Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment and hardware correction
Post-inflammatory dyschromia (post-inflammatory hyperpigmentation, post-inflammatory hypopigmentation) are acquired pigmentation disorders that arise due to the tendency of melanocytes to excessive or insufficient pigment synthesis, as well as due to the accumulation of pathological pigment in the skin (for example, lipofuscin during aging).
In our company you can purchase the following equipment for the treatment of post-inflammatory dyschromia:
- M22 (Lumenis)
- Fraxel (Solta Medical)
Post-inflammatory hyperpigmentation is one of the most common dermatological conditions that develops more often on dark skin. One study found that acne pigmentation occurs in 65.3% of African Americans, 52.7% of Hispanics, and 47.4% of Asians. It can occur at any age and affects both women and men equally.
As for hypopigmentation , in one study involving 423 healthy people, 20 (4.7%) had at least one area of skin lightening. Local discoloration is especially noticeable on dark skin phototypes due to the contrast with surrounding healthy tissue.
What can modern cosmetology offer?
Photodamage, photoaging, and pigmentation have been shown to be closely related. And this fact should be taken into account when choosing cosmetic procedures - it is necessary not only to remove external manifestations (actually unpleasant areas of darkened skin), but also to act deeper, preventing the initiation of deep destructive aging processes in the dermis.
Treatment algorithm for hyperpigmentation
- After assessing the severity of pigmentation, the cosmetologist can offer several correction options.
- For selected lesions or as protection: combination of topical agents with a high SPF sunscreen.
- For moderate pigmentation: external chemical peeling, non-ablative low-intensity laser.
- For intense pigmentation: fractionated radiofrequency, Q-laser or picosecond laser, non-ablative high-intensity laser, microneedling, IPL system.
Etiology and pathogenesis
Post-inflammatory dyschromia can occur after infections, allergic reactions, mechanical damage to the skin, reactions to drugs, phototoxic dermatitis, burns and inflammatory diseases (systemic lupus erythematosus, atopic dermatitis, etc.), as well as with long-term use of hydroquinone or chemical peels. The condition of the lesions can be aggravated by ultraviolet radiation, various chemicals and drugs - tetracyclines, doxorubicin, bleomycin and 5-fluorouracil (cytostatics), clofazimine (anti-tuberculosis drug), silver, gold, antimalarial drugs, hormones.
It is interesting that different people, under the influence of the same factors, can develop both hyper- and hypopigmentation - some experts associate this with the severity of the inflammatory process in each specific case. However, there is a deeper theory called individual chromatic tendency . It is based on the proposition that each person can have “strong” and “weak” melanocytes, the number and type of which are inherited. “Strong” melanocytes react to any external influence by producing excess pigment, which is expressed by hyperchromia, while “weak” melanocytes practically stop synthesizing pigment, which creates hypochromic areas of the skin. At the same time, “weak” (labile) melanocytes are subject to destruction, so the inflammatory process can simply destroy them, as a result of which some areas of the face and body will become much lighter than the surrounding skin.
As for post-inflammatory hyperpigmentation , one of the pathogenetic mechanisms of its development is an excess of squalene on the skin due to hyperproduction of sebum by the sebaceous glands. Ultraviolet radiation entering the skin generates singlet oxygen in the skin, which, under the influence of squalene, is converted into squalene peroxide. In turn, it stimulates the production of prostaglandin E2, which triggers melanogenesis. Excessive amounts of sebum are produced, for example, during acne - accordingly, with this disease, the content of squalene in surface lipids is increased. In addition, in inflammatory foci, oxidation processes are especially active, so post-inflammatory hyperpigmentation may occur after acne.
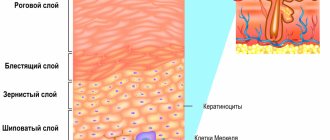
Mostly post-inflammatory hyperpigmentation is localized in the epidermis (brown pigmentation), but sometimes the pigment can be captured by macrophages and transferred to the dermis - in this case, the skin area becomes grayish-blue in color. Dermal pigmentation can last for many years or even last a lifetime.
Why is the sun dangerous?
Melanogenesis is triggered by the synthesis of melanin from amino acids such as L-phenylalanine and L-tyrosine with the involvement of many enzymes (the most basic is tyrosinase). The level of pigmentation largely depends on the activity of melanocyte cells and their number (Lerner, Fitzpatrick 1950).
Melanin production has a protective function in the skin and serves as a shield against solar radiation that leads to photodamage. Photodamaged skin responds by thickening the epidermis and increasing melanin production. This is how the body tries to protect the skin from ultraviolet radiation, and it is not surprising that after active recreation, cosmetology clinics are filled with patients with this problem (Gonzaga 2009).
From the point of view of phototoxicity, the most dangerous is the UVA spectrum (320–400 nm), the rays penetrate deep into the layers of the hypodermis and destroy collagen and elastin. The UVB spectrum (280–320 nm) mainly affects the outer layer of the skin - the epidermis. But when combined, both spectrums cause burns and mutagenic effects, including pigmentation.
Clinical manifestations
Various dermatological diseases and conditions with possible outcomes in hyper- or hypopigmentation are presented in table. 1 .
Table 1. Possible outcomes of dermatological diseases and skin conditions
| Disease/Condition | Hyperpigmentation | Hypopigmentation |
| Infections | ||
| Impetigo | + | + |
| Syphilis | – | + |
| Leprosy | – | + |
| Herpes simplex | + | + |
| Chicken pox | + | + |
| Allergic or immunological conditions | ||
| Insect bites | + | + |
| Atopic dermatitis | + | + |
| lupus erythematosus | + | + |
| Sarcoidosis | + | + |
| Photodermatitis | + | – |
| Scleroderma | + | + |
| Papulosquamous dermatoses | ||
| Lichen planus | + | – |
| Tinea striata | – | + |
| Psoriasis | + | + |
| Drug-induced dermatoses | ||
| Phototoxic dermatitis | + | – |
| Persistent drug erythema | + | – |
| Stevens-Johnson syndrome | + | + |
| Intralesional corticosteroid injections | – | + |
| Topical corticosteroids | – | + |
| Hydroquinone | + | + |
| Physical effects | ||
| Minor injuries | + | + |
| Burns | + | + |
| Abrasions | + | – |
| Radiotherapy | + | – |
| Dermabrasion | + | + |
| Chemical peeling | + | + |
| Cryotherapy | + | + |
| Other states | ||
| Acne | + | – |
| Mycosis fungoides | + | + |
| Persistent dyschromic erythema | + | – |
In the diagnosis of post-inflammatory dyschromia, one should take into account a history of a previous inflammatory/pathological process, medication use, excess sunlight, frequent visits to a solarium, or skin damage in the affected area ( Fig. 1, 2 ). It is important to find out the hereditary history - the presence of hyper- or hypopigmentation in close relatives.
The distribution of hypermelanotic lesions depends on the location of the original dermatosis or the site of injury. Their color varies from light brown to black - the shade will be lighter if the pigment is located in the epidermis, and darker if it is in the dermis.
Rice. 1. Areas of post-inflammatory hyperpigmentation on the face of a 42-year-old woman after acne (www.medscape.com)
Rice. 2. Multiple foci of post-inflammatory hypopigmentation on the arm (www.bmj.com)
What are pigmented skin diseases?
This category includes skin conditions associated with excess melanin accumulation, such as melasma, solar lentigo, post-inflammatory hyperpigmentation, chloasma, photoaging (Ogbechie-Godec, Elbuluk 2017).
According to domestic dermatologists, during a month of active practice, at least ten patients with the problem of age spots turn to them for professional help (Kasikhina 2011).
Sun-exposed areas of the skin of the face are usually affected, but there have been cases of involvement of the skin of the hands and other areas of the body.
As the word “hyperpigmentation” implies, this skin condition is characterized by increased production of the melanin pigment, caused by various factors, and primarily by solar radiation.
Principles of treatment and hardware correction
In the case of post-inflammatory hypo- or hyperpigmentation, the underlying pathology should be treated and the patient should be monitored dynamically. Often, after a few weeks (or months), the skin area will return to its normal color and no further treatment is required.
Post-inflammatory hyperpigmentation
If the cause of hyperpigmentation has been eliminated, but darkening of the skin remains, treatment should begin taking into account the depth of melanin:
- If pigmentation caused by increased melanin synthesis or the accumulation of other pigments (for example, lipofuscin) is localized in the stratum corneum or upper layers of the epidermis, it can be eliminated by exfoliating agents in combination with UV filters.
- Pigmentation localized in the deep layers of the epidermis can be reduced by means that affect the synthesis of melanin, as well as having a toxic effect on the melanocytes themselves (plus agents that destroy pigment).
- If pigmentation is located in the dermis, it is difficult to influence it using cosmetology methods; this may require hardware techniques.
Post-inflammatory hyperpigmentation can be treated with hydroquinone, tranexamic acid, retinoids, salicylic acid, alpha hydroxy acids (peels), hydrocortisone, etc. Also, do not forget about photoprotection of the skin using UV filters and clothing.
A number of studies have shown the effectiveness of fractional photothermolysis and IPL therapy in solving the problem of post-inflammatory hyperpigmentation. Since the cause of this condition is often a burn injury, techniques with minimal thermal exposure should be chosen. For example, non-ablative fractional lasers such as Fraxel are used to treat post-inflammatory hyperpigmentation, while ablative lasers are rarely used.
Post-inflammatory hypopigmentation
In this case, the main efforts should be directed to treating the inflammatory process - usually this is enough to gradually even out the skin color.
If this does not help, you can irradiate the skin with ultraviolet light (simple tanning or PUVA therapy) - under its influence, the remaining “weak” melanocytes can be activated and begin to synthesize pigment. It is important to be careful here not to convert hypo-pigmentation into hyperpigmentation.
Makeup is suitable as a concealer for bleaching small areas.
Post-inflammatory hypopigmentation can also be subjected to hardware cosmetology correction techniques, provided that the inflammatory process has stopped. Typically, non-ablative fractional lasers are used for this, which create micro-zones of damage in the depigmented area and in the adjacent normally colored area. In this case, the cells get a chance to proliferate and migrate to neighboring areas - as a result, the area of the pigmented area bordering healthy skin is gradually populated with melanocytes, followed by its staining.
Questions from our users:
- post-inflammatory hyperpigmentation causes
- post-inflammatory hyperpigmentation after burn
- post-inflammatory hyperpigmentation medication
- post-inflammatory hyperpigmentation treatment
The many faces of hyperpigmentation
Today, hyperpigmentation is considered one of the main signs of aging. Dark spots in the décolleté area, on the face and hands are perceived as an inevitable symptom of hormonal changes or liver disease. It is not surprising that women are as concerned about the appearance of characteristic spots as they are about new wrinkles.
The production of melanin (skin pigment) is a natural reaction of the skin that tries to prevent UV rays from penetrating into the nuclei of cells where DNA is located.
Hyperpigmentation occurs when, due to dysfunction of melanocytes (cells that produce melanin), melanin is synthesized many times more than necessary. This can happen for several reasons. Let's look at them in order.
Traumatic hyperpigmentation
This hyperpigmentation occurs due to the release of melanin in response to skin damage - as a kind of attempt by the body to protect itself.
This type of hyperpigmentation occurs more often in people predisposed to it, so if you have freckles on your face, be careful with peels, laser therapy, and squeezing pimples.
Help: The good news is that this type can only be treated with external remedies, i.e. ointments, creams and serums. Look for so-called “tyrosinase inhibitors” in the formulations - a protein that controls melanin synthesis: hydroquinone, arbutin, kojic acid, licorice root extract, nicotinamide, emblica extract, vitamin C, alpha-lipoic acid. As well as new products on the cosmetic market - synthetic peptides oligopeptide-34, oligopeptide-51.
Despite the fact that the mutagenic effect of hydroquinone has been actively discussed recently, cosmetologists have not yet developed a more effective whitening agent. Hydroquinone is particularly blamed for causing malignant tumors in rats. However, in the human body this substance is “neutralized” in the liver with the formation of non-toxic derivatives. Hydroquinone is approved for over-the-counter cosmetics at a concentration of 2%, but in some salons cosmetologists can make their own products containing a higher percentage. The main reason for limiting this drug for sale is various types of dermatitis due to the use of products with substance concentrations of 5% or higher.
Pigmentation in the elderly (lentigo)
Occurs in older people as a result of repeated exposure to UV radiation
The so-called “solar lentigo” are small spots 1 cm in diameter with a smooth edge, very similar to freckles. They appear on the hands and face, but unlike freckles, they do not disappear in winter and do not become paler. Lentigines occur in areas exposed to UV radiation throughout life. This is why it is important to use sunscreen on your neck, décolleté and arms at all times, especially if you spend a lot of time in the sun or like to visit a tanning salon.
Help: There are many ways to reduce the appearance of lentigo, it all depends on how quickly you want to see results. Long-term treatment includes the use of retinoids and sunscreens, as well as serums with tyrosinase inhibitor agents. The best results are obtained by combining these substances with glycolic acid, which helps them penetrate deeper into the skin. For example, a combination of glycolic acid with nicotinamide (vitamin B3) and retinol or resorcinol is good. If you want quick results, peelings with trichloroacetic acid and laser correction (Fraxel, IPL laser) are included in the treatment.
Chloasma, or “mask of pregnancy”
Chloasma (melasma) is a fairly typical skin condition during pregnancy or when using contraceptives.
This is due to an increase in estrogen levels. There are 2 types of melasma: epidermal and dermal, although the mixed type is more common.
Epidermal melasma
appears in the form of spots from light to dark brown, in some cases even black, with jagged edges. This type is more amenable to correction, since melanin is located in the upper layers of the skin, which means that the whitening components from creams and serums can achieve their goal.
Dermal melasma
appears in the form of gray-blue spots, the pigment lies in the middle layers of the dermis, where the lightening components no longer penetrate.
To make a correct diagnosis, it is best to use a Wood’s lamp (“blue lamp”) - the brighter the spots in the light of the lamp (epidermal melasma), the easier the therapy will be. However, most women do not conduct such tests, but simply randomly buy “whitening serums” in the hope that the spots will go away on their own. Alas, such a strategy does not always lead to success. Chloasma is one of the most stubborn types of hyperpigmentation. Lasts for a very long time even after the end of pregnancy or discontinuation of COCs.
Help: Hydroquinone, azelaic acid, a combination of retinoids and corticosteroids, such as fluocinolone (Fluocinoloni acetonidum), will help you in treatment. Oddly enough, but in this case, azelaic acid at a 20% concentration may be even more effective than hydroquinone at 2-4%. To speed up the effect, the so-called Jessner peel (an alcohol solution of resorcinol, salicylic and lactic acid) or peeling with salicylic and glycolic acids is performed once every two weeks. If you add medications with kojic acid to this treatment, the effectiveness increases further. In some cases, IPL laser treatment or microdermabrasion may make sense.
If you want to correct the manifestations of chloasma during pregnancy, be sure to consult your doctor!
Whatever regimen you and your dermatologist choose, the main thing is to strictly follow the regimen. To make this routine easier for consumers, manufacturing companies such as Obagi and La Roche-Posay produce products in special “numbered” packaging.
Today, cosmetic options are such that hyperpigmentation is not necessarily “forever.” Reducing unpleasant stains is possible even in the most severe cases. Of course, for skin 30+, spots will not disappear with the wave of a magic wand, and here you should no longer rely on “green” cosmetics. But the right therapy will definitely help you!
Tatiana Morrison
Photo thinkstockphotos.com
Products by topic: (retinol), [product](fluocinolone), [product](salicylic acid), [product](achromine), [product](acids), [product](peptides)