Sometimes both men and women develop moles in the groin area. By their nature, nevi are benign formations and do not require removal. However, sometimes a growth in the groin causes inconvenience to the owner. In such cases, doctors recommend removing the nevus using one of the elimination methods.
Having a mole in the groin is not dangerous, but if they begin to grow or change, it would be a good idea to visit a doctor.
Moles in an intimate place. Danger, Risks, Complications.
Intimate moles (nevi) are not only a kind of decoration of the body, but also a risk zone. This is due to the possibility of their malignancy. Moles on the labia in women or on the genitals in men are small and almost invisible. But convex formations can cause concern, as well as cause inconvenience and even pain during sexual intercourse. The size of intimate moles and their color may vary. Sometimes they are small, but they can also grow into birthmarks. There are black, brown, red moles, as well as flat and convex. Moles in intimate places can be congenital or acquired. Congenital nevi occur in the first year of a child’s life. Acquired ones arise during human life under the influence of various factors. There is nothing dangerous about birthmarks on the genitals themselves. Unfortunately, the danger is posed by the fact that under the influence of certain factors, a mole can begin to change and turn into melanoma and cost a man or woman not only his health, but also his life.
What can be the consequences of a mole on the labia?
Moles on intimate places can pose a threat in terms of degeneration into oncology, so they are at risk for trauma.
When carrying out hygienic measures, during sex, when wearing tight underwear, there is always a risk of injuring the tumor.
If the nevus is damaged, bleeding develops, and if the injured area is not treated with an antiseptic, it can lead to the development of complications.
As a result of injury to a mole, bleeding may develop, so you should immediately try to stop the bleeding.
You will need a bandage or cotton wool, hydrogen peroxide or chlorhexidine.
If the nevus comes off, then an attempt must be made to preserve it by placing it in a 0.9% NaCL solution so that histological examination can be carried out.
After this, you should consult a doctor who will examine the affected area and, if the tumor has not completely come off, remove its remains.
The risk of nevus degeneration may be associated with prolonged exposure to ultraviolet radiation, as well as when trying to get rid of a mole on your own.
You should immediately consult a doctor if:
- The nevus began to itch. The doctor will examine you and find out the cause of the itching.
- if the shape and size of the tumor changes, the doctor will suggest removing it
- moles become inflamed, change color, groin lymph nodes bleed and are swollen, then the patient will be treated by an oncologist
With a single lesion of a nevus, if it is not malignant, the danger of degeneration is unlikely.
When melanoma is injured, fragments of melanin can enter the systemic circulation, causing skin cancer.
Reasons for the appearance of moles in intimate places in men:
If a man has a mole on the penis that has a convex shape or is located on a thin stalk (a hanging mole), it is necessary to get rid of the pigment as soon as possible. Its risk of injury can lead to degeneration from a benign to a malignant formation.
- Frequent visits to the solarium. Regular use of a solarium before the age of 35 increases the risk of melanoma, the most aggressive type of skin cancer, by 75%, the American Center for Disease Control and Prevention (CDC) reports on its official website;
- Constantly wearing underwear in the form of swimming trunks. Such underwear rubs and compresses the genitals, and constantly slightly injures the skin. For a man accustomed to these sensations, it may not be noticeable, but the skin suffers;
- Accidental injury to the skin on the penis or the head of the penis can lead to the formation of a nevus. Injuries or microtraumas can happen anywhere and for any reason: excessively harsh washing, unsuccessful sex, a sharply buttoned fly;
- Regularly being under stress or chronic diseases can trigger the appearance of moles in intimate places;
- Frequent visits to the radiologist or long stay in an area of increased radiation;
- Transitional age, during which hormonal imbalance occurs;
- The presence of viral or infectious diseases of the genital area.
How to distinguish it from other skin formations
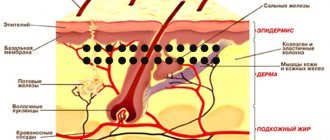
A mole between the legs is confused with papillomatosis; in the groin you can see a cluster of hanging warts, vaguely similar to nevi. Papillomas arise on the human dermis as a result of infection or increased activity of the dormant human papillomavirus. Small, flesh-colored growths begin to appear on the skin, which are easy to touch and tear off.
A mole differs from a papilloma in that it is brown, pink, black, blue or red in color, the surface is flat or slightly convex, the shape is regular, round, and the boundaries are clear. A dermatologist treats and examines nevi; it is better to show papilloma to a dermatovenerologist.
Ordinary neoplasms do not require treatment unless they are located in traumatic areas where they must be removed. Papillomas require complex treatment, removal, and pose a danger to the person on whose skin they are located.
A mole in the perineum differs from skin and venereal diseases according to the following characteristics:
- STDs and fungal diseases appear on the skin of the perineum in the form of papules, warts, lichen, ulcers, pustules, spots.
- A healthy mole does not bring discomfort to a person; skin manifestations of STDs and fungal infections itch, become inflamed, and break out.
- Skin and venereal diseases occur due to allergens, fungi, parasites or microbes. Moles appear during natural processes in the dermis.
Unpleasant sensations on the skin in the groin area, itching, tingling or tingling should be a reason to consult a doctor. If the symptoms are caused by an STD, they should be treated by a venereologist.
Reasons for the appearance of moles in a woman’s intimate places:
- Frequent trips to the solarium, prolonged exposure to direct sunlight. The WHO health organization equates solariums in terms of their harmfulness to cigarettes and alcohol. WHO has concluded that the risk of cancer from the use of tanning beds should be considered not “possible”, but “maximum”;
- Ultraviolet radiation - its excessive exposure promotes increased production of melanin, which provokes the appearance of nevi on different parts of the body or the growth of existing ones;
- Changes in hormonal levels - changes in hormone levels in women during puberty, when taking contraceptive medications or during pregnancy;
- Weakening of the general immune defense of the body (prolonged colds and infectious diseases, vitamin deficiency, congenital or acquired immunodeficiencies);
- Genetic predisposition - pigmented neoplasms are formed during the period of intrauterine development of the fetus;
- Neglect of basic hygiene rules, use of allergenic products for intimate hygiene;
- Diseases of the pancreas, gastrointestinal tract or liver also affect the appearance of skin tumors;
- Prolonged psycho-emotional tension, stress and shock;
- Infectious and inflammatory processes of the genital area;
- Metabolic disorders (in particular lipid metabolism);
- Congenital pathologies of skin pigmentation;
- Physiological characteristics of a woman’s body;
- Frequent and prolonged hypothermia;
- Pathologies of the cardiovascular system.
Moles on the labia or genitals in men must be distinguished from condylomas and warts, which can be a symptom of a sexually transmitted disease. Nevi that are regularly injured can provoke an oncological process. For example, convex or hanging growths cling to clothing or are injured during intimacy. In most cases, such pigmented formations are benign, but under the influence of a number of factors they can degenerate into melanoma. If a mole has sharply increased in size, its color or shape has changed, pain, cracks have appeared, or an inflammatory process has begun, then you need to consult an oncologist. In this case, surgical intervention is indicated to prevent their malignancy. For women, moles on the labia can cause huge problems, as they are easily damaged during shaving and hair removal: A mole on the labia, at first glance, is a highlight of a woman, but it can cause many problems and inconveniences. Such a formation does not always look aesthetically pleasing, but the most dangerous thing is that it can degenerate into a malignant tumor. All nevi must be monitored so as not to miss this process. A mole in an intimate place, especially if it is convex in shape, can cause considerable inconvenience and trouble to its owner. Many women are very worried about a mole on the labia or possible health complications associated with it, and are afraid of damaging it in some way.
What does this indicate?
Ancestors believed that the location of a dot or spot on a person’s body promised something good or negative on the path of life. In ancient times, people believed that if a person had a mark on the right side of his crotch, he would be rich and noble, but prone to disease. If the spot was located on the left, then the person will live in need, illnesses will haunt him.
Moleosophy – the science of moles – interprets marks in the groin as follows:
- A formation in the perineum characterizes a person as a capable person, but not always able to cope with emotions and desires.
- A mark in the groin indicates that its owner may have problems that do not have a solution.
- A spot in the groin of a man characterizes him as a passionate lover.
- Moles in the perineum in women indicate that the owner is experienced in love and love games.
People who have marks between their legs give birth to beautiful children.
When to see a doctor:
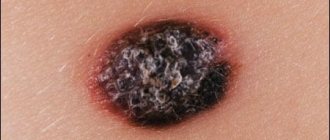
- Takes on a bright red or almost black color;
- Bleeds, peels, itches, cracks appear;
- Causes pain during sexual intercourse;
- It causes inconvenience and there is a risk of damage;
- It has uneven edges and an asymmetrical shape;
- A red rim appeared around the mole;
- Has dimensions greater than 6 mm;
- Increases in size.
Such moles require special attention and mandatory consultation with a doctor, regardless of whether they are located in the intimate area or on any other part of the body. According to research, it has become known that approximately 50% of intimate moles develop into melanoma. Therefore, every birthmark needs to be monitored.
Important! Melanoma is a malignant neoplasm. To treat melanoma, you need to see an oncologist. Modern medicine has developed ways to remove almost any mole. However, it is worth consulting with a doctor in advance, getting tested for tumor markers, and also doing a biopsy of the tumor to determine whether it is benign or malignant.
Mole removal methods:
Surgical removal of moles.
- Although surgical removal of formations is safe, it still has some disadvantages:
- After removing a mole, you need to avoid contact with ultraviolet radiation for a certain period of time;
- Long period of rehabilitation and healing of the wound after removal of the formation;
- The risk of noticeable scars and keloids appearing at the site of the former mole.
Cryodestruction.
- The inability to conduct a histological examination of the removed material, which increases the risk of not finding out about melanoma or skin cancer in time;
- The spread of liquid nitrogen is unpredictable; the nevus may not be completely removed, which means repeated removal will be required;
- It is difficult to predict the area of distribution of liquid nitrogen and there is a possibility of damage to healthy tissues by cold;
- This procedure is suitable for removing moles in visible places;
- This method is used mainly for small formations;
- The need for many repeated procedures;
- High risk of infection.
- The disadvantages of cryodestruction are quite significant, so before removal by this method, you should carefully weigh the pros and cons.
Electrocoagulation.
- the need to use local anesthesia, since the procedure is accompanied by pain; the need to treat the wound after surgery; the thermal effect extends to nearby areas of the skin;
- in some cases, a scar remains on the treated area; the possibility of an allergic reaction to local anesthesia;
- the need for repeated procedures;
- possibility of infection;
- allergic reaction to cold.
Radio wave removal of moles.
- when removing a large nevus, scar formation is possible;
- inability to remove large moles;
Laser removal of moles.
- The laser method of removing benign tumors is considered today the most painless, low-traumatic and effective method, which is popular all over the world.
- At the same time, the laser does not leave scars on the skin, and also eliminates pigmentation.
- There is no bleeding during or after the procedure.
- The effectiveness of the laser is due to the small diameter of its beam, high accuracy and the ability to fully control the depth of impact.
- After this procedure, the recovery process is very fast, due to the ability of the laser to stimulate the regeneration of skin cells.
- The only disadvantage of laser mole removal is the relatively high cost of removal.
Laser removal of intimate moles in the laser surgery room “LaserMedChisinau”! Today, the safest and most effective method of getting rid of unwanted moles is laser mole removal, during which layers of the mole are removed one by one. Anesthesia is usually not used. Thanks to the latest technologies, the highest precision in mole removal is achieved without damaging adjacent healthy tissue. The diameter of the laser beam can be adjusted with the highest precision, and it is also possible to select the optimal depth of exposure.
Preparation for laser removal of intimate moles in the laser surgery office “LaserMedChisinau”! Preparation for the procedure: no special preparation is required. It is not recommended to remove tumors (removal of moles, warts, papillomas, etc.)
- with photodermatosis – allergy to sunlight;
- women during menstruation;
- immunodeficiency states;
- oncological diseases;
- elevated temperature;
- inflammation of the skin;
- diabetes
- pregnancy;
- epilepsy;
- herpes;
- acne.
In the laser surgery office "LaserMedchisinau", the patient undergoes laser removal of moles only after a preliminary consultation with a licensed medical specialist - oncologist (for example: Doctor Victor Ciuperca, şeful secţiei Tumori Piele şi Melanom, IMSP Institutul Oncologic, Moldova or any licensed oncologist) with the issuance of an advisory opinion, which you must have with you. After consultation, a licensed medical specialist - oncologist issues an advisory opinion for the doctors of the medical institution at the patient’s place of residence.
Differential diagnosis of mole
The main task of a dermatologist when a patient comes to him is to correctly differentiate a mole from other growths.
To do this, the general condition of the skin is analyzed, including developmental defects, the number of moles and their types.
Difficulties in diagnosis are explained by the presence of a large number of known pathologies of the dermis that accumulate pigment.
A mole is differentiated from such neoplasms as fibroma, basal cell carcinoma, papilloma, condyloma, wart, etc.
Some types of nevi can mimic a tumor.
For example, congenital moles can be large in size and asymmetrical in shape.
They are also subject to degeneration.
Advantages of laser removal of moles in the laser surgery office “LaserMedChisinau”:
- Laser removal of skin defects, such as moles, is carried out using the most modern and high-tech laser equipment of the latest generation based on a CO2 laser;
- No relapses - moles no longer appear in the old place;
- Fast recovery and short rehabilitation period;
- The operation is painless, fast and without bleeding;
- Healthy tissue around the nevus remains intact;
- No noticeable scars or scars after surgery;
- You can remove several nevi at once in one session;
- Absence of various inflammatory processes;
- The operation is performed on an outpatient basis.
- Precise removal of the deepest part of the mole;
- Neighboring skin areas are not damaged.
Recommendations after removal of intimate moles:
- You will have to avoid sexual intercourse for at least 7 days, as there is a risk of bleeding;
- Under no circumstances should the crust at the site of the removed mole be torn off, nor should it be wetted or lubricated with cream, iodine, or brilliant green;
- Only those drugs prescribed by the doctor are used;
- You cannot visit the pool, sauna or sunbathe;
- It is necessary to wear only loose underwear and clothing so as not to rub the mole removal site;
- Fabrics must be natural.
In the laser surgery office “LaserMedchisinau”, the patient undergoes laser removal of moles only after a preliminary consultation with a licensed medical specialist - oncologist (for example: Doctor Victor Ciuperca, şeful secţiei Tumori Piele şi Melanom, IMSP Institutul Oncologic, Moldova or any licensed oncologist) with the issuance of an advisory opinion, which you must have with you. After consultation, a licensed medical specialist - oncologist issues an advisory opinion for the doctors of the medical institution at the patient’s place of residence.
Laser mole removal is not only an excellent aesthetic solution for getting rid of unwanted intimate moles, but also the prevention of malignant skin diseases.