Clotrimazole cream for external use 1% tube 20 g (GlaxoSmithkline)
Registration Certificate Holder
GlaxoSmithKline Trading (Russia)
Dosage form
Medicine - Clotrimazole
Description
Cream for external use 1%
in the form of a homogeneous white mass.
100 g
clotrimazole 1 g
Excipients
: benzyl alcohol - 1 g, cetostearyl alcohol - 11.5 g, octyldodecanol - 10 g, polysorbate 60 - 1.5 g, sorbitan stearate - 2 g, synthetic spermaceti - 3 g, water - 71 g.
20 g - aluminum tubes (1) - cardboard packs.
Indications
For external treatment of fungal skin diseases caused by dermatophytes, yeast-like fungi, molds, as well as pathogens sensitive to clotrimazole:
- mycoses of the feet, hands, torso, skin folds;
- candidal vulvitis, candidal balanitis;
- lichen versicolor, erythrasma;
- fungal infections of the outer ear.
Contraindications for use
- hypersensitivity to clotrimazole or other components of the drug.
pharmachologic effect
Clotrimazole inhibits the growth and division of microorganisms and, depending on the concentration, can have a fungistatic (delaying and stopping the growth of fungal cells) or fungicidal (leading to the death of fungi) effect. Clotrimazole inhibits the synthesis of ergosterol and binds to phospholipids of the fungal cell membrane, which leads to a change in the permeability of cell membranes.
At higher concentrations, clotrimazole causes damage to cell membranes by mechanisms independent of sterol synthesis.
Clotrimazole also disrupts the vital processes in the fungal cell, suppressing the formation of components necessary for the construction of vital cellular structures (proteins, fats, DNA, polysaccharides), damages nucleic acids and increases the excretion of potassium.
Ultimately, the effect of clotrimazole on fungal cells leads to their death.
Clotrimazole is characterized by a wide spectrum of antifungal and antibacterial activity:
dermatophytes (Epidermophyton floccosum, Microsporum canis, Trichophyton mentagrophytes, Trichophyton rubrum), yeast (Candida spp., Cryptococcus neoformans), dimorphic fungi (Coccidioides immitis, Histoplasma capsulatum, Paracoccidioides brasiliensis), protozoa (Trichomonas vaginalis).
He is also active in relation to
some gram-positive bacteria.
When studying the effectiveness of clotrimazole in laboratory conditions outside the human body (in vitro), a wide range of its fungistatic and fungicidal activity was revealed. It acts on the mycelium of dermatophytes (Trichophyton, Microsporum, Epidermophyton) in a similar way to griseofulvin, and its effect on budding fungi (Candida) is similar to the effect of polyenes (amphotericin B and nystatin).
At concentrations less than 1 mcg/ml, clotrimazole inhibits the development of most strains of pathogenic fungi belonging to Trichophyton rubrum, Trichophyton mentagrophytes, Epidermophyton floccosum, Microsporum canis.
At a concentration of 3 μg/ml, clotrimazole inhibits the development of most other bacteria: Pityrosporum orbiculare, Aspergillus fumigatus, the genus Candida, incl. Candida albicans, some strains of Staphylococcus aureus, Streptococcus pyogenes, as well as some strains of Proteus vulgaris and Salmonella. Clotrimazole is active against Sporothrix, Cryptococcus, Cephalosporium, Fusarium.
At concentrations greater than 100 μg/ml, it is effective against Trichomonas vaginalis.
Fungi resistant to clotrimazole are extremely rare; There is data only on individual strains of Candida guilliermondii.
The development of resistance in clotrimazole-sensitive fungi following passage of Candida albicans and Trichophyton mentagrophytes has not been reported. There have been no cases of the development of resistance to clotrimazole in Candida albicans strains resistant to polyene antibiotics due to a chemical mutation.
Drug interactions
Not studied.
Dosage regimen
For external use. The cream should be applied to the affected areas of the skin 2-3 times a day.
To prevent relapses
Treatment should be continued for at least two weeks after all symptoms of infection have disappeared.
The cream should be applied to clean, dry areas of affected skin (washed with neutral pH soap), and on the feet the cream should be applied between the toes.
The duration of treatment depends on the severity of the disease, its location, and the effectiveness of treatment.
Duration of treatment: ringworm - 3-4 weeks; erythrasma - 2-4 weeks; pityriasis versicolor - 1-3 weeks; candidal vulvitis and balanitis - 1-2 weeks.
The duration of treatment may vary according to individual characteristics, but a treatment duration of less than 3 weeks is not recommended. To prevent recurrence of infection, use of the drug should be continued for 1-2 weeks after all symptoms of the disease disappear. If after 7 days of treatment there is no improvement in symptoms, you should consult your doctor.
Overdose
Symptoms:
If the drug is accidentally taken orally, dizziness, nausea, and vomiting may occur.
Treatment:
In case of accidental ingestion of the cream, symptomatic treatment should be carried out. When using the drug externally, an overdose is unlikely.
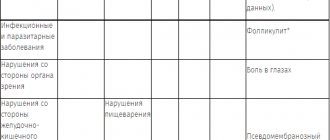
Side effect
The adverse events presented below are listed according to the damage to organs and organ systems and the frequency of occurrence.
The frequency of occurrence is defined as follows: very common (≥1/10), common (≥1/100 and <1/10), uncommon (≥1/1000 and <1/100), rare (≥1/10,000 and < 1/1,000), very rare (< 1/10,000, including isolated cases), unknown (frequency cannot be estimated from currently available data). Frequency categories were formed based on post-marketing surveillance. From the immune system:
unknown - allergic reaction (manifested by urticaria, fainting, arterial hypotension, shortness of breath).
For the skin and subcutaneous tissues:
unknown - rash, itching, blistering rashes, peeling, pain or discomfort, swelling, burning, irritation.
special instructions
Avoid contact of the cream with the mucous membrane of the eyes. Do not swallow.
All infected areas should be treated at the same time.
The drug Clotrimazole contains cetostearyl alcohol, which can cause local skin reactions (for example, contact dermatitis).
If symptoms of hypersensitivity or irritation appear, stop treatment.
Laboratory data indicate that the use of latex-containing contraceptives may cause contraceptive damage when used concomitantly with clotrimazole.
Consequently, the effectiveness of such contraceptives may be reduced. Patients should be advised to use alternative methods of contraception for at least 5 days after using clotrimazole. Effect on the ability to drive vehicles and operate machinery.
The effect of clotrimazole on the ability to drive vehicles and operate machinery has not been reported.
Storage conditions
The drug should be kept out of the reach of children at a temperature not exceeding 25 °C. Do not freeze.
Best before date
Shelf life: 3 years.
Use during pregnancy and breastfeeding
Restrictions during pregnancy - With caution. Restrictions when breastfeeding - With caution.
The use of Clotrimazole during pregnancy is allowed only if, in the opinion of the doctor, the potential benefit of using the cream for the mother outweighs the possible risk to the fetus.
Epidemiological studies have not revealed any adverse events related to pregnancy or fetal health when using the drug Clotrimazole.
The use of the drug Clotrimazole in women during breastfeeding is allowed only if, in the opinion of the doctor, the potential benefit of using the cream for the mother outweighs the possible risk for the child.
Fertility
No data available.
Terms of sale
The drug is available without a prescription.
Contacts for inquiries
GlaxoSmithKline Trading JSC (Russia)
125167 Moscow Leningradsky Prospekt, 37a, bldg. 4 BC "Arcus III" Tel. Fax
Clotrimazole
Over the past few decades, the problem of fungal diseases has become particularly relevant. This is largely due to the progression of immune disorders, which leads to an increase in the incidence of mycoses and a more severe course of the pathological process. One of the drugs that helps solve this problem is Clotrimazole. According to its chemical structure, it belongs to imidazole derivatives and has a wide range of antifungal effects. The fungicidal properties of the drug are due to its ability to disrupt the formation of one of the key elements of the cell wall of the parasitic fungus - ergosterol, which provokes a change in the morphology and properties of the cell, and ultimately causes its death (lysis). The ability to be fungistatic (inhibit the growth and development of parasitic fungi) or fungicidal (destroy them) is determined by the concentration of Clotrimazole in vitro: in the first case, from 1 μg/ml to 10 μg/ml of the active substance is sufficient. At a higher dose, the drug has a fungicidal effect against most known types of fungi. For candidiasis, Clotrimazole exhibits a fungicidal effect starting at 2 μg/ml. Sensitivity to Clotrimazole has been noted in dermatophytes, molds, yeasts (including “red” yeast, candida), in the causative agents of pityriasis versicolor and erythrasma. In addition, the drug exhibits an antibacterial effect against the most common opportunistic gram-positive microorganisms (staphylococci, streptococci), certain genera of gram-negative bacteria (gardnerella, bacterioides), as well as Corynebacterium minussimum, Malazessia furfur and Trichomonas vaginalis.
Due to poor absorption through the skin and mucous membranes, the drug does not have a systemic effect and associated side effects.
Clotrimazole is available in several dosage forms: vaginal cream, suppositories and tablets, cream and ointment for external use. In domestic pharmacies, the drug with the trade name “Clotrimazole” in the form of branded generics and generics can be found from several manufacturers at once, including Russian (Atoll, Avexima, GlaxoSmithKline Trading, ZiO-Zdorovye, Sintez, Ozon, Akrikhin) and foreign pharmaceutical companies: Esparma (Germany), Hyperion (Romania), Farmaprim (Moldova), Sedate Helcare (India), Medana Pharma (Poland), Teva (Israel), Shreya (India). Considering the lack of absorption through the skin and, therefore, systemic (not only locally, but also on remote organs and tissues) action, the use of Clotrimazole in high doses is not associated with life-threatening reactions. Poisoning by the drug is possible only through inappropriate (in this case, oral) use. Symptoms of toxicosis caused by Clotrimazole are nausea, vomiting, epigastric pain, anorexia, liver dysfunction, dermatological reactions, polyuria. In such a situation, the use of activated carbon is indicated.
Vacation conditions
Dispensed without a doctor's prescription.
More information about fungal infection:
Fungal infections are very common and affect many people.
Some of the most common fungal skin infections are athlete's foot, fungal diaper rash, fungal skin rash, and dermatophytosis.
There are two main types of fungal infections:
- Dermatophytosis caused by pathogens of the genus Tinea
- Candidiasis caused by yeast-like fungi of the genus Candida.
Dermatophytosis of the genus Tinea includes athlete's foot and ringworm. The causative agents of athlete's foot, as a rule, coexist without risk on our skin and in our environment. The natural balance, which is usually kept under control, can be disrupted by factors such as excess moisture (dampness). This can be observed, for example, when regularly wearing sneakers, in which the feet constantly sweat and are warm. Since this pathogen is contagious and can be infected by changing rooms. Ringworm can be transmitted from animals to children.
The main symptom of both types of dermatophytosis is itching, peeling and rash.
Pathogens of the genus Candida cause fungal skin rashes and thrush. Yeast rashes can develop anywhere on the body, but most often occur where areas of skin rub against each other, such as under the breasts, under the arms, in the groin area and on the back.
Candida is a yeast-like fungus that usually lives harmlessly on our skin. However, the normal balance, which is usually kept under control, can be disrupted by factors such as excessive sweating, tight or synthetic clothing, hygiene products, and bath additives. When the growth of fungi on the skin increases, the following symptoms may develop on it: constant burning and itching, soreness and various spots or plaques, as well as the phenomena of diaper rash and maceration.
Fungi of the genus Candida can cause the development of heat rash in children.
Most children experience heat rash at some stage. Although heat rash is rarely serious, it can be very distressing for you and your baby. Miliaria that lasts more than three days may be fungal in origin and require antifungal treatment. Symptoms of fungal prickly heat: red spots on the buttocks and genitals in children, burning and itching.