Emla cream: composition and mechanism of action on the skin
Why does a person experience pain? In general, this feeling performs a kind of protective function in the body. When the skin is injured or otherwise damaged, the nerve endings immediately send an impulse to the brain about it. Thus, the biological meaning of pain is that it instantly mobilizes the body for self-preservation.
The epilation process is always accompanied by painful sensations
However, pain becomes a serious obstacle during some beauty procedures, in particular during hair removal or depilation, when hairs are removed, damaging the hair follicle, or pulled out along with the root. In this case, Emla cream is often used, which blocks the nerve endings, as a result of which the brain does not receive any alarm signals.
The drug contains the anesthetic components lidocaine and prilocaine. Lidocaine exhibits its analgesic properties much faster than prilocaine, but its duration of action is shorter than that of the second anesthetic.
The combination of these two components in Emla provides, although not instantaneous, a relatively quick and fairly long-lasting effect, which allows epilation or depilation over large areas of the skin.
Research shows that Emla is a highly effective drug. 91% of women noted complete pain relief after applying the cream. The remaining 9% experienced minor pain. This could be due to the use of an insufficient amount of the drug, or the exposure time was incorrectly chosen .
Another reason for inadequate anesthesia may be a physiological feature of the skin: the thicker the skin, the longer it takes the drug to reach the nerve endings. Therefore, in this case, the application time of Emla should be increased so that the components of the drug can penetrate the skin layers as deeply as possible.
Emla cream for local and external use 30g
Compound
Active ingredients: lidocaine 25 mg, prilocaine 25 mg.
Excipients: macrogol glyceryl hydroxystearate (Arlaton 289) - 19 mg, carbomer 974P (carboxypolymethylene) - 10 mg, sodium hydroxide - 5.2 mg (to bring the pH to 8.7-9.7), purified water - up to 1 g.
Pharmacokinetics
Systemic absorption of EMLA® cream depends on the dose, duration of application and thickness of the skin (depending on the body area), as well as other skin conditions such as skin diseases and shaving. When applied to the ulcerative surface of the lower extremities, the absorption of the drug may be influenced by the characteristics of the ulcers, for example, the size (with an increase in the area of the ulcer, absorption increases).
Intact skin:
In adults, after applying 60 g of cream to an area of 400 cm2 of intact thigh skin (1.5 g per 10 cm2) for 3 hours, systemic absorption for lidocaine was approximately 3% and for prilocaine 5%. Absorption is slow. The maximum concentration of lidocaine (average value 0.12 μg/ml) and prilocaine (average value 0.07 μg/ml) in blood plasma was reached approximately 4 hours after application of the cream. The risk of toxic symptoms exists only when the concentration of active substances in the blood plasma is 5-10 mcg/ml. When EMLA® cream is applied to intact skin 8-12 hours after shaving, the maximum plasma concentration of lidocaine and prilocaine in both young and elderly patients is very low and well below possible toxic levels.
Trophic ulcers of the lower extremities:
The time to reach the maximum concentration of lidocaine (0.05-0.84 mcg/ml) and prilocaine (0.02-0.08 mcg/ml) in the blood plasma is 1-2.5 hours from the moment the drug is applied to the ulcer surface (5 - 10 g of cream for 30 minutes). With repeated application of the cream to the ulcerative surface, there was no accumulation of prilocaine, lidocaine or their metabolites in the blood plasma. 2-10 g of EMLA® cream were applied to the ulcer surface with an area of up to 62 cm2 for 30-60 minutes from 3 to 7 times a week (15 times within a month).
Mucous membrane of the genital organs:
The time to reach the maximum concentration of lidocaine and prilocaine in the blood plasma (on average 0.18 mcg/ml and 0.15 mcg/ml, respectively) is approximately 35 minutes from the moment the drug is applied to the vaginal mucosa (10 g of cream for 10 minutes).
Indications for use
In adults:
- superficial anesthesia of the skin during punctures (including vaccinations), punctures and vascular catheterization and superficial surgical interventions, including minor cosmetic procedures and hair removal;
- superficial anesthesia of trophic ulcers of the lower extremities during surgical treatment (mechanical cleaning), for example, to remove fibrin, pus and necrotic tissue;
- superficial anesthesia of the mucous membrane of the genital organs before painful manipulations and for pain relief before injections of local anesthetics.
In children:
- superficial anesthesia of the skin during injections (including vaccinations), punctures and catheterization of blood vessels and superficial surgical interventions (including removal of molluscum contagiosum).
Contraindications
- Hypersensitivity to amide-type local anesthetics or any other component of the drug;
- premature newborns born at less than 37 weeks of gestation;
- newborns weighing less than 3 kg.
With caution: Glucose-6-phosphate dehydrogenase deficiency, hereditary or idiopathic methemoglobinemia, common neurodermatitis (atopic dermatitis), patients taking class III antiarrhythmic drugs (for example, amiodarone) (see section “Special Instructions”).
Directions for use and doses
Externally, on the skin or mucous membrane.
Adults
Superficial anesthesia of intact skin
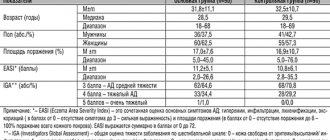
| Indication | Dose and method of application | Application time |
| When inserting a needle, for example when catheterizing blood vessels and taking blood samples | Apply half a 5 g tube (approximately 2 g) per 10 cm2 in a thick layer to the skin and cover with an occlusive dressing. | 1 hour, maximum 5 hours |
| For minor surgical procedures, such as curettage of molluscum contagiosum, removal of warts, minor cosmetic procedures and hair removal | Apply 1.5-2 g/10 cm2 in a thick layer to the skin and cover with an occlusive dressing | 1 hour, maximum 5 hours |
| On large areas of freshly shaved skin (on an outpatient basis), including before epilation | maximum recommended dose 60 g, maximum recommended application area 600 cm2; apply a thick layer to the skin and cover with an occlusive dressing | 1 hour, maximum 5 hours |
| For superficial procedures on large areas (in stationary conditions), for example, taking a rut using the split flap method | Apply 1.5-2 g/10 cm2 in a thick layer to the skin and cover with an occlusive dressing | 2 hours, maximum 5 hours |
Superficial anesthesia of trophic ulcers of the lower extremities:
For surgical treatment (mechanical cleaning) of trophic ulcers of the lower extremities: a single dose of about 1-2 g/10 cm2; Apply the cream in a thick layer to the ulcer surface, no more than 10 g of cream per procedure. Apply an occlusive dressing. Application time: minimum 30 min.
An opened tube of cream is intended for single use; the tube with any remaining cream should be discarded after use on one patient.
In the case of treating ulcers, into the tissues of which penetration of the drug is difficult, the duration of application can be increased to 60 minutes. Mechanical cleaning must begin no later than 10 minutes after removing the cream.
When manipulating ulcers of the lower extremities, EMLA® cream was used up to 15 times over 1-2 months without reducing the effectiveness and increasing the incidence of local reactions.
Superficial anesthesia of the genital organs:
Genital skin:
Pain relief before local anesthetic injections:
Men: 1 g/10 cm2. Apply the cream in a thick layer to the skin. Application time: 15 min.
Women: 1-2 g/10 cm2. Apply the cream in a thick layer to the skin. Application time: 60 min.
Superficial anesthesia of the genital mucosa:
When removing condylomas and for pain relief before injections of local anesthetics: approximately 5-10 g of cream, depending on the area of the treated surface. The cream should be applied to the entire surface of the mucous membrane, including the folds of the mucous membrane.
No occlusive dressing is required. Application time: 5-10 min. Carry out the procedure immediately after removing the cream.
Children
Anesthesia during needle insertion (including vaccination), curettage of molluscum contagiosum and other minor superficial surgical procedures.
Apply the cream in a thick layer to the skin and cover with an occlusive dressing. The dose should correspond to the surface being treated and should not exceed 1 g of cream per 10 cm.
| Age | Application area | Duration of application |
| 0-3 months | maximum 10 cm2 (total 1 g of cream) (maximum daily dose) | 1 hour (important: no more than 1 hour) |
| 3-12 months | maximum 20 cm2 (total 2 g cream) | 1 hour |
| 1-6 years | maximum 100 cm2 (total 10 g cream) | 1 hour, maximum 4 hours |
| 6-12 years | maximum 200 cm2 (total 20 g cream) | 1 hour, maximum 4 hours |
A 3.5 cm strip of EMLA® cream approximately corresponds to a dose of 1 g.
Increasing the application time reduces anesthesia. In children with atopic dermatitis, the application time should be reduced to 30 minutes.
Apply the cream in a thick layer to the skin and cover with an occlusive dressing.
Recommendations for applying the drug
- Pierce the protective membrane of the aluminum tube using the screw cap, squeeze out a sufficient amount of cream from the tube and apply to the site of the intended procedure. When anesthetizing the skin, it is possible to use occlusive stickers (5 x 5 g included in the package).
- a. Take one of the occlusion stickers and remove the central part. b. Separate the paper lining from the paper border on the back of the headband.
- When anesthetizing trophic ulcers of the lower extremities, use an occlusive PVC dressing.
- Cover the applied cream with a bandage so that the layer of cream underneath is thick and does not squeeze out from under the bandage. Gently smooth the edges of the bandage to avoid cream leakage.
- If using the occlusion sticker included in the package, remove the paper frame. The time of application of the drug can be recorded directly on the bandage.
- After the recommended time has passed, remove the bandage and any remaining cream from the surface.
Storage conditions
Store at temperatures below 30°C, out of the reach of children. Do not freeze.
Best before date
3 years. Do not use after the expiration date stated on the package.
special instructions
Patients with glucose-6-phosphate dehydrogenase deficiency or hereditary or idiopathic methemoglobinemia are more susceptible to drug-dependent methemoglobinemia.
The effectiveness of using the cream in newborns during the procedure of taking blood samples from the heel has not been established.
Caution should be exercised when applying EMLA® Cream around the eyes as the product causes eye irritation. Elimination of protective reflexes can cause irritation or damage to the cornea. If the cream gets into your eyes, immediately rinse your eyes with water or 0.9% sodium chloride solution and protect your eyes until protective reflexes are restored.
Caution must be exercised when applying the drug to the skin with atopic dermatitis; Application time should be reduced (15-30 minutes).
In children under 3 months of age, the safety and effectiveness of EMLA® cream was determined after a single dose. In such children, after applying the cream, a temporary increase in the level of methemoglobin in the blood was often observed, lasting up to 13 hours. However, the observed increase in blood methemoglobin levels is probably not clinically significant.
Patients taking class III antiarrhythmic drugs (for example, amiodarone) should be under constant monitoring and ECG monitoring, because Possible effect on cardiac activity.
EMLA® Cream should not be applied to a damaged eardrum or in other cases of possible penetration of the cream into the middle ear.
The cream should not be applied to open wounds.
Due to the lack of data on the absorption of the drug, it is not recommended to apply the cream to the genital mucosa in children.
Lidocaine and prilocaine in concentrations above 0.5-2% have bactericidal and antiviral properties. Due to
Therefore, it is recommended to take special care when applying the cream before subcutaneous administration of a live vaccine (for example, BCG).
Due to the lack of data, the combined use of EMLA® cream and drugs that cause methemoglobinemia is not recommended in children aged 0 to 12 months.
Description
Local anesthetic.
Pharmacodynamics
EMLA cream contains lidocaine and prilocaine, which are amide-type local anesthetics, as active ingredients.
Skin anesthesia is caused by the penetration of lidocaine and prilocaine into the layers of the epidermis and dermis. The degree of anesthesia depends on the dose of the drug and the duration of application. Intact skin
After applying EMLA® cream to intact skin for 1-2 hours, the duration of anesthesia after removing the occlusive dressing is 2 hours. There were no differences in efficacy (including time to achieve analgesic effect) and safety when applying the cream to intact skin between elderly (65-96 years) and younger patients.
Due to the effect of EMLA® cream on superficial vessels, temporary paleness or redness of the skin may occur. Similar reactions in patients with widespread neurodermatitis (atopic dermatitis) may occur faster, within 30-60 minutes after applying the cream, which indicates faster penetration of the cream through the skin.
For puncture biopsy (4 mm in diameter), the use of EMLA® cream provides adequate anesthesia of intact skin in 90% of patients 60 minutes after application of the cream when the needle is inserted to a depth of 2 mm and after 120 minutes when the needle is inserted to a depth of 3 mm. The effectiveness of EMLA® cream does not depend on skin color or pigmentation (skin types I-IV).
When using combined vaccines against infections such as measles, rubella, mumps, or intramuscular combined vaccines against diphtheria, whooping cough, tetanus, polio and infection caused by Haemophilius influenzae type B, as well as when vaccination against hepatitis B, the use of EMLA® cream is not affected the mean antibody titer, the rate of appearance or disappearance of specific antibodies in the blood serum, or the number of patients achieving a protective or positive antibody titer after immunization.
Mucous membrane of the genital organs
Anesthesia of the genital mucosa is achieved faster compared to anesthesia of intact skin due to faster absorption of the drug.
In women, 5-10 minutes after applying EMLA® cream to the mucous membrane of the genital organs, anesthesia sufficient to relieve pain caused by the use of an argon laser is achieved; The duration of anesthesia is 15-20 minutes (taking into account individual characteristics from 5 to 45 minutes).
Trophic ulcers of the lower extremities
After applying the cream when treating trophic ulcers of the lower extremities, the duration of pain relief is up to 4 hours. There was no negative effect of the drug on the healing process of ulcers or on bacterial flora.
Side effects
When applied to intact skin
Common (≥1%, <10%): Skin:
transient local reactions in the area of application of the drug, such as pallor, redness and swelling.
Uncommon (≥0.1%,<1%): Skin:
at the first moment after application there is a slight burning sensation, itching and a feeling of warmth (in the area where the drug is applied).
Rare (<0.1%): Common:
allergic reactions, in the most severe cases - anaphylactic shock. Methemoglobinemia and/or cyanosis. Reactions in the area of application of the drug, such as hemorrhagic rash or pinpoint hemorrhages, especially after prolonged application in children with atopic dermatitis or molluscum contagiosum. Irritation of the cornea due to accidental contact of the cream with the eyes.
When applied to trophic ulcers of the lower extremities
Common (≥1%, <10%): Skin:
transient local reactions in the area of application of the drug, such as pallor, redness and swelling; at the first moment after application there is a slight burning sensation, itching and a feeling of warmth (in the area where the drug is applied).
Uncommon (≥0.1%,<1%):
Skin: skin irritation (in the area where the drug is applied).
Frequent (>1%, <10%):
General: allergic reactions, in the most severe cases - anaphylactic shock.
Use during pregnancy and breastfeeding
Pregnancy.
There is insufficient data on the use of EMLA® cream in pregnant women. Animal studies did not reveal any direct or indirect negative effects of the drug on pregnancy, intrauterine development of the fetus, the process of childbirth or postnatal development. Lidocaine and prilocaine penetrate the placental barrier and can be absorbed into fetal tissues. No specific reproductive effects, such as increased incidence of malformations or other direct or indirect adverse effects on the fetus, have been reported.
Lactation.
Lidocaine and prilocaine are excreted in breast milk in quantities that do not pose a risk to the baby when the drug is used in therapeutic doses.
Interaction
In patients receiving drugs that induce the development of methemoglobinemia (for example, drugs containing a sulfo group), EMLA® cream may help increase the concentration of methemoglobin in the blood.
When treating with other local anesthetics and structurally similar drugs (including tocainide), the risk of increased systemic effects when using high doses of EMLA® cream should be taken into account.
No specific studies have been conducted to evaluate the interaction of lidocaine/prilocaine with class III antiarrhythmic drugs; caution should be exercised when using drugs together.
Pharmaceutical interaction: not detected.
Drugs that reduce the clearance of lidocaine (eg, cimetidine or beta-blockers) may cause potentially toxic plasma concentrations when repeated high doses of lidocaine are administered over an extended period of time. This interaction is not clinically significant during short-term therapy with lidocaine (eg, EMLA® cream) at recommended doses.
Overdose
If the recommended dosage regimen is followed, the development of signs of systemic toxicity is unlikely.
Symptoms of intoxication are likely to be the same as with other local anesthetics, such as central nervous system (CNS) stimulation and, in severe cases, CNS and cardiac depression. In rare cases, the development of clinically significant methemoglobinemia has been observed. Prilocaine in high doses can cause an increase in methemoglobin levels.
Superficial application of prilocaine 125 mg for 5 hours caused the development of moderate methemoglobinemia in a 3-month-old child. Superficial application of lidocaine at a dose of 8.6 - 17.2 mg/kg caused serious intoxication in newborns.
Treatment
Severe neurological symptoms (convulsions, depression of the central nervous system) require symptomatic treatment, including the prescription of anticonvulsants and, if necessary, artificial ventilation. In case of development of methemoglobinemia, the antidote is methylthioninium chloride (methylene blue).
Due to the slow systemic absorption of the drug, patients should be monitored for several hours after starting treatment for intoxication.
Impact on the ability to drive vehicles and operate machinery
Does not affect the ability to drive vehicles or operate equipment.
Use of the drug for hair removal/depilation
For many women, Emla cream has become a lifesaver when removing excess hair from the body, since there are areas where the skin is highly sensitive and the resulting painful sensations become unbearable.
Can the product be used in the bikini area?
The intimate area is one of the most difficult in terms of hair removal or depilation. The skin here is thin and delicate, and the hairs have a hard and dense structure, so their removal is fraught with some difficulties. To destroy the hair follicle during hair removal, it will take a slightly longer exposure to laser or photo radiation, which is painful for the skin. And pulling out a hair along with a dense root from sensitive skin during depilation is accompanied by sharp pain.
Emla cream is used in gynecology for anesthesia during local operations.
Therefore, Emla cream is used more often to treat the bikini area than for other areas of the body. At the same time, you should not be afraid that the product may get on the genital mucosa . The fact is that Emla is quite often used in gynecology as an anesthetic drug during local operations.
Emla release forms
The most common form of release of the product is cream. Many people mistakenly call it ointment or gel. Emla cream is available in tubes of 5 g. One package contains 5 tubes and 12 occlusive stickers for fixing the anesthetic application.
The package contains 5 tubes of Emla cream and 12 occlusive stickers
The effect of numbing the skin occurs within 0.5–1 hour after applying the cream and lasts up to 5 hours. The longer the product is on the skin, the greater the depth of penetration of its components. 1 hour after application, Emla cream will “freeze” the skin to a depth of 2 mm, and after 2 hours the skin surface will completely lose sensitivity at a depth of 3 mm.
The second form in which Emla can be found is a pain-relieving patch. The duration of application and the degree of pain relief are determined by the dosage of lidocaine and prilocaine in the patch. Typically, the analgesic effect occurs within 1–2 hours and lasts for 2 hours.
The patch takes effect within 1–2 hours
How to use cream and patch
Emla cream for pain relief is used as follows:
- The treated area of skin must be thoroughly cleaned of dirt and sebaceous secretions. Experts recommend steaming the skin surface, as this will allow the components of the drug to penetrate deeper through the open pores.
- Apply the cream to the skin in a thick layer so that the surface of the skin is not visible. The cream cannot be rubbed in, but only applied!
- An occlusive sticker is applied on top of the drug to achieve maximum analgesic effect. For convenience, you can write on the sticker the time it was fixed.
- After 30–60 minutes, the application is removed, and the remaining cream is removed with a dry cloth. The skin is ready for epilation or depilation.
When Emla cream is used correctly, the necessary anesthetic effect is achieved.
Attention! If there is a small amount of cream left in the tube, the tube with the remains of the drug cannot be saved until the next use! The product just needs to be thrown away.
Video: how to use Emla cream
The Emla patch is also applied to a clean, dry skin surface. Its wearing time exceeds the duration of application of the cream and is 60–120 minutes. After this, the patch is removed and you can begin the procedure for removing excess hair.
The use of Emla before hair removal and depilation has slight differences. Before epilation, the consumption of the drug and the duration of its effect are slightly increased compared to the depilation procedure.
For example, for laser or photoepilation of the intimate area, you will need 8–10 g of Emla cream (two tubes), and for depilation with wax, sugar paste or an epilator, you need to apply 3–5 g of the drug (one tube) to the skin. In addition, before epilation, the duration of application of the cream should be at least 1.5–2 hours, and the time of wearing the patch should be 2 hours. The time for “freezing” the skin before depilation is 30–40 minutes less.
Before sugaring, sensitive areas can be numbed with Emla
Emla 30g cream
pharmachologic effect
Local anesthetic.
Composition and release form Emla 30g cream
Cream:
- Active ingredients: lidocaine 25 mg, prilocaine 25 mg;
- Excipients: polyoxyl hydrogenated castor oil (Arlaton 289), carboxypolymethylene, sodium hydroxide to bring the pH to 8.7-9.7, purified water.
Cream for external and local use.
Description of the dosage form
Symptoms: central nervous system stimulation, convulsions, coma, methemoglobinemia (induced by prilocaine).
Treatment: pulmonary ventilation, maintenance of vital functions, symptomatic therapy; for methemoglobinemia - slow intravenous methylene blue solution, for convulsions - anticonvulsant therapy.
Directions for use and doses
Emla should be applied at least 1 hour before the start of the procedure.
For skin anesthesia, adults and children over 1 year old apply about 1.5 g/10 cm2.
Minor procedures (i.e. needle insertion and surgical debridement of small lesions) - 2 g for 1-5 hours manipulation on large surfaces (including skin grafting) - 1.5-2 g/10 cm2 for 2-5 h.
For children aged 3-12 months, apply up to 2 g of Emla cream to the surface of the skin with an area of no more than 16 cm2. Application time - 1 hour.
For anesthesia of the genital mucosa in adults during surgical treatment and removal of warts, apply 5-10 g of cream for 5-10 minutes (without a tight bandage) and immediately carry out the procedure.
Pharmacodynamics
A preparation for superficial anesthesia of the skin and mucous membranes. The effect of the drug is ensured by its constituent components - lidocaine and prilocaine, which are amide-type local anesthetics. Local anesthetics, penetrating into the layers of the epidermis and dermis, cause anesthesia of the skin.
The degree of anesthesia depends on the dose of the drug and the duration of application.
After applying the cream to intact skin for 1-2 hours, the duration of anesthesia after removing the occlusive dressing is 2 hours. During puncture biopsy, the use of Emla cream provides adequate anesthesia of intact skin in 90% of patients 60 minutes after application.
Anesthesia of the genital mucosa is achieved faster than that of intact skin due to faster absorption of the drug. In women, 5-10 minutes after applying Emla cream to the mucous membrane of the genital organs, anesthesia sufficient to relieve pain caused by the use of an argon laser is achieved; The duration of anesthesia is 15-20 minutes (taking into account individual characteristics from 5 to 45 minutes).
When treating trophic ulcers of the lower extremities, the duration of anesthesia after applying the cream is up to 4 hours. There is no negative effect of the drug on the healing process of ulcers or on bacterial flora.
Pharmacokinetics
Systemic absorption of the cream depends on the dose, duration of application and thickness of the skin (depending on the area of the body), as well as on other features of the skin.
In adults, after applying 60 g of cream to intact skin of the thigh with an area of 400 cm2 (0.2 g per 10 cm2) for 3 hours, systemic absorption of lidocaine is approximately 3%, prilocaine - 5%. Absorbed slowly. Cmax of lidocaine and prilocaine in blood plasma was achieved approximately 4 hours from the moment of application of the cream and was 0.12 μg/ml for lidocaine and 0.07 μg/ml for prilocaine.
In the treatment of trophic ulcers of the lower extremities, the time to reach Cmax of lidocaine (0.05-0.84 mcg/ml) and prilocaine (0.02-0.8 mcg/ml) in the blood plasma is 1-2.5 hours from the moment the drug is applied to the ulcer surface (5-10 g of cream per 30 min). With repeated application of the cream to the ulcerative surface, accumulation of prilocaine, lidocaine and their metabolites is not observed.
When applying the cream to the genital mucosa, the time to reach the Cmax of lidocaine and prilocaine (0.18 mcg/ml and 1.15 mcg/ml, respectively) is approximately 35 minutes from the moment the drug is applied to the vaginal mucosa (10 g of cream for 10 minutes).
Pharmacokinetics in special clinical situations
In patients with advanced neurodermatitis, the rate of absorption increases.
Indications for use Emla 30g cream
Methemoglobinemia; premature babies born at less than 37 weeks of gestation; hypersensitivity to amide-type local anesthetics or any other component of the drug.
Contraindications
Common to both dosage forms
- hypersensitivity to amide-type local anesthetics or any other component of the drug;
- premature newborns born at less than 37 weeks of gestation.
Extra for cream
- newborns weighing less than 3 kg.
Carefully
Cream: glucose-6-phosphate dehydrogenase deficiency, hereditary or idiopathic methemoglobinemia, common neurodermatitis (atopic dermatitis), patients taking class III antiarrhythmic drugs (eg, amiodarone).
Therapeutic system: when using the drug near the eyes; before subcutaneous administration of a live vaccine (for example, BCG); in case of application to the skin for widespread neurodermatitis (atopic dermatitis); The combined use of EMLA® and drugs that cause methemoglobinemia in children aged 0 to 12 months is not recommended; in patients with glucose-6-phosphate dehydrogenase deficiency; It is not recommended to apply the drug to open wounds.
Use of Emla 30g cream during pregnancy and breastfeeding
Emla should not be used in children under three months of age.
special instructions
Emla should be used with caution in patients with atopic dermatitis.
In this category of patients, a shorter application period (15-30 minutes) is used due to the faster absorption of Emla.
Overdose
Local reactions: often (>1%) - pallor, hyperemia and swelling at the site of application of the drug (due to the effect on superficial vessels); sometimes (0.1%) - slight burning and itching immediately after applying the drug; rarely (
Systemic reactions: rarely (
Side effects of Emla 30g cream
Superficial anesthesia: skin during punctures and catheterization of blood vessels and superficial surgical interventions; trophic ulcers of the lower extremities during surgical treatment (mechanical cleaning); mucous membrane of the genital organs before painful manipulations and for pain relief before injections of local anesthetics.
Contraindications and possible side effects
A distinctive feature of Emla is a small list of contraindications for its use:
- increased sensitivity of the body to the main analgesic components;
- some blood diseases (methemoglobinemia);
- taking sulfonamides;
- period of bearing a child (relative contraindication);
- damage to the skin in the form of wounds and scratches;
- individual intolerance.
Sometimes after using Emla, side effects may occur:
- pallor or redness of the skin at the site of application of the product;
- itching or burning;
- swelling of tissues;
- rashes.
An overdose of the drug may cause unpleasant consequences in the form of:
- overexcitability of the nervous system;
- weakness in muscle tissue;
- disturbances in the functioning of the respiratory and cardiovascular systems (difficulty breathing, rapid heartbeat);
- general weakness.
Advantages and disadvantages
Consumers appreciated Emla and noted its following advantages:
- effective skin pain relief before epilation/depilation;
- Possibility of use in the intimate area;
- no odor;
- good consistency of the product, which does not allow the cream to spread after application;
- easy and convenient use;
- a small list of contraindications;
- the ability to purchase tubes individually, which saves money.
However, consumers also discovered disadvantages:
- the need to wait until the components of the drug begin to act;
- the likelihood of side effects;
- high price of the drug.
Precautionary measures
To ensure that the hair removal or depilation process is painless and that no side effects occur after using Emla, certain precautions must be observed.
When applying an anesthetic to the skin of the face, you need to ensure that the cream does not get on the mucous membrane of the eyes, since Emla causes irritation of the cornea. If accidental contact with the drug does occur, the eyes should be thoroughly rinsed with running water.
The use of cream for anesthesia of the upper lip should also be careful, since getting the product into the oral cavity is undesirable.
To avoid any unpleasant moments when using Emla before hair removal or depilation, experts advise studying the instructions for the drug and strictly following the instructions.
Analogues of the product
One of the disadvantages of Emla cream, consumers note its rather high cost: 350–370 rubles. for one tube. Because of this, many women cannot afford to purchase this product and are looking for more affordable drugs.
Cream Acriol Pro
The composition of Acriol Pro is identical to the composition of Emla: it also contains lidocaine and prilocaine. In addition, the use of the drug, the list of contraindications, possible consequences and side effects are the same as for Emla cream. The difference between the products is only in cost: a 5 ml tube of Acrylic Pro costs 200–220 rubles.
Acriol Pro contains lidocaine and prilocaine
Light Dep
Cosmetologists often resort to using Light Dep cream before hair removal/depilation. This product is distinguished by the fact that it contains the component epinephrine, which prevents irritation, redness and swelling.
The anesthetic effect of the drug appears within 15–20 minutes after application and lasts 4 hours. However, Light Dep cream is not intended for pain relief in the deep bikini area.
The cost of a 15 ml tube of Light Dep is 750 rubles.
LightDep cream does not cause irritation
Menovazin ointment
Menovazin contains:
- menthol, which has anesthetic and anti-inflammatory effects;
- novocaine, which blocks nerve endings;
- anesthesin that reduces pain.
The ointment begins to act within 10 minutes after application, and the “freezing” effect lasts 1.5 hours.
Menovazin costs only 30–60 rubles.
Menovazine can be used to anesthetize the deep bikini area
DeepNumb tool
The anesthetic effect of the drug is achieved due to the content of lidocaine, tetracaine and epinephrine. The cream is applied to the skin in a layer 2 mm thick. The effect of the product appears after 60 minutes and lasts 4 hours.
DeepNumb cream is available in 10 g tubes. One tube costs 350 rubles.
The anesthetic effect occurs after 60 minutes. after applying DeepNumb
Anesthesia EMLA® (EMLA)
Full description
Pharmacological action:
Emla is a local anesthetic drug in the form of a cream. Emla contains lidocaine and prilocaine - medicinal substances of the amide-type local anesthetic group. Skin anesthesia occurs due to the penetration of the active components of Emla cream into the deep layers of the epidermis and dermis. The degree of local anesthesia when using Emla cream depends on the time of application and the dose of lidocaine and prilocaine. When Emla is applied to intact areas of the skin for 60-120 minutes, the local anesthetic effect lasts for 2 hours after removing the occlusive dressing. There are no changes in the systemic absorption and tolerability of Emla in young and elderly patients (provided the cream is applied to intact skin). Considering the influence of the active components on the blood vessels of the skin, the development of hyperemia or pallor of the skin is possible. 60 minutes after applying the cream, sufficient anesthesia is achieved for puncture with a needle inserted to a depth of 2 mm, after 120 minutes - for puncture with a needle inserted to a depth of 3 mm. It is allowed to use Emla cream for anesthesia before vaccination with drugs intended for intramuscular or subcutaneous administration. The drug Emla does not slow down the healing of wounds and trophic ulcers, and also does not affect the bacterial microflora (in therapeutic doses). Systemic absorption of the active components of Emla depends on the dose, location and area of application of the cream.
When applied to intact skin, systemic absorption of lidocaine and prilocaine was 3% and 5%, respectively. Percutaneous absorption is slow, with peak plasma concentrations of local anesthetics observed 4 hours after topical application. When treating trophic ulcers, the peak fiery concentration of lidocaine and prilocaine was observed after 1.5-2 hours. When applied to the mucous membrane of the genital organs, the peak plasma concentration of the active components of Emla was reached within 30 minutes. Lidocaine and prilocaine do not accumulate in the body.
Indications for use:
Emla cream is used for superficial anesthesia of the skin during punctures, superficial surgical interventions, as well as vascular catheterization. Emla cream can be prescribed to reduce pain during mechanical cleaning of trophic ulcers of the extremities. Emla can also be prescribed for superficial anesthesia of the mucous membranes of the genital organs in preparation for painful manipulations.
Mode of application:
Emla cream is intended for topical use on the skin and mucous membranes. It is forbidden to apply Emla cream to areas with damaged skin, to areas of the skin around the eyes. Emla cream should not be used in otolaryngological practice if there is a risk of the drug getting into the middle ear. The duration of application and dose of Emla is determined by the doctor. For adults, when inserting needles or performing minor superficial operations (for example, removing warts), a thick layer of Emla cream is usually prescribed under an occlusive dressing. The recommended duration of application is 60 minutes.
Adults undergoing superficial surgical interventions on large areas are usually prescribed the application of a thick layer of Emla cream under an occlusive dressing. The recommended duration of application is 2 hours. The maximum application time for adults is 5 hours. For trophic ulcers of the lower extremities, before mechanical cleaning, as a rule, the application of 1-2 g of Emla cream per 10 cm2 of skin is prescribed. After applying the cream, the skin area is covered with an occlusive dressing. The recommended application time is 30 minutes. If absorption of the cream is difficult, the application time is extended to 60 minutes. For superficial anesthesia of the genital skin, it is usually recommended to apply 1-2 g of Emla cream. Application time for men is 15 minutes, for women 60 minutes.
For anesthesia of the mucous membrane of the genital organs (including when removing condylomas), as a rule, the application of 5-10 g of Emla cream is prescribed, depending on the area being treated. Emla cream should also be applied to the folds of the mucous membrane. The recommended application time is 5-10 minutes. For children, the amount of cream is determined depending on the age and area of the treated area. The maximum recommended dose is 1 g of cream per 10 cm2. The maximum duration of application for children under 1 year is 60 minutes, for children over 1 year – from 2 to 5 hours. The maximum duration of application for children with atopic dermatitis is 30 minutes.
Side effects:
Emla cream, as a rule, did not cause unwanted effects in patients. However, during clinical studies, isolated cases of adverse reactions caused by lidocaine and prilocaine were recorded. In particular, one cannot exclude the development of local undesirable effects in the form of hyperemia or pallor of the skin, itching, irritation and swelling of the skin at the site of application of the cream. In addition, it is possible to develop allergic reactions when using Emla cream, including urticaria, angioedema and anaphylactic shock.
Mainly in children or when using high doses of Emla, methemoglobinemia may develop. There is evidence of isolated cases of the development of hemorrhagic rashes and pinpoint hemorrhages when using Emla cream. The risk of developing these unwanted effects is higher in children with atopic dermatitis or warts. If Emla accidentally gets into the eyes, corneal lesions may develop.
Contraindications:
Emla is not prescribed to patients with hypersensitivity to prilocaine, lidocaine and other amide-type local anesthetics, as well as additional components of the cream. The use of Emla cream in premature newborns (who were born before the full 37 weeks of pregnancy) is prohibited. Emla should not be prescribed to children under 12 months of age who are receiving medications that can increase the formation of methemoglobin. Particular care should be taken when prescribing Emla cream to patients suffering from idiopathic or congenital methemoglobinemia, as well as glucose-6-phosphate dehydrogenase deficiency.
Emla is prescribed with caution to patients with atopic dermatitis (such patients should reduce the application time). Caution should be exercised when prescribing Emla cream to children under 1 year of age (due to the high risk of developing methemoglobinemia). It is necessary to carefully monitor the results of vaccination with a live vaccine when using the drug Emla (lidocaine and prilocaine in concentrations of more than 0.5-2.0% have an antiviral and bactericidal effect). Emla should be used with caution in patients with cardiac arrhythmias receiving class III antiarrhythmic drugs.
Pregnancy:
There is insufficient data from clinical studies of Emla in pregnant women. It is known that lidocaine and prilocaine penetrate the blood-placental barrier. Prescribing Emla cream to pregnant women is allowed only after a thorough assessment by a doctor of the risks and benefits. Some concentrations of lidocaine and prilocaine are detected in breast milk. Emla cream should not be used while breastfeeding.
Interaction with other drugs:
In patients receiving sulfonamides and other drugs that induce the formation of methemoglobin, there is an increased risk of developing methemoglobinemia when using Emla. There is an increased risk of additive systemic effects when Emla cream is used in combination with other local anesthetics and drugs with a similar chemical structure (for example, tocainide). Emla should be used with caution in patients receiving class 3 antiarrhythmic drugs.
Overdose:
If you follow the instructions presented in the annotation, the development of an overdose of Emla is unlikely. When using high doses of Emla cream, applying the drug to large areas of the skin or areas of the skin with compromised integrity, systemic intoxication with lidocaine and prilocaine may develop. In case of overdose, patients experience the development of excitation of the central nervous system; with a further increase in the dose, depression of the central nervous system and cardiac activity is possible. When intoxicated with prilocaine in patients, mainly children, the development of methemoglobinemia is possible (when 125 mg of prilocaine was applied for 5 hours, clinically significant methemoglobinemia developed in children). In addition, with an overdose of local anesthetics, seizures may develop.
A specific antidote is not known. If neurological symptoms of overdose develop, appropriate therapy is administered. For methemoglobinemia, methylthionine is prescribed. The patient's condition should be monitored and, if necessary, anticonvulsant therapy and artificial ventilation should be provided. Given the duration of systemic absorption of lidocaine and prilocaine after applying Emla cream, the patient's condition should be monitored for at least 2 hours after overdose therapy.
Release form:
Cream for external use Emla 5 g in tubes, package contains 5 tubes of cream complete with 12 occlusive stickers.
Storage conditions:
Emla cream must be stored in its original packaging at a temperature not exceeding 30 degrees Celsius. The shelf life of Emla cream is 3 years. After opening the tube, the cream should not be stored; unused remains should be disposed of.
Compound:
1 g of cream for external use Emla contains: Lidocaine – 25 mg; Prilocaine – 25 mg; Additional ingredients.
Pharmacological group:
Painkillers and anti-inflammatory drugs Local anesthetic drugs
Attention!
The description of the drug “Emla (cream)” on this page is a simplified and expanded version of the official instructions for use. Before purchasing or using the drug, you should consult your doctor and read the instructions approved by the manufacturer. Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.