 2 types of Fordyce granules:
- pearly penile papules;
- Fox-Fordyce disease.
Pearly penile papules are a normal variant. According to various authors, they occur in 30% of young men. They do not cause harm to health, are not sexually transmitted, and do not cause complications. In medicine, this problem has been little studied due to doctors’ lack of awareness of the presence of this manifestation. No effective treatment has been proposed.
The reason for the appearance of this type of Fordyce granules is also not clear. Some authors consider the cause to be excessive proliferation of the epithelium of the excretory ducts of the glands of the penis. Others are inclined to think about fibroplastic proliferation of areas of the epithelium of the glans penis.
Pearly penile papules appear during puberty and indicate a sharp increase in androgens in the blood. Among peoples who practice circumcision, the incidence of these papules is extremely low. This is due to the fact that an increased amount of secretion and smegma, which irritate the epithelium of the penis due to their physicochemical properties and cause fibroplastic proliferation (growth), is more easily released during hygiene procedures.
Fox-Fordyce disease is an analogue of pearly papules, only in women. Her clinic is absolutely identical to the clinic of pearly penile papules. The lesion is localized in the apocrine sweat glands and is associated (to some extent) with the genitourinary system. Endocrine origin is suspected.
In traditional medicine, there are two types of sebaceous cysts. In the first case, the granules are presented in the form of nodular papules. They do not result in painful symptoms and are not considered to require therapeutic intervention. Pearly papules often form on the labia, and in men - on the testicles (scrotal area) or penis.
By circumcising the foreskin, the likelihood of sebaceous spots forming on the glans penis is minimized. This is due to the fact that after circumcision the local number of sweat glands decreases. And those that remain easily remove sweat and are cleaned even during simple hygiene procedures (due to very thin skin)
The second type of granules is Fordyce's disease. A distinctive feature of the disease is that the rash is observed only in females. This is due to the anatomical structure of the urinary system.
Lichen sclerosus
Lichen sclerosus of the penis, also known as balanitis obliterans, can occur at any age. The average age of patients at diagnosis is 42 years, and the incidence is 1 in 300 men. In 4–6% of patients, lichen sclerosus is associated with the development of squamous cell carcinoma. Genital lichen sclerosus is considered a precancerous condition.
Lichen sclerosus appears as a hypopigmented lesion with a surface resembling wrinkled paper or cellophane. It mainly affects the glans penis and foreskin. There may be visible blisters, erosions and skin atrophy. Patients usually have phimosis, painful erections, difficulty urinating, itching, pain and bleeding.
Photo 1. Lichen sclerosus
Photo 2. Lichen sclerosus
Because skin lesions can obstruct the urethra, the first symptom in patients may be urinary retention. Although lichen sclerosus can affect almost any part of the body, some people may have no symptoms. It must be differentiated from carcinoma in situ, leukoplakia, and systemic sclerosis. If squamous cell carcinoma cannot be ruled out, a biopsy is indicated.
- In the treatment of lichen sclerosis, topical fluorinated glucocorticoids with moderate to very high potency are usually used to reduce symptoms and prevent malignant transformation.
- With very high efficacy, GCS pulse therapy is effective and safer than long-term daily use of weaker GCS.
- Tacrolimus or pimecrolimus may also be effective, but their safety for long-term use has not been established.
Surgery is indicated for persistent lesions or if there is clinical suspicion that changes in the penis may be squamous cell carcinoma. In uncircumcised patients with lichen sclerosus limited to the glans and foreskin, removal of the foreskin (circumcision) may be indicated. For severe lesions, reconstructive surgery may be required, although if the risks of surgery outweigh the potential benefits, conservative treatment may be appropriate.
Systemic medications such as retinoids and methotrexate are indicated for the treatment of severe lichen sclerosus or when topical treatments are ineffective. Long-term follow-up with periodic physical examination is necessary to monitor the patient for malignant transformation.
Treatment
Fordyce granules are a congenital feature of the body. It is not harmful to health, so there is no need to treat or remove cysts. Some consider this phenomenon a physical defect. If you really want to get rid of tumors, you can consult a dermatologist. The doctor will choose the appropriate way to solve the problem.
Sometimes men try to squeeze out such nodules. But this is not recommended. Due to damaged skin, there is a high risk of infection. And at home it is difficult to comply with all antiseptic standards. In addition, after healing of microtraumas, scars remain. And they look much less aesthetically pleasing than granules.
Topical medications combat fresh rashes. Doctors recommend herbal gels and oils. Positive results are shown by ointments and creams with retinol or its metabolites. But it should be remembered that such remedies will not cope with old cysts. The most effective methods for removing Fordyce granules in men are the following procedures.
Laser coagulation
Exposure to a laser beam. During the procedure, the fatty contents of the granule are evaporated. Manipulations in one area take a couple of minutes. The instrument is precisely targeted and does not affect the deep layers of the skin and surrounding tissues. The method is completely bloodless, so there is no risk of infection. Recovery occurs quickly, but scarring is possible.
Electrocoagulation
Cauterization of tumors with electric current. The procedure is not long. After it, a crust remains on the treated area, which disappears after a few days. In its place, thin, young skin appears, which soon takes on its normal appearance. During the manipulations, damaged vessels are soldered together, so there is no bleeding. Disinfection also occurs at the same time. Disadvantages include a longer recovery period and a high risk of scar formation.
Radio knife
The device emits radio waves, which cause the granule cells to evaporate. The procedure is quick and painless. Adjacent tissues are not injured, recovery takes no more than a week. But this method can only remove small seborrheic cysts. With old and deep tumors, the method may not produce results.
Cryodestruction
Removal of tumors with liquid nitrogen. This gas has an ultra-low temperature. It freezes the cells, after which they are destroyed. This method does not require anesthesia. But the recovery process is quite long. In addition, during the manipulation, surrounding tissues and deep layers of skin are affected.
Before you decide to remove Fordyce granules from your penis, you need to think carefully and consult with a specialist. Any procedure to destroy seborrheic cysts has contraindications and side effects. Considering the absolute safety of such neoplasms, the harm from the intervention will be greater than the benefit. In addition, no method will get rid of nodules forever. After some time, the gland ducts will still become clogged.
Methods of treatment and removal of Fordyce granules in men
There is no drug treatment to eliminate benign seborrheic cyst nodules on the penis. The disease does not require therapeutic intervention; if itching occurs, the doctor prescribes a soothing ointment. Surgeons suggest that patients remove Fordyce granules on the glans in men to improve the cosmetic condition of the epidermis. Surgical methods for treating growths:
- Using a laser. A powerful stream of light is directed to the center of the white spot on the penis, which allows you to eradicate seborrheic granules in large quantities in one session. The procedure does not provoke bleeding, the wound surface heals quickly.
- Cryotherapy is a targeted effect of extreme cold on Fox Fordyce granules. The technique is traumatic, the formations are small in size, and when treating the epidermis on the penis, nearby tissues are affected.
- Electrocoagulation is a cosmetic procedure based on the elimination of F. Fordyce elements with microcurrent.
Operations to remove granules localized on the penis are carried out cyclically: the reappearance of purple papules is observed 2–3 years after their elimination.
A traditional medicine used to improve the aesthetic appearance of the surface covered with Fordyce papules is jojoba essential oil. The substance is used to wipe the skin on the penis affected by the granules. The effectiveness of therapy is low; the product cannot be used without consulting a doctor.
Growths on the head of the penis
CISS A7 Cherepovets, reviews of printers and MFPs
Many men suddenly discover strange formations on their genitals. However, don't panic right away.
Growths on the head of the penis are not always a symptom of any disease; in some cases, these may be normal variants that do not require any correction.
In order to clarify these issues a little, we will consider several reasons for the appearance of such formations.
Pearl necklace
A pearl necklace or pearlescent papules are the normal variant that we discussed above.
These papules are small white growths on the head of the penis, which are located in the form of one or more rings around the entire circumference of the head.
The appearance of such formations is associated with hormonal changes in the male body during puberty.
https://youtube.com/watch?v=AOGKQeo4LOs
This theory is supported by data that pearlescent papules in most cases appear in young people aged 15-20 years and go away on their own by the age of 30-35. Male sex hormones androgens stimulate the production of an increased amount of smegma, which has an irritating effect on the epithelium and leads to its proliferation, i.e. proliferation.
Treatment of these growths is not required, but if something bothers a young person, they can be removed using radio wave surgery, cryodestruction, electrocoagulation or special medications.
Choosing a specific method for treating growths on the head of the penis requires an examination and adequate diagnosis, because each method has its own contraindications. In our clinic we use many effective and modern types of treatment, which we carefully select for each patient.
Papillomas on the head of the penis
Growths on the head of the penis can be a manifestation of papillomavirus infection. In this case, specific growths that resemble cauliflower appear at the sites where the virus enters the body. They are called genital warts.
It should be borne in mind that HPV infection does not necessarily mean the development of pathological formations. The occurrence of condylomas in infected people is associated with the characteristics of the immune system.
In some patients, symptoms never occur; in others, the virus does not manifest itself for a long time, and condylomas appear several months or even years after contact with the virus.
With HPV, condylomas can be located anywhere in the genital organs, but most often they find growths under the head of the penis, in the area of the coronary sulcus, near the urethra and in the perianal area.
Condylomas on the genitals must be removed, because... they tend to increase and grow. Such formations rarely exist asymptomatically. Over time, they begin to itch, cause pain, become injured and bleed from friction with clothing. In some cases, human papillomavirus infection can trigger the development of penile cancer in men.