Pharyngitis is an inflammatory process that forms on the back wall of the larynx and affects the mucous membrane, as well as deeper layers, tissues of the soft palate and lymph nodes. The acute form of pharyngitis can develop into chronic if the patient does not seek help from a doctor and self-medicates.
Since the pathological process in the larynx is caused by the spread of pathogenic bacteria, the risk of developing pharyngitis increases in people with a weak immune system and in those who suffer from ENT diseases or are predisposed to them.
How dangerous is pharyngitis and how does it manifest itself? Which doctor should I contact and how to treat the disease? We will answer these and other questions in this article.
ICD - pharyngitis:
- J02 - acute pharyngitis
- J02.0 - streptococcal pharyngitis
- J02.8 - acute pharyngitis caused by other specified pathogens
- J02.9 - acute pharyngitis, unspecified
- J31.2 - chronic pharyngitis
- J31.1 - chronic nasopharyngitis
Pharyngitis is rarely isolated as a separate disease; the diagnosis is usually acute respiratory viral disease (ARVI).
ARVI is a general name; the doctor usually specifies how exactly ARVI manifests itself.
This may be rhinitis (runny nose), pharyngitis (red throat), nasopharyngitis (inflammation of the nose and throat), etc.1,2
It is important not to confuse pharyngitis with tonsillitis.
To do this, let's understand the structure of the pharynx and oral cavity.
Etiology
Epiglottitis can be caused by bacterial, viral, and fungal pathogens.
In healthy children, most cases of epiglottitis are caused by a bacterial infection. The most common pathogen is Haemophilus influenzae type b (Hib). Other pathogens are pneumococci, streptococci (including group A beta-hemolytic streptococcus, GABHS), Staphylococcus aureus (including its methicillin-resistant strains, MRSA).
In adults, epiglottitis is associated with a wide range of bacteria, viruses, fungal infections, and combinations thereof.
Among the non-infectious causes of epiglottitis, traumatic ones are most often diagnosed: ingestion of a foreign body, thermal burn, burn with acid or alkali.
Epiglottitis can be one of the manifestations of chronic granulomatous diseases (polyangiitis, sarcoidosis, systemic lupus erythematosus, etc.).
Structure of the pharynx
The pharynx is divided into 3 sections:
- upper (nasopharynx)
- middle (oropharynx)
- lower (larynx)
This division is very conditional, because There are no clear boundaries between departments. When inflammation occurs, it rarely happens that the inflammatory process is localized in one section; usually infectious processes spread and move throughout all sections of the pharynx5,7
As can be seen in the picture below, the oropharynx is composed of the velopharyngeal arches, the uvula and the soft palate.
Pharyngitis usually affects:
- temples
- tongue
- soft sky
- posterior wall of the pharynx
The doctor uses a spatula to completely examine the pharynx. It is needed to improve visibility of the back of the throat.
The palatine tonsils also become inflamed with pharyngitis, because it is impossible to limit the inflammation process. This widespread nature of inflammation in pharyngitis distinguishes it from tonsillitis, where the tonsils are predominantly affected.
How common is pharyngitis?
Pharyngitis, like a common ARVI (viral infection), occurs quite often. The incidence rate increases during the season from September to May, with a peak in February and March. A decrease in the incidence of pharyngitis by 3-5 times is observed in the summer months.10,11
Acute pharyngitis occurs more often in childhood than in adults. Children under 5 years of age suffer viral infections, including pharyngitis, 6-8 times a year.8,9
In the first year of visiting a preschool institution, the incidence of the disease is 10-15% higher than in children at home. But, unfortunately, “home” children subsequently get sick more often at school age.
Symptoms
Clinical features of epiglottitis vary depending on the etiology, age, and severity of the disease.
In young children, respiratory distress syndrome is usually diagnosed - a progressive respiratory disorder, manifested by shortness of breath, chest depression during inspiration, cyanosis, pallor of the skin, and wheezing when breathing. To facilitate breathing, the child takes a sitting position with the body tilted forward, the neck is extended, the chin is pushed forward. Drooling may occur.
In older children, adolescents and adults, epiglottitis is more often manifested by a sore throat and drooling. During pharyngoscopy (examination of the pharynx), there is often no hyperemia and swelling - the oropharynx looks healthy.
Epiglottitis in children is characterized by a sharp onset and rapid progression of the disease. As a rule, 12-24 hours pass from the moment of the first signs to hospitalization.
The main symptoms of the disease in children:
- difficulty breathing (80%);
- stridor - noisy, wheezing breathing (80%);
- muffled voice or hoarseness (79%);
- pharyngitis (73%);
- fever (57%);
- sore throat (50%);
- sensitivity of the anterior surface of the neck (38%);
- cough (30%);
- difficulty swallowing (26%);
- voice change (20%).
The main symptoms of the disease in adults:
- sore throat (90-100%);
- fever ≥37.5°C (26-90%);
- muffled voice (50-80%);
- drooling (15-65%);
- stridor (33%);
- hoarseness (20-40%).
Causes of pharyngitis and tonsillitis
Etiology (origin, cause) of pharyngitis. In 70-90% of cases, pharyngitis is caused by viruses. Pharyngitis can also be caused by bacteria, fungi, allergies, injuries, and exposure to irritating factors.
The most common viruses are rhinoviruses, adenoviruses, influenza, parainfluenza, enteroviruses, Coxsackie A, coronaviruses, a group of herpes viruses (Epstein-Barr virus, cytomegalovirus, HSV).12
There are pharyngitis, which are classified as a separate diagnosis depending on the pathogen, for example streptococcal pharyngitis ICD J02.0
Reasons for the development of pharyngitis
Experts believe that the peak development of pathology occurs at the end of winter and the beginning of spring, since at this time the human immune system is especially susceptible to colds. Often in the spring season, a lack of vitamins and microelements in the human body leads to the appearance of vitamin deficiency, the body weakens and creates an excellent environment for the development of pathogenic bacteria. Inflammatory processes are also possible: both separately and against the background of the underlying disease.
The first signs of pharyngitis and its further treatment may differ depending on the stage of the pathology, gender, age and general health of the patient.
We include the following as the main reasons for the development of pharyngolaryngitis:
- hypothermia, eating too cold foods;
- deformation of the nasal septum;
- strains of microorganisms that cause the development of chlamydia, candidiasis, whooping cough, scarlet fever, measles;
- adenovirus, influenza virus;
- streptococci, staphylococci, pneumococci;
- sinusitis, tonsillitis, caries, rhinitis;
- difficulty breathing through the nose;
- pathologies of the gastrointestinal tract: reflux, heartburn, hernia;
- abuse of bad habits;
- regular high loads on the vocal cords;
- polluted, toxic air;
- hormonal disorders and endocrine pathologies (diabetes mellitus, obesity, hypothyroidism, etc.);
- tonsillectomy, which was performed on the patient previously;
- infectious diseases in chronic form;
- weakened immunity.
Classification of pharyngitis
Pharyngitis can be acute or chronic. Acute is inflammation that just arose (suddenly), and chronic is a disease that persists for a long time, and it may not bother a person, but under certain circumstances again cause complaints and anxiety.3
| CLASSIFICATION | A COMMENT | ||
| classification: | Classification of pharyngitis due to its occurrence: | a comment: | viral bacterial fungal allergic traumatic caused by exposure to irritating factors caused by gastrointestinal diseases (gastroesophageal reflux, stomach diseases, etc.) |
| classification: | Pharyngitis associated with specific pathogens: | a comment: | Epstein Bar virus for infectious mononucleosis Yersinia enterocolitica for yersinial pharyngitis gonococcus for gonorrheal pharyngitis Leptotrix buccalis for leptotrichosis of the pharynx |
| classification: | Types of chronic pharyngitis: | a comment: | hypertrophic (enlargement of the mucous membrane) atrophic (depletion of the mucous membrane) catarrhal (standard inflammation) mixed |
Diagnosis of pharyngitis
Acute pharyngitis can be determined by patient complaints and examination of the oropharynx (pharyngoscopy).
Objective symptoms of pharyngitis, which are assessed by a doctor when examining the throat:
- swelling and hyperemia (redness) of the pharyngeal mucosa
- purulent or mucopurulent plaque on the walls of the pharyngeal mucosa
- the presence of inflammation in the arches, tonsils, orifices of the auditory tubes
- the presence of bright red tubercles on the back surface of the pharynx and on the side - hypertrophied (enlarged) lymphoid follicles
- thinning of the mucosa with areas of exfoliating epithelium, crusts and viscous mucus (atrophic pharyngitis)
Based on this, the doctor can make not only a diagnosis of pharyngitis, but also suggest its cause (viral inflammation, fungal infection, etc.).
Despite the fact that 70% of acute pharyngitis is a viral disease, sometimes it is necessary to exclude a bacterial cause. This is very important for further treatment tactics and prevention of complications. To do this, you should conduct a rapid test to exclude the streptococcal nature of pharyngitis.
In some cases, with fever, long-term complaints, or a temperature exceeding 3 days, it is also necessary to take a general blood test to understand the cause of acute pharyngitis.
Survey
In adolescents and adults, laryngoscopy (examination of the larynx) and fibrolaryngoscopy (examination of the larynx with a flexible endoscope inserted through the nasal cavity) are the generally accepted standard for diagnosing epiglottitis.
In children, the diagnostic method depends on the age and severity of the disease. Laryngoscopy is not always possible or safe, so the diagnosis is often made based on the clinical picture. If necessary, it is confirmed by an X-ray examination of the neck in a lateral projection.
During laryngoscopy, the doctor identifies inflammatory changes in the larynx, swelling of the epiglottis, laryngeal cartilage, and vestibular folds. Palpation of the anterior neck may be tender, especially in the area of the hyoid bone.
Patients with epiglottitis (especially if Hib infection is suspected) should always be examined for the presence of extralaryngeal foci of infection: pneumonia, cervical lymphadenitis, septic arthritis, and less commonly, meningitis.
Laboratory assessment should include a complete blood count with leukocyte count, blood culture for sterility, and in intubated patients - bacteriological examination with sampling of material from the epiglottis area.
Differential diagnosis
True croup (diphtheria) . The clinical picture of diphtheria is sometimes similar to that of epiglottitis. Symptoms—sore throat, malaise, and low-grade fever—usually appear gradually. Diphtheria is extremely rare in countries with high levels of immunization against diphtheria, tetanus and whooping cough.
False croup . The main symptom is a barking cough. It is not observed with epiglottitis. Children with croup usually feel comfortable lying on their back.
Bacterial tracheitis . There is an acute onset, a rapid increase in upper respiratory tract obstruction, and fever, which is similar to epiglottitis. Upon examination, no changes in the laryngopharynx are revealed, and radiographs reveal irregularities in the tracheal wall, and there are no changes in the epiglottis.
Peritonsillar abscess . In children with peritonsillar abscess or other infections of the oropharynx (retropharyngeal abscess, acute tonsillopharyngitis), the development of the disease is slower, breathing at the onset of the disease is not difficult, and intoxication is less pronounced than with epiglottitis.
Foreign bodies in the larynx, trachea and esophagus can cause complete or partial airway obstruction, which requires immediate treatment.
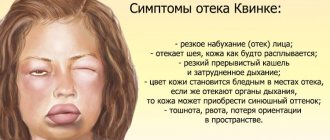
Angioedema (Quincke's edema) . Characterized by rapid onset without previous symptoms of cold or fever. The main manifestations are swelling of the lips and tongue, urticaria, dysphagia without hoarseness.
Upper respiratory tract trauma , including thermal burns.
Complications of pharyngitis
Acute pharyngitis usually responds well to treatment. The prognosis for viral pharyngitis is recovery.
Bacterial (streptococcal pharyngitis) can be complicated by the formation of a retropharyngeal abscess, and subsequently have a negative effect on the heart and kidneys, causing endocarditis and glomerulonephritis.
Symptoms of pharyngitis can persist even with proper treatment, if the true cause of pharyngitis is not eliminated. For example, if gastroesophageal reflux disease (damage to the gastrointestinal tract) is not treated, then pharyngitis will constantly remind itself.
Acute pharyngitis can become chronic.
Prevention of pharyngitis
To prevent pharyngitis, it is recommended:
- avoid hypothermia and dress appropriately for the weather
- avoid contact with tobacco and chemical irritants
- carry out frequent ventilation of working and living spaces
- walk outdoors more often. Walking will help strengthen the body's defenses in the fight against pharyngitis.
- don't drink ice water
- do not share food and cutlery, cups
- avoid crowded places and, if possible, stay in them for as little time as possible
- use disinfectants, including in public places,
- transport, etc.
- wash your hands often
Pharyngitis in pregnant women
During pregnancy, a woman's body's protective properties decrease. In this regard, the risk of contracting infectious diseases, as well as exacerbation of chronic diseases, greatly increases.
Pregnant women need to carefully monitor their health and prevent diseases: avoid contact with people with respiratory diseases, avoid crowded places, wash your hands, eat regularly and properly.
If you develop acute pharyngitis or exacerbation of chronic pharyngitis, treatment is required. It is not recommended to use drugs that can affect the entire body. They can pass through the placenta to the baby and cause harm to him. To treat pharyngitis, pregnant women are advised to consult a doctor and use saline mouth rinses.
FAQ
Can pharyngitis be treated at home?
Pharyngitis usually does not require hospitalization (hospital treatment). You can treat strep throat at home on your own by using topical remedies to relieve sore throat and sore throat. If, after self-treatment, the sore throat does not go away within 3 days, then you should consult a doctor. If you have a fever in addition to a sore throat, you should immediately consult a doctor.
Which doctor should I contact if I have a sore throat?
If you have a sore throat, sore throat, or difficulty swallowing, you should first consult a therapist or pediatrician if you are a child. If there are indications, the doctor will prescribe a consultation with an ENT doctor.
Very severe sore throat. Are you sure I don't have a sore throat?
With pharyngitis, the pain syndrome may be more pronounced than with tonsillitis (tonsillitis). To treat pharyngitis, it is good to use a remedy that has an analgesic effect, for example Tantum® Verde. To exclude sore throat (streptococcal tonsillitis) or streptococcal pharyngitis, it is recommended to conduct a rapid test (streptotest).
Do you need an antibiotic for pharyngitis?
The antibiotic is indicated ONLY for bacterial pharyngitis. For a quick diagnosis, perform a rapid test for streptococcus. It will allow you to exclude or confirm the bacterial nature of pharyngitis. If streptococcus is detected, the doctor will prescribe antibiotics.
Is strep throat contagious?
Most often, strep throat is a viral disease, so a person can shed the virus and infect other people. A sick person is contagious, so you should stay at home until you recover.
What happens if pharyngitis is not treated?
Complications may arise. If pharyngitis is not treated, complaints persist much longer, inflammation does not go away and begins to become chronic.
Is it possible to get vaccinated for pharyngitis and when?
Against the background of an acute illness or exacerbation of chronic pharyngitis, vaccination is contraindicated. Wait until you have fully recovered and then you can get vaccinated. The exception is vaccination against influenza. It can be done when the temperature is normalized, i.e. There is no need to wait for all symptoms to disappear.
Is it possible to eat cold food if you have a sore throat?
If you have pharyngitis, it is not recommended to eat very cold foods, including ice cream. This can increase inflammation and slow down recovery.
Sore throat in children: forms and clinical manifestations
Depending on the nature of the change and the degree of damage to the tonsils, several forms of angina are distinguished.
Catarrhal sore throat
A mild form, characterized by enlargement and redness of the tonsils, as well as the absence of purulent lesions. The child feels dry mouth, a whitish coating appears on the tongue, and the cervical lymph nodes are slightly enlarged. In addition to a sore throat that gets worse when swallowing, the child feels a sore and burning sensation. The temperature rises to 38 degrees, children complain of weakness and headache.
Follicular tonsillitis
A serious disease in which the tonsils become covered with purulent pinpoint follicles. On days 2-3, the ulcers open, leaving wounds that heal quickly. There is severe pain in the throat, radiating to the ear, making it difficult to swallow, children refuse to eat and drink. The lymph nodes are enlarged and painful when pressed lightly. Fever and chills are accompanied by a temperature of up to 40 degrees, vomiting, convulsions and fainting are possible.
Lacunar tonsillitis
In the lacunae, between the lobes of the tonsils, islands of yellow purulent plaque appear, which tend to unite into wide purulent foci. The symptoms are similar to those of purulent follicular tonsillitis, but are more pronounced and are accompanied by severe intoxication of the body. It hurts the child to turn his head, his mouth opens with difficulty, which makes speech slurred.
Viral (herpetic) sore throat
Most often, the development of the disease is facilitated by vitamin deficiency and weakened immunity. The tonsils become covered with red blisters, which burst, leaving small ulcers in their place. In addition to a sore throat, symptoms are acute respiratory in nature: cough, runny nose, abdominal pain, indigestion, as well as stomatitis and conjunctivitis. Lack of timely treatment of herpetic sore throat in children can lead to serous meningitis.
Fungal tonsillitis
A relatively mild form of sore throat that occurs in children under 3 years of age. It is distinguished by a coating of white, curdled flakes on the tonsils and, with proper treatment, goes away within a week.