Why does my neck swell?
Traumatic injuries
Soft tissue bruises are accompanied by moderate local swelling and pain that intensifies during neck movements.
The swelling disappears within a few days. Subluxation of the cervical vertebra occurs as a result of a sharp turn of the head, and is more often detected in children. Asymmetrical swelling of the back of the neck is complemented by a forced position of the head, pain, and muscle tension. In case of fractures, local swelling is determined in the projection of the spinous process of the damaged vertebra. In victims with laryngeal injuries, external swelling is usually minor. Severe swelling can be a consequence of severe complications: internal bleeding into soft tissues, subcutaneous emphysema that occurs against the background of a rupture or penetrating wound of the larynx. Difficulty breathing, aphonia, and pain are noted. Hemoptysis and asphyxia are possible.
With uncomplicated laryngeal foreign bodies, there is no symptom. Against the background of inflammation in the area where a foreign object is located, swelling of varying severity occurs, combined with pain, hyperthermia, and symptoms of intoxication. A life-threatening condition is perforation of the larynx by a sharp foreign body with the development of subcutaneous emphysema.
Diseases of the lymphatic system
Swelling of the neck is often associated with inflammation of the regional lymph nodes. The following diseases can cause lymphadenitis:
- Purulent lesions of soft tissues
: infected wounds, boils, carbuncles, abscesses, phlegmon of the face, head and neck. - Dental problems
: caries, pulpitis, gumboil, stomatitis, purulent mumps, maxillary abscess, abscesses of the tongue, oral cavity, osteomyelitis of the jaw. - ENT pathologies
: tonsillitis, chronic tonsillitis, paratonsillar, parapharyngeal, intratonsilal abscesses, otitis, pharyngitis, laryngitis. - Children's infectious diseases
: diphtheria, scarlet fever, mumps. - Dangerous infections
: plague, anthrax.
In children with chronic skin diseases, lymphadenitis of the cervical, submandibular, and occipital lymph nodes occurs with the development of Kaposi's eczema herpetiformis. Enlarged lymph nodes also become a consequence of the lymphogenous spread of malignant tumors: cancer of the tongue, lower and upper jaw, larynx, pharynx, nose, paranasal sinuses.
Swelling of the neck due to thyroiditis
Endocrine pathologies
The most pronounced diffuse swelling of the neck is observed with myxedema. Not only the neck, but also the face swells; in severe cases, the swelling spreads throughout the body. Distinctive features are the absence of redness, pallor, pitting when pressing on the skin, shortness of breath, lethargy, lethargy, and increased sensitivity to cold. Changes in the anterior surface of the neck are determined in all forms of goiter:
- Diffuse euthyroid goiter.
The general condition has not changed, sometimes weakness and headaches are observed. In mild cases, swelling is noticeable only when palpating, tilting the head back, in severe cases it reaches the level of a pronounced cosmetic defect. - Diffuse toxic goiter.
Detailed symptoms of thyrotoxicosis are detected. The thyroid gland is uniformly enlarged, the degree of swelling does not always correlate with the severity of the disease. - Nodular goiter.
The function of the gland is often preserved; some patients show signs of hypo- or hyperthyroidism. The swelling of the neck is uneven, one side is larger than the other.
In acute thyroiditis, swelling is combined with pain, local hyperthermia, hyperthermia. The onset of the purulent form of thyroiditis is marked by increased pain, severe fever, and lymphadenitis. In patients with subacute thyroiditis, the body temperature is subfebrile, there is swelling, moderate pain in the projection of the thyroid gland, in half of the cases symptoms of thyrotoxicosis are detected. Chronic thyroiditis develops gradually. The affected area is lumpy and painless.
Maxillofacial pathology
The cause of swelling is often diseases of the salivary glands and soft tissues. Swelling is observed in the following pathological conditions:
- Sialadenitis.
The parotid salivary gland most often suffers; a one-sided painful swelling is located on the border of the neck and lower jaw, next to the earlobe. Less commonly affected are the submandibular salivary glands, which are localized in the submandibular triangle of the neck. - Purulent parotitis.
With purulent inflammation, swelling spreads to the neck, cheek, and submandibular area on the affected side. A pronounced deformation occurs. Pain, general hyperthermia, severe weakness, weakness are noted. - Salivary gland abscess.
Along with the parotid, other salivary glands may be affected. In 50% of cases, inflammation affects the paired organ. The area of swelling corresponds to the location of the affected gland. There is severe pain, febrile body temperature, and severe intoxication syndrome. - Perimaxillary abscess.
Formed as a complication of tonsillitis, furunculosis, infected abrasions of the skin and oral mucosa. Unilateral swelling is detected in the area of the submandibular triangle. When the abscess ruptures, swelling spreads down the neck. - Cellulitis of the neck.
It is provoked by odontogenic or tonsillogenic infection, foreign bodies of the laryngopharynx. Swelling appears on one side, grows quickly, and diffusely covers a significant part of the neck. The skin over the area of swelling is red, hot, and tense. The general condition is serious.
Diseases of the ENT organs
Swelling of the neck in otolaryngological diseases is often caused by lymphadenitis. Diseases accompanied by swelling of the neck, not associated with enlarged lymph nodes, include:
- Chondroperichondritis of the larynx.
A limited area of swelling is located in the front of the lower or middle third of the neck. Combined with chills, weakness, hyperthermia, pain, aggravated by talking, coughing, swallowing. - Neck cyst.
The tumor-like formation is localized on the lateral or anterior surface, and is more clearly contoured when the head is turned in the opposite direction. In the absence of inflammation, it is asymptomatic. When infected, the skin turns red, the cyst enlarges, becomes painful, and swelling spreads beyond the affected area. - Retropharyngeal abscess.
Swelling of the neck behind the angle of the lower jaw, sore throat, breathing problems aggravated in an upright position, severe impairment of the general condition, and hyperthermia are detected. - Lemierre's syndrome.
Postanginal anaerobic sepsis is manifested by swelling of the lower part of the lateral surface of the neck (in the projection of the jugular vein), pain, progressive deterioration of the condition up to impairment of consciousness and speech, the development of pneumonia, arthritis, and osteomyelitis. - Ludwig's sore throat.
The disease is characterized by a rapid onset and severe course with fever, intoxication, severe sore throat, and diffuse swelling of the soft tissues of the neck. On palpation, the tissues are painful, dense, and “woody.”
Allergy
With angioedema, swelling of the neck, face, lips, eyelids, ears, limbs, and genital area is observed. The swelling is painless, accompanied by a feeling of tension and fullness, and pale skin. It is provoked by contact with allergens: drugs, food, insect poison. Sometimes it occurs due to pseudo-allergy. In addition, severe swelling of the face, neck, feet, and hands is found in the edematous type of allergy to salicylates.
Infectious diseases
The most common infectious cause of neck swelling is mumps. Swelling is detected in the area of the salivary glands, often bilateral, sometimes asymmetrical. Due to the enlargement of the upper parts of the neck, the face becomes pear-shaped. Severe swelling of the anterior parts of the neck is detected in the toxic form of diphtheria. 1st degree is characterized by swelling reaching the middle of the neck, 2nd – to the collarbones, 3rd – spreading to the face, chest, back, back of the neck.
In patients with typhus, redness and swelling of the face and neck are accompanied by injection of the conjunctiva, the appearance of a thick rash on the torso and limbs, hepatosplenomegaly, oliguria, neurological disorders, and severe intoxication.
Neoplasms
Local swelling of the neck may be due to the development of neoplasia, which includes:
- lipomas, fibromas;
- cancer of the pharynx and larynx;
- thyroid tumors.
Benign neoplasms are limited, painless swellings that do not increase or increase very slowly in size. Malignant neoplasia rapidly progresses, causes enlargement of lymph nodes, invades neighboring organs, and is accompanied by breathing and swallowing disorders, and voice changes.
Other reasons
The list of other causes of neck swelling includes a number of diseases of various etiologies:
- Rheumatology, orthopedics
: cervical myositis, Shulman's disease, scleroderma, dermatomyositis. - Cardiology, pulmonology
: exudative pericarditis, pleurisy, mediastinitis, superior vena cava syndrome. - Dermatology
: furunculosis, bullous dermatitis. - Neurology
: Melkersson-Rosenthal syndrome. - Nephrology
: membranous glomerulonephritis. - Emergency conditions
: cytokine storm.
Swelling in the neck
Swelling in the neck - Growths in the neck - Lymph nodes in the neck - Lump in the neck
Patients and their families may notice a lump in the neck area, or it may be discovered during a routine examination. A lump in the neck area may be painless or painful, depending on the cause. When neck augmentation is painless, it may take a long time before patients seek medical attention.
Cause:
There are many causes of cervical mass, including inflammatory diseases, neoplasms, and congenital diseases.
The most common causes in younger patients include the following:
- local and generalized lymphadenopathy - acts as an organizational response to a viral or bacterial infection, usually of the oropharynx, tongue, salivary glands, pharynx and scalp.
- primary bacterial infection
- systemic infections
- some systemic infections (eg, mononucleosis, HIV, tuberculosis)
- congenital disorders can cause a cervical mass (a growth on the neck), usually in the long term. The most common is thyroglossal duct cyst, branchiogenic tumor, etc.
- Neoplastic masses (neoplastic masses) are more common in older patients, but can also occur in younger people. These masses may represent the site of a primary tumor or lymph node metastases from local, regional, or distant cancer. Approximately 60% of the supraclavicular mass is lymph node masses metastasized from distant primary sites. In the neck, 80% of metastatic cervical lymph nodes originate from the upper respiratory and digestive systems. Possible localization of the tumor is the lateral surface of the tongue, floor of the mouth, nasopharynx, pharynx, laryngeal epiglottis and infraorbital region.
- The thyroid gland can dilate in various disorders, such as simple non-toxic goiter, subacute thyroiditis and, less commonly, thyroid cancer.
- The submandibular salivary glands may become swollen if the salivary duct is blocked by a stone, inflammation or tumor.
Reference Information:
As a history of this disease, it should be noted how long the mass has been present, and whether it is painful. It is important to note associated symptoms, which include sore throat, upper respiratory tract infection symptoms, tooth pain, nasal congestion, ear fullness, etc.
Questions about difficulty swallowing or speaking and symptoms of chronic illness (eg, fever, weight loss, general malaise). Peripheral and distant metastases of cancer cause throat symptoms in the swallowing system (eg, cough in lung cancer, difficulty swallowing in esophageal cancer). Because many types of cancer can metastasize to the neck, a complete otolaryngological examination of all systems is important and can help find the cause of the disease.
Your doctor should tell you whether you have HIV or tuberculosis and what risk factors you may be at risk for. Risk factors for cancer include alcohol consumption or tobacco use (especially snuff or chewing tobacco), poor placement of dentures, and chronic oral thrush. Poor oral hygiene can also be dangerous.
Physical examination:
It is necessary to determine the composition of the growth on the neck (that is, whether it is soft, elastic or hard), as well as the presence and degree of sensitivity. If the mass is freely mobile or stable, it appears only under the skin or the depth must be determined.
The scalp, ears, sinuses, mouth, nasopharynx, oropharynx, hypopharynx and larynx are closely associated with possible infection and any visible damage. The base of the tongue, the base of the oral glands, the thyroid gland and the salivary glands should always be palpated for possible involvement.
The mammary gland and prostate gland are palpated for possible hypertrophy, palpation of the spleen, and examination for splenomegaly. The presence of blood in the stool indicates gastrointestinal cancer.
Other lymph nodes are palpable (eg, armpits, groin).
Attention:
The following signs are of particular concern:
- Rigid, immovable mass
- Elderly patients
- Presence of oropharyngeal lesions (other than simple pharyngitis or dental infection)
- History of chronic hoarseness or dysphagia
Interpretation of results:
Significant differentiation of factors by neck mass (including severity, pain, mobility, size and location).
A new mass (that is, swelling of the neck just a few days old), especially after symptoms of an upper respiratory tract infection or pharyngitis , signifies benign reactive lymphadenopathy .
Chronic neck swelling in young patients may suggest a congenital cyst .
A lateral cervical mass in elderly patients, especially those with risk factors, should be considered cancer until proven otherwise!
The midline mass is likely a thyroglossal duct cyst.
Pain, tenderness, or both with cervical swellings indicates inflammation (especially infection), while a painless mass is a cyst or tumor. A tough, hard, painless mass suggests cancer , while an elastic texture and mobility suggest the opposite.
Generalized lymphadenopathy and splenomegaly may be found in infectious mononucleosis . Only generalized adenopathy may indicate HIV , especially in individuals with risk factors.
Red and white mucous membrane ( erythroplakia and leukoplakia ) in the oropharynx may be a malignant change that is responsible for metastases in the neck. .
Difficulty swallowing may be noted with a thyroid tumor or cancer in various areas of the neck. Hoarseness may be due to cancer of the larynx or paresis of the recurrent laryngeal nerve.
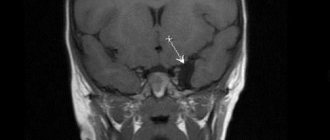
If nasal endoscopy shows changes in the nasopharynx , then tests may include CT or MRI, and a fine needle biopsy of the lesion.
In older patients, especially those who have a risk factor for cancer, additional tests must be done first to determine the underlying cause: a biopsy of the mass may simply reveal undifferentiated squamous cell carcinoma without telling us the source of the disease. These patients should undergo direct laryngoscopy, bronchoscopy with biopsy, and esophagoscopy of all suspicious areas.
CT scan of the facial region of the skull, neck and chest is necessary. If the primary tumor is not found, a fine aspiration biopsy of the mass should be performed.
If the neck mass has been identified as a metastatic and primary tumor, then it should be considered necessary for general anesthesia - biopsy of the nasopharynx, tonsils, base of the tongue, pyriform fossa, larynx, esophagus and bronchoscopy.
Treatment:
Key points:
- A neoplasm on the neck in young patients is usually benign.
- New growths on the neck in old age usually cause cancer.
- The first and main test that guides the otolaryngologist in the right direction for diagnosis in a clinic or hospital is flexible endoscopy using a rhinolaryngoscope with or without local anesthesia. This test is painless and allows the otolaryngologist to examine the nose, nasopharynx, hypopharynx and larynx in detail using video imaging. Read more
- If you have a lump in the neck with a firm, painless, unilateral structure and a diameter of more than 2 cm, urgently consult an otolaryngologist or go to the nearest hospital for examination and diagnosis of possible malignant transformation.
Diagnostics
Therapists are involved in determining the cause of neck swelling. According to indications, patients are referred to otolaryngologists, endocrinologists, maxillofacial surgeons, and other specialists. The examination includes objective, instrumental, and laboratory techniques. The following diagnostic procedures are carried out:
- Questioning, general examination
. A basic study that allows you to establish a preliminary diagnosis and draw up a plan for further examination. Involves studying symptoms, medical history, and assessing external changes. - Sonography
. Ultrasound of the neck is informative when studying the condition of organs and soft tissues, it allows you to identify tumors, areas of inflammation, determine the localization and boundaries of pathological processes. An ultrasound of the thyroid gland is prescribed if an endocrine cause of neck swelling is suspected. Ultrasound of the lymph nodes is recommended for lymphadenitis and cancerous tumors. - Radiography
. To exclude subluxations and vertebral fractures, X-rays of C1 or the cervical spine are prescribed. If there are symptoms of damage to the ENT organs, an x-ray of the larynx is performed. - Other visualization techniques
. CT and MRI of the neck are performed to detail the information obtained during sonography or radiography and make it possible to clarify the location, volume, and nature of the pathological process. - Radioisotope scintigraphy.
Effective in studying the thyroid gland, visualizes nodes, confirms the presence of diffuse changes. - Endoscopic examination of the throat.
Direct and indirect laryngoscopy, microlaryngoscopy, fibrolaryngoscopy are prescribed for lesions of the larynx. According to indications, a biopsy is performed during the study. - Lab tests
. Depending on the existing symptoms, general and biochemical blood tests, examination of the level of thyroid hormones and antibodies to them, microbiological analysis of swabs, punctures, blood samples, cytological or histological examination of a biopsy specimen can be performed.
Neck palpation
Why does my chin hurt?
Traumatic injuries
The most common traumatic cause of the symptom is bruise.
Occurs as a result of a fight or fall. It manifests itself as moderate, gradually subsiding local pain and swelling. The formation of hemorrhages or hematomas is possible. Opening the mouth is not difficult or slightly limited, all manifestations disappear after 1-2 weeks. Hematomas, as a rule, resolve on their own; autopsy is very rarely required. Median, mental and lateral fractures of the body of the lower jaw are the result of intense traumatic effects: a frontal impact, an accident, the fall of heavy objects on the face. The pain is very sharp, intense, and decreases slightly over time. Hematomas and bruises form on the skin. Hemorrhages appear on the mucosa; with an open fracture, bleeding develops. Swelling increases quickly. Stepping of the dentition, mobility and, often, tooth dislocations are observed.
Purulent processes
Due to the characteristics of the skin, the increased oiliness of this area of the face, possible contamination and contact with mechanical irritants, the chin is a favorite location for superficial and deep pyoderma:
- Ostiofolliculitis.
Occurs most often. Initially, an area of redness and slight pain appear, which intensifies with pressure. The pain intensifies, a cone-shaped pustule with a yellow tip up to 0.5 cm in size is formed. Then a brownish crust forms on its own. - Folliculitis.
When inflammation spreads to the entire depth of the hair follicle, folliculitis develops. The symptoms are the same, but more pronounced than in the previous case. The pain at rest is insignificant, bursting, and when touched it is moderate. The pustule ruptures, leaving behind a small ulcer that heals to form a scar or area of hyperpigmentation. - Furuncle.
The purulent infiltrate increases and turns into a cone-shaped purple node. The pain is initially dull, bursting, quickly intensifies, becoming jerking and throbbing. There is extensive swelling. A fluctuation zone is formed. After the pus drains and the rod is rejected, the pain quickly decreases.
Adenophlegmon of the chin is not pyoderma; it develops as a result of suppuration of the submental lymph nodes after dental operations (for example, tooth extraction), with regional lymphadenitis of various origins. The pathology is manifested by a progressive pain syndrome of a bursting, tugging nature. A dense swelling forms on the chin, quickly spreading to nearby areas. Palpation is sharply painful. Severe intoxication is noted.
Osteomyelitis in this anatomical zone is post-traumatic in nature, affecting the body of the lower jaw with open fractures, deep wounds with subsequent suppuration, and the spread of local purulent processes to solid structures. With good drainage, pain is moderate. They intensify with bone involvement and are accompanied by an increase in edema and hyperemia of the wound edges. In the absence of a path for the outflow of pus, the pain quickly becomes unbearable and is complemented by a pronounced intoxication syndrome.
Chin pain
Trigeminal neuralgia
Pain in the chin appears when the third branch of the trigeminal nerve is involved and spreads to the lower lip, lower jaw, gums, and oral mucosa. Painful paroxysms are short-term, but extremely intense, reminiscent of electrical discharges, occur one after another, forcing patients to freeze without moving. Provoking factors for neuralgia include shaving, talking, laughing, chewing, and exposure to cold.
Dental pathologies
Referred odontogenic pain in the chin is detected when 1 premolar, canine and incisors are affected. They are caused by the spread of impulses along the autonomic nerve fibers to the corresponding Zakharyin-Ged zone. They can be aching, drilling, pulling, shooting. Sometimes they develop in the absence of pain in the affected area. They are provoked by tooth extraction, surgical operations, and pulpitis.
Atypical facial pain
The chin is one of the possible localizations of atypical prosopalgia. The pain is deep, aching, dull, debilitating. Sometimes it is painful, but more often it is of medium intensity. Wavy, disturbing often or constantly, intensifies under the influence of external stimuli, and in many patients disappears at night. It is often combined with facial pain in other locations, migraines, and back pain.
Other reasons
Radiating pain in the chin can be disturbing with myositis of the cervical muscles. They appear after hypothermia, are localized along the front surface of the neck, from where they spread upward to the chin and downward to the shoulder girdle. They can be dull or shooting, intensifying with physical activity. In patients with stylohyoid syndrome, the pain is one-sided, dull, occurs under the jaw, radiates to the chin, TMJ, ear, and root of the tongue. When turning the head, the cough becomes stabbing and sharp. Progresses gradually. Complemented by dysphagia, sensation of a foreign body in the throat.
Treatment
Pre-hospital assistance
In case of traumatic injuries, the neck must be secured with a cotton-gauze collar. In other cases, it is recommended to provide functional rest to the neck and not self-medicate, since swelling occurs in many diseases that require different approaches to therapy. In case of intense pain, the use of painkillers is allowed. You should not warm your neck - this can intensify inflammatory and other pathological processes.
Conservative therapy
The conservative treatment regimen includes a protective regimen, etiopathogenetic and symptomatic drug therapy, and physical therapy. The following medications are used:
- NSAIDs
. They are used in the form of tablets, injections, and local remedies. They have analgesic and anti-inflammatory effects. - Antibiotics
. Broad-spectrum medications are prescribed, and after culture results are obtained, medications are replaced taking into account the sensitivity of the pathogen. For extensive purulent processes, combinations of two drugs are recommended. - Antithyroid drugs
. Hyperthyroidism is considered as an indication for the use of medications. For hypothyroidism, replacement therapy is carried out. - Antihistamines
. Necessary for neck swelling caused by allergic reactions.
After eliminating acute phenomena, UHF, laser therapy, electrophoresis with novocaine, and anti-inflammatory drugs are used. Patients with cancer undergo chemotherapy and radiation therapy.
Surgery
For acute pain, blockades with local anesthetics are performed. Taking into account the nature of the pathology, the following operations are performed:
- Traumatic injuries
: transoral fixation, application of a Halo-apparatus, PSO of neck wounds, tracheostomy, chordectomy, resection of the larynx, laryngopexy, removal of foreign bodies of the larynx, reconstructive interventions. - Maxillofacial pathologies
: parotidectomy, opening of abscesses and phlegmons of the neck, dilation of the excretory duct of the salivary gland. - Endocrine diseases
: enucleation of the node, subtotal resection of the thyroid gland, hemithyroidectomy. - Otolaryngological diseases
: removal of a median or lateral neck cyst, opening of a retropharyngeal abscess. - Tumors
: excision of lipomas and fibromas of the neck, removal of the thyroid gland, radioiodine therapy for thyroid cancer, laryngectomy, laryngopharyngectomy, hemilaryngectomy, installation of a voice prosthesis, Krail, Vanach operations.
Causes of swelling under the chin and their symptoms
Chin swelling is not an independent disease, but a symptom of a pathological process in the body. Most often this can be caused by:
Lymphadenitis
Swelling in this disease is often provoked by a viral infection that has entered the lymph nodes. It can also be caused by harmful microorganisms (bacteria) entering the body.
With this disease, a person also experiences a number of additional symptoms, which include:
- Increased body temperature
- Pulsating pain
- Tissue compaction, swelling under the chin in the center,
- Skin redness,
- General weakness.
Important! The most likely infectious diseases that provoke a tumor under the chin: tonsillitis, streptococcal or staphylococcal infection, tonsillitis, laryngitis, purulent tooth abscess, alveolitis, otitis media, sinusitis, chicken pox, mumps (mumps), measles.
Lipoma formation
The causes of this complication are still not fully understood and unknown. This tumor consists of fatty tissue that has begun to grow uncontrollably. It is soft, mobile and painless to the touch. In the initial stages, it can be removed without any consequences. Otherwise, when enlarged, the nerves will be pinched, and the affected area will begin to hurt.
Fibroma
A formation similar to the previous one, causing a condition in which the chin is swollen. The only difference is that fibroma consists of connective tissue, is dense to the touch and does not cause pain.
Atheroma
Subcutaneous infiltrate, which is a clogged sebaceous duct. Dense and does not cause pain in the first stages. However, with its, albeit slow, growth, it can begin to fester and become inflamed.
Read also: Cranberry for edema during pregnancy
Allergy
Swelling of the chin and lower lip or upper lip can be caused by an allergic reaction. Distinctive features are a fairly large area of edema and the absence of pain. Allergens that provoke this condition can be: citrus fruits, chocolate, seafood, medicines, cosmetics, pollen.
The appearance of a subcutaneous pimple
One of the most common causes of swelling on the chin. It manifests itself due to blockage of the sebaceous glands; such compaction often hurts greatly upon palpation.
Cancer metastases
This problem can cause swelling under the chin in all areas (center, side, back of the neck, etc.). This disease takes a long time to develop and in the early stages can be treated, which is more likely to be successful. If you notice some kind of formation that is slowly increasing, consult a doctor immediately to avoid fatal consequences.
Important! Problems caused by malignant tumors develop over a long period. If you find a tumor on your chin and lower lip, which appeared in a short time, then with a high degree of probability this is a benign neoplasm.