345
230
Diaper rash in newborns (diaper dermatitis) is a problem that almost every mother faces. Irritation usually appears in the folds of the baby’s skin (cervical, popliteal, inguinal, elbow, axillary), sometimes you may notice diaper rash on the baby’s bottom.
Most often, irritation occurs in children from 1 month to a year. According to statistics, diaper dermatitis of varying degrees occurs in 50% of children under 2 years of age (USA - 75%, Japan - 87%). It is important to detect redness in time and exclude possible complications.
Causes of diaper rash in newborns
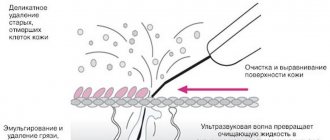
The main reason why newborn babies are most susceptible to diaper rash is the structure of their skin. The lipid barrier on its surface is still very thin and sensitive to any aggressive external influences, and the stratum corneum is 30% thinner than that of an adult.
As a result, the protective properties of the skin can be destroyed due to temperature changes, frequent bathing, and the use of hygiene products that are not intended for children's skin.
Powder8
Powders are powdery products primarily based on talc and starch. Their main function is to absorb moisture, contact with which provokes skin inflammation. Most powders are intended to prevent diaper rash, but sometimes medicinal herbal extracts, anti-inflammatory or antibacterial components are added to them. In this case, they are also used to treat skin diseases. The powder is used morning and evening, applying it in a thin layer to clean, dry skin; if necessary, apply more often.
Recently, the advisability of powders has been discussed by pediatricians due to the high probability of their inhalation by the baby9. In addition, the powder collects deep in the folds, not providing reliable protection for the entire surface of the skin. It is increasingly recommended to replace powders with ointments that reliably protect the skin10. When using cream and powder at the same time, be aware that the talc may absorb water from the cream, and both products will not work.
Diaper rash usually occurs as a result of:
- excessive sweating. Due to the fact that some mothers are afraid of colds and hypothermia, they wrap their babies like cabbage. As a result, the child’s skin does not breathe at all, and sweat appears in its folds, which leads to inflammation.
- untimely hygiene. Newborns defecate very often. Uric acid itself causes irritation, and when combined with feces it forms ammonia, which can damage the skin many times more.
- mechanical impact. This could be a diaper that is not put on correctly, clothes made of synthetic fabrics or with tight seams, or uncomfortable underwear.
- high humidity. Most often, this situation occurs when the baby is not wiped dry after bathing. Water remains in the folds of the skin and causes irritation. Diaper rash on the neck of a baby often appears for this very reason.
- allergies. Usually it comes in 2 types: food. If the baby is breastfed, then allergies can be caused by changes in the mother's diet. In addition, skin irritation is often provoked by foods that the baby first tries when complementary feeding begins.
- contact This may be a reaction to the chemical composition of washing powder, hygiene products or diapers.
About the disease
Diaper rash is irritation of the baby's delicate skin due to mechanical friction or secretions (urine, feces).
The skin often suffers in natural folds (perineum and under the arms). Inflammation primarily occurs without infection, especially with a change in diet, which changes the properties of feces. However, due to the nature of children's skin, a bacterial or fungal infection can quickly develop, requiring immediate treatment. Diaper rash most often occurs in children who are bottle-fed, have excess body weight for their age, have digestive disorders, are prone to allergies, have lactase deficiency, and abnormal kidney development. Excessive wrapping, high room temperature, untimely bathing, prolonged stay in wet diapers or a diaper of the wrong size contribute to the development of diaper rash.
In practice, to select the correct treatment method, the following classification of diaper rash is used:
- diaper dermatitis - redness and rash appear only in those places that are constantly in contact with wet diapers;
- allergic ring - occurs around the anus due to a food allergy that develops to a new food product;
- seborrheic eczema - the skin of the lower abdomen and genitals becomes rough, swollen, oily to the touch, the border with normal skin is clear, looks like a hyperemic (bright red) huge spot;
- intertrigo - affects natural folds (gluteal, elbow, popliteal and others), against the background of redness, weeping cracks form, this condition is provoked by increased humidity;
- genital candidomycosis - occurs when a fungal infection is attached, has the appearance of red spotty rashes;
- impetigo - occurs when a pyogenic infection occurs; it first appears as separate and then small draining ulcers, which form crusts after drying. Impetigo in children forms on the buttocks.
Diaper rash at the initial stage can be eliminated with good care, changing the brand of diapers and using a high-quality baby skin cream. In severe cases, etiotropic treatment is required, aimed at combating the infectious onset.
What are the degrees of diaper rash?
Doctors distinguish 3 degrees of diaper dermatitis:
- 1st degree.
The mildest stage, in which only slight redness or rash is noticeable. There are no lesions on the skin, and the baby does not show any signs of anxiety. - 2nd degree.
The redness becomes brighter, in addition to them microcracks and small pustules appear. The child tries to reach out with his hands to damaged areas of the skin, is capricious, and cries when you change a diaper or clothes. - 3rd degree.
The redness is very intense, the area of diaper rash is covered with ulcers and ulcers, and liquid is released from cracks in the skin. The baby constantly cries and becomes overly restless, as the pain prevents him from sleeping, eating, and staying awake.
If parents cope with mild diaper rash on their own, then if more serious symptoms appear, you should immediately contact your pediatrician. Only he will be able to accurately make a diagnosis, determine the degree of development of the disease and tell you how to treat diaper rash in newborns. Please never act as a doctor yourself, otherwise you may face complications and unnecessary side effects.
Diaper rash care
How to treat diaper rash in newborns? Doctors recommend purchasing special products that will help soothe the skin and relieve irritation. The product must be safe for children's skin, without fragrances or dyes. Typically, special creams are applied several times a day until the redness completely disappears.
If you notice slight redness on your baby's skin, it is important to review his skin care and make the necessary adjustments. Usually it is enough to be more attentive during daily hygiene, change diapers in a timely manner, and make sure that the child does not overheat.
During this period, it is especially important to pay attention to the fact that skin care products are hypoallergenic, do not contain harmful additives, and are approved by pediatricians.
Anti-inflammatory powder “My Sunshine®” is included in this category. It will help prevent and eliminate irritation, redness and diaper rash. The composition includes zinc oxide, which perfectly dries out inflammation. Powder-cream “My Sunshine®” differs from regular powder in that it does not roll off on the skin and provides more comfortable and safe use. It prevents powdered talc from entering the baby's respiratory tract. You just need to apply powder-cream for diaper rash in newborns on the baby’s skin in places of redness and watch how they gradually disappear.
Also pay attention to the cream with panthenol “My Sunshine®”. It contains 5% D-panthenol, a concentration considered optimal in clinical studies. Cream Children's panthenol “My Sunshine®” promotes:
- restoration of healthy baby skin;
- improving the protective functions of the epidermis;
- protecting children's skin from moisture loss.
The cream is suitable both for getting rid of diaper rash and for preventing its occurrence.
Both products from the “Moyo Solnyshko®” brand can be used for babies from the moment of birth.
If you experience grade 2 or 3 diaper rash, you should visit your doctor. He will conduct the necessary tests and make an accurate diagnosis. In this case, all you have to do is follow his recommendations, follow the instructions in a timely manner and monitor the progress of treatment.
IN
Diaper dermatitis is an irritation of the skin of the gluteal region or inner thighs in infants and young children caused by physical, chemical and microbial factors [3, 9, 11, 12]. According to various authors, diaper dermatitis develops in children in 30–70% of cases [1, 5, 2, 8, 9]. It usually occurs in children aged 3 to 12 months, more often in girls [2, 4, 7]. Diaper dermatitis is much more common in children suffering from atopic or seborrheic dermatitis. Breastfed children are much less likely to suffer from diaper dermatitis compared to children receiving artificial formula, this is explained by the lower enzymatic activity of feces during natural feeding [6, 10, 12]. Diaper dermatitis sometimes develops even with good care of the baby's skin, for example in the case of diarrhea, switching from liquid to solid food, or stopping breastfeeding.
Before moving on to considering the causes of diaper dermatitis, it is necessary to once again pay attention to the physiological characteristics of the child’s body. The skin is the first barrier to the penetration of bacteria and toxins into the body. The skin also protects the child’s body from temperature fluctuations, mechanical stress, and at different periods of childhood it has morphological and functional characteristics that make it especially vulnerable and vulnerable to various environmental influences.
The three-layer structure of the skin is characteristic not only of adults, but also of children [1, 4, 11]. The first (outer layer) is the epidermis
, in turn, is divided into basal, spinous, granular and stratum corneum.
The stratum corneum consists of 2-3 rows of keratinized cells, which are constantly rejected and replaced by new ones. It is known that the process of skin renewal completely takes about 25–30 days [2, 5, 8, 11]. The skin of a newborn is at risk because the outer layer is looser and its cells are very easily exfoliated and damaged. The dermis, the basis of the skin, consists of papillary and reticular parts and poorly developed connective tissue. This layer contains blood and lymphatic vessels, nerve endings, hair papillae, sebaceous and sweat glands. The skin is elastic due to the interweaving of collagen and elastin fibers; it is the insufficient development of collagen and elastic fibers that reduces the natural shock-absorbing ability of the skin in children [3, 5, 10]. Infants have 12 times more sweat glands than adults [1, 9, 12]. The process of sweating begins first on the face (from the 2nd–5th day of life), then on the palms and other parts of the body. Fully sweat glands are formed only by the age of 3, which is explained by imperfect innervation of the skin of newborns [11, 12]. It is interesting that the number of sebaceous glands is 4–8 times greater than in adults, but by the age of 2 their function decreases and increases only by adolescence. Subcutaneous tissue protects the skin
from mechanical and thermal damage .
It is formed from adipose tissue and collagen fibers. The low activity of the local immunity of the child’s skin leads to its slight vulnerability. The macrophage system of the epidermis and dermis, including Langerhans cells and histiocytes [1, 3, 7, 12], provides antimicrobial properties. But at the same time, the bactericidal activity of skin neutrophils in young children is not sufficiently developed [5, 9]. The immaturity of cellular and humoral immunity in young
children After the birth of a child, active microbial colonization of his skin begins, mainly with staphylococcal flora, which is part of the normal microflora of the child’s skin. High humidity and low acidity of the baby's skin can promote excessive growth of various microorganisms on its surface, including staphylococci [3, 4, 7]. The respiratory function of the skin in children is more active than in adults. Gases easily diffuse through the wall of numerous skin vessels. Contamination of the skin excludes it from the process. The infant's skin receptors provide tactile, thermoregulatory and pain sensitivity. Under the influence of sunlight, the skin synthesizes the pigment cholecalciferol [4, 6, 11]. Excessive contamination of the skin impairs its functions and leads to irritation of sensitive receptors, which causes anxiety for the child.
All these features lead to more frequent mechanical damage and possible infectious and allergic inflammation. Therefore, proper care of a child’s skin is care for the prevention, first of all, of inflammatory diseases. The integrity and preservation of the protective functions of the skin are very important.
So, the goal of skin care for young children is to ensure normal microbiocenosis and prevent irritation and damage to the epidermis.
To cleanse the skin of a newborn and young child, use water and special grades of pH-neutral baby soap, and choose special detergents without alkaline components.
With frequent bathing and the use of cosmetics, children's skin becomes dry, cracks appear in the stratum corneum, and irritation reactions intensify in the form of redness and fine pityriasis-like peeling. In children predisposed to skin diseases, especially such as seborrheic and atopic dermatitis, in such cases water-oil emulsions, baby and cosmetic milks can be used. Using powder and cream on the same areas of the body can lead to maceration of the skin. Oils that protect the skin from dehydration and degreasing are recommended for the bath. Baby soap with lipid additives provides a cleansing, degreasing, but at the same time hydrating effect. To wash hair, use a special children's shampoo that does not irritate the mucous membrane of the eyes. Constant care is necessary for the child's perineal area, as it is in constant contact with moisture and metabolites excreted in the urine. For the prevention of diaper dermatitis
, infections, maceration of the skin under the influence of feces and urine, after thorough cleansing, the skin must be powdered and lubricated with ointment, which contains 5% dexpanthenol, which promotes tissue regeneration. You should always keep in mind that some children do not tolerate any cosmetic products well.
It is prohibited to use cosmetics containing antibiotics on the skin of a healthy infant. This can lead to changes in the microbiocenosis of the skin and the development of a fungal infection.
Baby skin care products
| Means | Purpose of application |
| Soap, pH neutral | Cleansing and moisturizing the skin |
| Powder | Skin protection, moisture absorption, diaper rash prevention |
| Oils | Protection, skin regeneration, hydration |
| Cosmetic milk | Cleansing, skin protection, moisturizing |
| Cream | Skin protection, moisturizing, anti-inflammatory and anti-allergic effect, prevention of diaper dermatitis |
| Ointments | Skin protection, hydration, prevention of diaper dermatitis |
| Wet wipes | Cleansing and moisturizing the skin |
Children under 6 months are bathed daily for at least 5 minutes, over 6 months - every other day, the duration of the water procedure is about 10 minutes. The soda temperature is usually 36–37 °C. In the hot season, in summer, a child, regardless of age, is bathed daily. Use pH-neutral soap 1-2 times a week. At the end of the water procedure, the child should be doused with water at a temperature 1–2 °C lower than the water in the bath.
The baby's perineal area is in constant contact with moisture and requires constant care. It is very important to regularly remove waste products from the body in the form of urine and feces from the skin. It is necessary to wash the child with water after each bowel movement, thoroughly washing the numerous folds and buttocks. The baby's delicate skin is blotted with a soft towel. The girl is washed from front to back with water without soap. Regular cleansing of the skin in itself will help prevent the development of diaper dermatitis. You can use special wipes with which you can remove all dirt. They are especially convenient on the road when there are no toilet facilities for the child. To prevent infection and maceration of the skin under the influence of feces and urine, after thorough cleansing, the skin must be powdered, lubricated with cream, ointment or oil. All care products are applied to the skin in moderation, with mandatory assessment of their effectiveness, since many children do not tolerate any cosmetic products well. In this case, air baths in the genital area for 10–15 minutes are helpful. The prevention of diaper dermatitis is facilitated by the use of disposable absorbent diapers, as well as dietary correction aimed at reducing the amount of protein to the age norm in order to reduce the acidity of feces, which have a strong irritating effect on the skin. Errors in caring for a child’s skin can lead to a violation of its integrity and the development of an inflammatory reaction.
An effective way to prevent diaper dermatitis is the use of disposable absorbent diapers with a gel component. Diapers absorb moisture, concentrate feces, and reduce the damaging effects of enzymes contained in the baby's secretions. Diapers containing gel, compared to gauze diapers made of cotton, are significantly more likely to prevent irritation and diaper rash of the skin in the buttocks and perineum.
Skin irritants can be eliminated by reducing the hyperacidity of feces that results from a diet high in protein. Reducing the amount of protein in a child’s food to the age norm, temporarily eliminating acidic juices and fermented milk mixtures (for example, kefir) reduce the acidity of the child’s discharge, preventing the development of diaper dermatitis.
Most often, diaper dermatitis develops in children aged 6 to 12 months, but it can also develop earlier (for example, from 3 months of age). Girls are much more likely to suffer from diaper dermatitis. Often the development of the disease is facilitated by the appearance of loose stools.
Diaper dermatitis is a consequence of skin irritation due to the impact of mechanical, physical, chemical, and microbial factors on the skin.
Causes of diaper dermatitis in children
|
|
| |
|
|
|
|
|
|
In children with diaper dermatitis, infiltrates appear in the area of skin folds and buttocks, erosions, ulcers, papules, and weeping.
It is customary to distinguish between primary and secondary diaper dermatitis [1, 10, 12]. In turn, primary diaper dermatitis is divided into:
1) uncomplicated as a result of improper care, constitutional characteristics of the child’s skin (exudative-catarrhal type of constitution), as well as metabolic processes (ammonia irritation);
2) complicated, with the addition of a fungal infection (candidiasis), bacterial infection (staphylococcal, streptococcal, gram-negative flora), viral infection (usually herpetic), allergic or toxic skin lesions.
Secondary diaper dermatitis develops in patients with systemic skin diseases.
The course of diaper dermatitis depending on concomitant diseases
1. Combination of diaper and atopic dermatitis. In this case, atopy contributes to the development of diaper dermatitis. What are the distinctive features of atopic dermatitis?
· Family history of atopic diseases (atopic dermatitis, bronchial asthma, allergic rhinitis, hay fever, etc.).
· Typical localization characteristic of atopic dermatitis (skin of the cheeks, forehead, flexor surface of the arms and legs).
· Damage to the perineal area is not typical for atopic dermatitis.
· Consecutive appearance of elements (papules, vesicles, eczematous skin lesions, crusts, lichenification, etc.).
· Often with atopic dermatitis there is simultaneous damage to other organs (respiratory, gastrointestinal tract, etc.) [3, 12].
· Laboratory indicators (increased levels of eosinophils in the blood, high levels of immunoglobulin class E and specific antibodies of food, fungal, bacterial, household and other spectra).
In the case of a combination of diaper rash and atopic dermatitis, improvement in the condition is observed only as a result of complex therapy. Proper skin care is very important. To prevent diaper dermatitis, the skin of children with atopic dermatitis can be periodically treated with zinc paste, the fatty fraction of which contains petroleum jelly. The paste contains zinc oxide and wheat starch as a powder component. It is preferable to use soft preparations that do not contain potential allergens.
2. Combination of diaper and seborrheic dermatitis. Seborrheic skin damage is localized on the skin of the scalp (gneiss), behind the ears, on the forehead, and cheeks of the child. Seborrhea elements may appear on the inner surface of the thighs and buttocks. Seborrheic dermatitis is characterized by the appearance of redness of the skin, severe dryness, papules with pityriasis-like peeling, sometimes merging plaques, and sebaceous crusts. Seborrheic dermatitis is often combined with candidal and fungal infections [8, 10, 11], and a possible combination with atopic dermatitis. As a result of combined skin lesions, an extensive weeping surface and the development of diaper dermatitis can form.
3. Complicated diaper dermatitis. Fungi of the genus Candida albicans are considered the main culprit of complicated diaper dermatitis. The clinical picture of candidiasis is well defined: bright erythema of the skin with clearly defined boundaries, located in the area of the inguinal folds, buttocks, thighs, abdomen and external genitalia. Primary manifestations in the form of papules or vesicles quickly spread, forming large areas of lesions with possible ulceration of the skin. Vesicles and pustules often form along the edges of the affected areas, the appearance of which indicates viral or bacterial damage to the skin. Often in children with severe manifestations of the complicated course of diaper dermatitis, urination disturbance (painful, frequent) is observed. A urinary infection may develop. Children often become restless when defecating. As a rule, elimination of Candida albicans infection is not accompanied by a complete cure for diaper dermatitis [6, 9, 10], since cutaneous candidiasis is not the only cause of dermatitis. In addition to antifungal agents (clotrimazole ointment, nizoral and others), it is necessary to use D-PANTHENOL.
4. Combination of diaper dermatitis with IMPETIGO (pustular skin lesions). Most often, bullous elements appear on the skin of staphylococcal etiology. Often, after opening the bullae, superficial ulcers form.
5. Combination of diaper dermatitis and FOLLICULITIS (infected prickly heat). This disease is considered as a complication of prickly heat on the skin in contact with diapers. When overheated, papules and pustules appear in these places. The cause of infection is the microbe Staphylococcus aureus.
It is necessary to begin treatment immediately when the first clinical symptoms of diaper dermatitis (redness, swelling) appear. First of all, you need to stop using regular cloth diapers and oilcloths and switch to using disposable diapers with increased absorption capacity (containing a special gel). And even such diapers must be changed at least every 4 hours [1, 3, 8]. In the presence of a complicated course of diaper dermatitis caused by Candida albicans fungi, ointments containing antifungal antibiotics, such as clotrimazole, nystatin, pimafucin, nizoral, are used. In the presence of bacterial complications, antibiotic ointments are used. To treat affected areas of the skin, you can use creams and ointments based on zinc, which has a drying, antimicrobial effect that helps create a protective layer on the surface of the skin.
Medicines for external treatment of diaper dermatitis
| A drug | Action | Mode of application |
| Powder (talc, zinc oxide, bismuth nitrate) | Cooling, anti-inflammatory, antipruritic | Used when there is no weeping. Dispersion with cotton wool or through gauze. |
| Lotions (solutions of medicinal substances in distilled water - boric acid 2%, silver nitrate 0.10–0.25%, furatsilin solution 0.01–0.05%) | Anti-inflammatory, stimulation of epithelization | Used in cases of weeping and erosive processes. Moisten 4–5 layers of gauze with a lotion and place on the affected area of the skin. |
| Solutions of aniline dyes (aqueous or 1–2% alcohol) | Antimicrobial, anti-inflammatory, drying | They are applied to the skin in the acute phase of inflammation, used to open blisters and treat affected skin, applied by shading with a swab or spraying. |
| Chatterboxes are powdery substances mixed with water and glycerin, with water and vegetable oil (liquid or thicker) | Anti-inflammatory, antipruritic | Used for inflammation without weeping. Shake well before applying to skin. |
| Paste (a mixture of medicine in powder form and a fat base in equal proportions with the addition of naphthalan, ichthyol, sulfur, tar) | Anti-inflammatory, drying, softening | It is used during the period of subsidence of acute inflammatory phenomena, for minor erosions. Apply without a fixing bandage. |
| Ointment - a mixture of medicinal substances (naphthalan, resorcinol, corticosteroids - 10%) and a fatty base (lanolin or vegetable oil - 90%) | Anti-inflammatory, antipruritic, emollient, exfoliating, epithelializing | It is used during the period of subsidence of acute inflammatory phenomena, on areas of redness and minor erosions. Apply to the affected area for 12–24 hours. |
One of the highly effective remedies for the treatment of diaper dermatitis is D-panthenol, the active principle of which is dexpanthenol (provitamin B5).
D-PANTHENOL:
Ø has an anti-inflammatory effect;
Ø accelerates skin regeneration;
Ø improves metabolic processes in the skin;
Ø increases skin elasticity.
D-PANTHENOL is available in the form of 5% cream and ointment. 5% D-panthenol is effective for the treatment of skin redness, diaper rash, prickly heat, abrasions, and mild manifestations of infectious dermatitis in infants. Can be used to treat itchy skin in children. D-panthenol 5% ointment protects the sensitive skin of a child’s face from frost, dampness and wind. The drug may be useful for nursing women to treat nipples with cracks and inflammation.
Clinical trials to study the effectiveness and safety of dexpanthenol in the treatment of non-infected skin lesions in newborns, conducted in leading clinics in Russia, showed that all treated children had a clinical effect (58% of children had a complete disappearance of dermatitis, 48% had a significant reduction in skin symptoms) [1, 3, 11]. Our experience in the treatment of uncomplicated diaper dermatitis in 30 children aged 1 month to 1 year using dexpanthenol cream showed that all children on the 2-3rd day from the start of therapy experienced a decrease or disappearance of hyperemia in the gluteal region and perineum [1] . Clinical trials conducted to study the effectiveness and safety of dexpanthenol ointment in the treatment of infected skin lesions in newborns in leading clinics in Russia and abroad showed that all treated children had a clinical effect (58% of children had a complete disappearance of dermatitis, 48% had a significant decrease skin symptoms) [2, 10, 11]. Children's anxiety decreased and sleep improved. Our observations and literature data allow us to consider dexpanthenol one of the most effective and safe means for prevention and treatment
diaper dermatitis.
However, when prescribing the drug, the doctor should always take into account the individual sensitivity of the skin to various products recommended for care.
ICD-10. Atopic dermatitis L20. Diaper dermatitis L22.
Bibliography
1. Geppe N. A., Belousova N. A., Korovina N. A. et al. // Modern aspects of early child care using disposable diapers. - M., 1998. - P. 5.
2. Krafchik BR, Eczematous Disorder. Textbook of Neonatal Dermatology. 241–2001.
3. Longhi F., Carlucci G., Bellucci R. et al. Diaper dermatitis: a study of contributing factors // Contact Dermatitis. 1992. - v. 26. - pp. 248–252.
4. Prasad H., Srivastava P., Verma K. Diaper dermatitis - an overview // Indian J. Pediatr., 2003. - v. 70. - pp. 635–637.
5. Davis J., Leyden J., Grove G., Raynor W. Comparison of disposable diapers with fluff absorbent and fluff plus absorbent polymers: effects on skin hydration, skin pH, and diaper dermatitis // Pediatr. Dermatol., 1989. - v. 6. - pp. 102–108.
6. Wilson P., Dallas M. Diaper performance: maintenance of healthy skin // Pediatr. Dermatol., 1990. - v. 7. - pp. 179–184.
7. Prasad H., Srivastava P., Verma K. Diapers and skin care: merits and demerits // Indian J. Pediatr., 2004. - v. 71. - pp. 907–908.
8. Adam R. Skin care of the diaper area // Pediatr. Dermatol., 2008. - v. 25. - pp. 427–433.
9. Korting H., Braun-Falco O. The effect of detergents on skin pH and its consequences // Clin. Dermatol., 1996. - v. 14. - pp. 23–27.
10. Andersen PH, Bucher AP, Saeed I. Faecal enzymes: in vivo human skin irritation. Contact Dermatitis. 1994; 30 (3): 152–158.
11. Davies D., Dore A., Perissinotto K. Topical Vitamins A, or it's derives in topical treatment of napkin dermatitis in infants. The cochrane library. Issue 1. 2009: 2–5.
12. Li C., Zhu Z., Dai Y. Diaper dermatitis: a survey of risk factors for children aged 1–24 months in China // J. Int. Med. Res., 2012. - v. 40. - pp. 1752–1760.