The term “antibacterial chemotherapy” refers to the use of chemical compounds prescribed for infectious diseases and causing the death of their pathogens without damaging host tissues.
Unfortunately, many of the drugs developed in the 40-60s have now largely lost their clinical significance, which is due to the evolution of microorganisms and the emergence of their resistance to antibiotics.
This biological phenomenon - antibiotic resistance - determines both the tactics of therapy and the directions of activity of the pharmaceutical industry, which is forced to produce ever new antibacterial drugs, as well as the directions of scientific research to find new groups of drugs that are more effective for treating wound infections.
Wound infection occupies one of the leading places in the general structure of surgical morbidity.
Purulent-inflammatory processes are observed in 35% - 45% of surgical patients. Infection is the cause not only of various surgical diseases, but also of numerous postoperative complications: from suppuration of the postoperative wound to the development of surgical sepsis, which often leads to the death of the patient.
The reasons for the increase in the frequency and course of purulent infection in surgery are diverse and include the following factors: an increase in the volume of surgical interventions, especially in patients at risk, the widespread use of instrumental examination and treatment methods, accompanied by infection of the patient (intravascular and urinary catheters, endotracheal tubes, endoscopic manipulations etc.), the spread of antibiotic-resistant strains of microorganisms. These factors, as well as the irrational use of antibiotics, have led to an increase in the frequency of nosocomial infections caused by multidrug-resistant opportunistic pathogens.
More than half of all antibiotics currently used in the world are betalactams (penicillins, cephalosporins, cephamycins, carbapenems, monobactams).
Data from bacteriological studies conducted in various clinics indicate that pathogenic microorganisms have acquired resistance to long-term antibacterial drugs used in practice (penicillin, streptomycin, ampicillin, amoxicillin, cefazolin, etc.).
The most significant mechanism for the formation of resistance to betalactam antibiotics is the production of betalactamases by bacteria - approximately 80% of cases of resistance of both gram-positive and gram-negative microorganisms are associated with it, which is one of the main reasons for the declining effectiveness of many traditional antibacterial drugs for every hospital.
One of the ways to overcome antibiotic resistance is the use of betalactamase inhibitors in combination with penicillins or cephalosporins as part of combination drugs. Based on the betalactamase inhibitor clavulanic acid, a combination drug amoxicillin/potassium clavulanate was created, based on the betalactamase inhibitor sulbactam, combined drugs ticarcillin/clavulanic acid, ampicillin/sulbactam, cefoperazone/sulbactam were created, and piperacillin/tazobactam was created based on the betalactamase inhibitor tazobactam.
The study of the causative agents of severe surgical purulent complications and their sensitivity to antibacterial drugs allows us to consider the following drugs to be the most effective:
- 3rd generation aminoglycosides (netilmicin, amikacin, sisomycin),
- III-IY generation cephalosporins,
- fluoroquinolones,
- lincosamines,
- imipenem, meropenem,
- antibiotics in combination with betalactamase inhibitors (ampicillin and cefoperazone with sulbactam, amoxicillin with clavulanic acid, piperacillin with tazobactam).
If methicillin-resistant microorganisms are detected - vancomycin, teicaplanin. The long-known antimicrobial drugs – dioxidin and furagin-soluble – retain a fairly high clinical significance.
The choice of an antibacterial drug should be justified not only by the data of bacteriological examination, but also by the severity of the clinical manifestations of intoxication, the severity of multiple organ failure, and the extent of the purulent process.
In case of limited purulent process and absence of clinical and laboratory signs of intoxication, preference should be given to oral forms of drugs.
When a complicated course of wound infection involving internal organs is established, antibacterial therapy should be based only on injection forms. in these cases, all antibiotics should be administered only through catheters installed in the central veins or arteries, in the presence of a purulent process in the lower extremities.
Modern antibacterial therapy for wound infections is based on the requirement of adequate surgical treatment of a purulent focus, supplemented by new antibacterial drugs prescribed rationally and in adequate doses, focusing on the severity of the wound process with regular monitoring of the composition of the microflora in wounds and monitoring the tolerability of the therapy.
In emergency cases, in the absence of the possibility of performing bacteriological studies, the use of antibacterial drugs listed in the programs of empirical and etiotropic antibacterial therapy for patients with wound infection is sometimes allowed (Fig. 30).
HISTORY OF THE DEVELOPMENT OF ANTIBACTERIAL CHEMOTHERAPY
In the development of chemotherapy, three periods can be traced: before the work of P. Ehrlich (before 1891), the period of research by P. Ehrlich and after 1935, when sulfonamides and antibiotics were discovered.
Ehrlich’s theses, formulated on the basis of experience and the logic of search work, remain of enduring importance today: “Chemotherapy sets itself the task of finding substances that, while having a great effect on parasites, would cause as little harm to the body as possible.”
The most important antibiotics for medical practice in the 20th century were discovered either by accident (penicillin) or through so-called targeted screening.
The waste products of fungi and microorganisms (Penicillium, Streptomyces, Bacillus, as well as higher fungi), which have the ability to kill pathogens, are referred to in the narrow sense as antibiotics.
“Looking at the infected wounds, at the people who were suffering and dying, I burned with the desire to find some remedy that could kill germs” (Fleming A., 1881-1995).
Today, every passerby will silently, respectfully bow his head, reading on the gravestone “Sir Alexander Fleming - inventor of penicillin.”
The people of our country will always be grateful to Z.V. Ermolyeva - the creator of domestic penicillin, which saved thousands of lives of the wounded during the Great Patriotic War.
In 1943, the Pharmacological Committee, following the report of Z.V. Ermolyeva makes a decision on the medical use of domestic penicillin. From this date the era of antibiotics began in our country. Z.V. Ermoleva, N.I. Grashchenkov, I.G. Rufanov conducted a detailed study of the effectiveness of penicillin in the treatment of more than 1,200 wounded for two months (evacuation hospital No. 5004).
1943 - treatment and regimens for the use of the first domestic penicillin for 25 “hopeless” and subsequently recovered septic patients were carried out by surgeon Anna Markovna Marshak.
Russian penicillin received its “baptism of fire” on the 1st Baltic Front under the leadership of the Chief Surgeon of the Army N.N. Burdenko.
A student of Z.V. Ermolyeva, S.M. Navashin, academician of the Russian Academy of Medical Sciences, professor, State Prize laureate, director of the State Center for Antibiotics, continued the main directions of her fundamental research in the complex science of antibiotics from the early 50s.
Under the leadership of S.M. Navashin, over a 50-year period, antibacterial drugs of almost all groups were developed at the State Research Center:
- natural, long-acting and semi-synthetic penicillins,
- natural and semi-synthetic aminoglycosides,
- semisynthetic cephalosporins,
- tetracyclines,
- macrolides,
- reserve anti-tuberculosis antibiotics,
- rifampicin and its derivatives,
- lincomycin,
- fusidine,
- antitumor antibiotics,
- polymyxins,
- liposomal forms of antibiotics.
A domestic technology for the most important 1st generation fluoroquinolones has been developed.
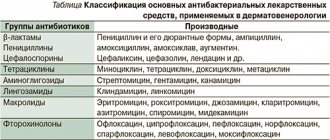
Already in the 70s, the domestic antibiotic industry ranked second in the world, both in volume and in the range of drugs produced. The table in Fig. 1 shows the classification of antibacterial agents.
The “Golden Era” of antibiotic therapy was marked by outstanding achievements in all areas of medicine - a decrease in the spread of infections, the severity of their course and a decrease in the mortality rate from infectious diseases. Gone are the ideas about the incurability of many infectious diseases (sepsis, tuberculosis, endocarditis, many especially dangerous infections, etc.). The effectiveness of antibiotic therapy can be judged, for example, by the mortality rates for pneumonia: before the 40s - 30-40%, after the introduction of penicillin - 5% (S.M. Navashin, 1997).
Diagnosis and treatment of bacterial skin infections
What is the best way to manage a patient with a staphylococcal skin infection? How can a general practitioner diagnose and treat erysipelas? What treatment is effective for erythrasma?
Normally, human skin is populated by a huge number of bacteria that peacefully coexist on its surface or in the hair follicles.
However, the skin has certain properties that protect it from infection by pathogens. These include a dense and dry stratum corneum, practically impenetrable to microorganisms, and an adhesive intercellular substance - a complex mixture of lipids that tightly connects the cells of the malpighian layer and also protects the skin by clogging the entrance to the hair follicles.
Other factors that stop the penetration of pathogenic microorganisms include the constant turnover of skin cells, acidic pH, the presence of immunoglobulins in sweat and various types of skin flora.
Skin infections typically develop only when injury, overhydration, or inflammatory skin conditions compromise these protective properties. Organisms that cause skin infections may be part of the resident flora of the skin or nearby mucous membranes, or may come from external sources such as another person, the environment, or contaminated objects.
Impetigo is the most superficial skin infection caused by S. aulreuls and S. pyogenes. There are two main clinical variants: bullous impetigo, considered a staphyloccal disease, and nonbullous impetigo, caused by S. aulreuls or S. pyogenes or both organisms.
The disease occurs in children much more often than in adults, developing on exposed parts of the body, face and limbs, in places of scratches, abrasions and insect bites.
Initially, red spots appear, which turn into blisters and pustules, which open easily and form thick, adherent yellowish-brown scales on an erythematous base (see Fig. 1). They are often numerous and may be itchy, but are usually painless.
| Figure 1. Thick yellow crusts at the base of erythema and superficial erosions in a patient with streptococcal impetigo. |
With the bullous form, large vesicles and blisters with a diameter of 1-2 cm can develop. They open more slowly and persist for two to three days. Pathogens are usually identified by culture, but this is not necessary in clinically obvious cases.
The most serious complication of impetigo is post-streptococcal acute glomerulonephritis, the overall incidence of which has decreased in recent years.
Bullous impetigo is caused exclusively by S. aulreuls, which secretes the toxin exfoliatin, which causes breakdown of the intercellular substance in the superficial layers of the epidermis. Absorbed in large quantities into the bloodstream, this toxin causes staphylococcal scalded skin syndrome, which is fatal in 5% of cases.
For moderate and localized infections, a topical antibiotic such as mupirocin or fusidic acid is used, and topical neomycin and bacitracin are also effective. The use of licacin gel is very effective.
For severe and widespread forms, a systemic antibiotic is prescribed. Erythromycin or a first-generation cephalosporin such as cephalexin is usually sufficient.
Ecthyma refers to infections that resemble impetigo, but affect the deeper layers of the skin. It is characterized by the formation of thick, adherent scales (see Fig. 2) covering areas of skin ulceration, preceded by the formation of pustules and blisters. The buttocks, thighs and legs are most often affected. The disease is common in the tropics, where poor hygiene and inadequate nutrition contribute to its development. The causative agents may be S aulreuls or S pyogenes, or both microorganisms, but the ulcerations they cause reach the dermis and heal with scarring, which is not characteristic of impetigo. Treatment is with systemic antibiotics targeting S. aulreuls and S. pyogenes.
| Figure 2. Child with extensive foci of bullous (staphylococcal) impetigo on the body |
Superficial folliculitis, boils and carbuncles. Folliculitis (inflammation of the epithelium of hair follicles) is a common dermatological disease, not always primarily of an infectious nature. Physical or chemical trauma, as well as occupational exposure to tar products also used for medicinal purposes, all cause folliculitis.
When staphylococci penetrate into the deeper layers of hair follicles, inflammation seizes the dermis, causing the formation of boils and carbuncles. An inflammatory vesicle with a purulent head (furuncle) develops or the infection covers several nearby hair follicles and an inflammatory conglomerate is formed, from which pus is released (carbuncle).
Boils are most often found on the face and legs, and the typical location of carbuncles is the back of the neck; as a rule, they accompany diabetes mellitus. Large boils and carbuncles are opened and drained, prescribing a penicillinase-resistant antibiotic.
Recurrent staphylococcal skin infections. Some patients are susceptible to recurrent staph skin infections.
Predisposing factors here are diabetes mellitus, chronic renal failure and some immunodeficiency conditions, but most patients do not have the diseases listed above: these patients are probably chronic carriers of staphylococci, and with the slightest injury to the skin, pathogens cause infection.
They try to prevent recurrences of such infections in various ways: by washing the skin with various antiseptics, treating other family members with antistaphylococcal antibiotics and prolonged therapy with other local or systemic antibacterial drugs. All these methods are aimed at destroying the staphylococcal “trail”.
Unfortunately, these measures are usually nonspecific and ineffective, since bacteria reappear soon after the antimicrobial drug is discontinued. Therefore, long-term use of local antiseptics is preferable.
Erysipelas and cellulitis are acute, rapidly spreading infections of the skin and underlying tissues.
The hallmark of erysipelas is a well-defined, raised edge, reflecting involvement of the more superficial (dermal) layers (see Fig. 3). However, cellulite can be located superficially, and erysipelas deeper, so that in many cases these two processes coexist and it is almost impossible to distinguish them.
| Figure 3. A typical lesion of ecthyma on the dorsum of a boy's foot. He developed multiple lesions during his holidays in Bangladesh. |
It is believed that erysipelas is caused by streptococci, usually group A and sometimes groups G and C. For cellulitis, either S. aulreuls alone or together with streptococcus is cultured. H. influlenzae type b is an important etiological factor for facial cellulitis in children under two years of age.
Erysipelas, which typically affects the face, is a disease of the elderly that develops for no apparent reason or sometimes after facial trauma.
Cellulite affects the lower extremities, especially the calf area. It is often preceded by an injury, ulcer or other damage to the skin, where the infection originates.
As with erysipelas, cellulitis may be accompanied or preceded by fever and chills, but many patients do not develop a fever and do not appear seriously ill.
| Figure 4. Well-defined erythematous swelling of facial erysipelas; more often the lesion is bilateral |
The skin is red, hot and swollen, the edges of the inflamed area are uneven, and bubbles and blisters may develop on the surface (see Fig. 4). In rare cases, lymphangitis and regional lymphadenitis are detected.
Without treatment, complications such as fasciitis, myositis, subcutaneous abscess and septicopyemia may develop. Periorbital cellulitis, usually caused by trauma, may be complicated by cavernous sinus thrombosis, orbital, subperiosteal or cerebral abscess formation, or meningitis.
Patients with these conditions must be hospitalized.
The staphylococcal and streptococcal pyodermas described here make up the majority of skin bacterial infections. You need to be able to distinguish between infectious processes inherent in three clinical situations:
- the infection does not fit into the typical clinical picture of pyoderma or does not respond completely to standard therapy;
- the patient’s body is weakened and cannot withstand the fight against infection;
- There is a history of exposure to unusual skin pathogens.
- Infections caused by resident corynebacteria
Erythrasma is characterized by red-brown scaly areas of skin located in the groin, armpits and interdigital spaces (see Fig. 5).
| Figure 5. Bubbles and blisters developing against the background of erythematous edema of the cellulite area of the foot in a diabetic patient |
Corynebacteriulm minultissimulm is considered the etiological factor of this disease, which is asymptomatic and develops, as a rule, in diabetics, obese and elderly people, as well as in those living in tropical climates.
| Figure 6. Brown, scaly, hyperpigmented area of erythrasma in the axilla of a man from Central Asia. The patient has lesions in the groin and between the toes |
Due to the fact that these microorganisms produce porphyrins, in the ultraviolet light of a Wood lamp, the affected areas fluoresce from coral pink to orange-red, which confirms the diagnosis. Typically, no cultivation is required.
Sometimes vigorous washing with soap is enough to cure. Another approach is topical treatment with erythromycin and clindamycin or topical azoles such as clotrimazole, which are active against some Gram-positive bacteria and fungi. For extensive lesions, erythromycin is probably most effective.
Pockmark keratolysis is a superficial skin infection apparently caused by strains of Corynebacteriulm and characterized by the presence of pockmarks 1–7 mm in diameter on the soles of the feet. Pockmarks, merging, can form surface erosions.
The disease is usually asymptomatic, but sometimes patients complain of itchy, burn-like pain or a cheesy smell.
Pockmark keratolysis appears to be associated with excessive wetness of the feet due to tight shoes, frequent contact with water, or excessive sweating.
Treatment of hyperhidrosis, combined with the methods described for erythrasma, is usually effective.
Axillary trichomycosis is characterized by waxy nodules that form in the hair of the armpit. Yellow, red or black, they are formed by large colonies of coryneform bacteria covering the hair cuticle.
First of all, the disease affects patients who pay little attention to personal hygiene and suffer from excessive sweating.
For successful treatment, as a rule, it is enough to shave your hair and use deodorants for your armpits. Topical application of erythromycin and clindamycin is also effective.
References
1. Noble WC Microbal Skin Disease: its Epidemiology. Arnold, London, 1983. 2. Hoor EW, Hooton TM, Horton CA et al. Mircroscopic evaluation of cultaneouls cellulitis in adults // Arch. Intern. Med. 1986; 146: 295-297.
Note!
- For moderate and localized forms of impetigo, both streptococcal and staphylococcal etiologies, a local antibiotic, such as mupirocin or fusidic acid, is sufficient. Topical forms of neomycin and bacitracin are also effective and are often used in combination. For widespread and severe forms of infection accompanied by lymphadenopathy or if there is reason to suspect nephritogenic streptococcal infection, oral antibacterial drugs that act on both microorganisms, such as erythromycin, are indicated
- Some patients are susceptible to recurrent staphylococcal skin infections. Predisposing factors such as diabetes mellitus, chronic renal failure and some immunodeficiency conditions are absent in most patients. The method of choice is long-term use of local antiseptics
- Erysipelas, usually localized on the cheeks, is streptococcal in nature. It is most common among older patients and develops either for no apparent reason or, in rare cases, sometimes after facial trauma. The drug of choice is penicillin; in more severe cases, benzylpenicillin is prescribed intravenously at 600-1200 mg.
- Erythrasma appears as red-brown patches of skin covered with scales in areas of diaper rash, such as the groin, armpits and interdigital spaces. Intensive washing with soap is sometimes enough to cure. Another approach is topical treatment with erythromycin and clindamycin or topical azoles such as clotrimazole, which are active against some Gram-positive bacteria and fungi. For extensive lesions, erythromycin is probably most effective.
ANTIFUNGAL DRUGS
Patients with wound infections receiving long-term antibiotic therapy with several drugs at once are a group at high risk of developing mycotic infections. The mortality rate for invasive mycoses caused, for example, by fungi of the genus Candida, reaches 85%. Candidiasis, being an endogenous infection, can manifest itself as a clinical manifestation of fungal damage to the brain, liver, spleen, kidneys, heart, lungs, and joints. For treatment, the doctor has only five effective antifungal drugs: amphotericin B, fluconazole, itraconazole, flucytosine and liposomal amphotericin B.
The first two are most widely used in clinics: amphotericin B and fluconazole. However, despite the high clinical efficacy of amphotericin B, this drug is used much less frequently in the treatment of candidemia due to its toxic effects on the kidneys. Liposomal amphotericin B is less toxic and more convenient to use, since it can be administered through peripheral veins. Fluconazole is considered the drug of choice for candidemia, wound infection, peritonitis, urinary tract infection
EUBIOTICS FOR THE PREVENTION OF DYSBACTERIOSIS IN PATIENTS WITH WOUND INFECTION
Long-term antibiotic therapy, radiation therapy, hormonal and chemotherapy inevitably lead to significant qualitative and quantitative changes in the composition of normal human microflora. To prevent endogenous infection in seriously ill patients, selective decontamination of the digestive tract is used. Oral or intragastric administration of antibiotics that are not absorbed in the intestine is used. For wound infections, if the clinical situation allows, preference is given to chemotherapy drugs for local use. In the prevention and treatment of dysbacteriosis in wound infections, the emphasis is currently on the use of bacterial biological preparations from normal microflora, i.e. the use of eubiotics made on the basis of bifidumbacteria, lactobacilli, Escherichia coli, and spore forms of bacteria. Recent studies have established the high effectiveness of the biological product “Bifiliz” (a combination of lysozyme and bifidumbacterin).
To maintain normal intestinal ecology, it is necessary to include probiotics in complex treatment.
- monocomponent (bifidumbacterin, lactobacterin, colibacterin, sporobacterin, bactisporin, bactisubtil, etc.);
- multicomponent (bifilong, acylact, acinol, linex, biosporin);
- combined (bifidumbacterin forte, bifiliz).
ROUTES OF ANTIBIOTIC ADMINISTRATION
The effectiveness of the antibiotic depends on the creation of a high concentration in the lesion, which is achieved by prescribing the appropriate dose of the drug and administering it in the optimal way.
In the case of a local purulent infection, in order to stop an acute purulent process, it is sufficient to use one antibacterial drug with mandatory local treatment of a purulent wound under bandages with ointments on a polyethylene glycol basis, which have a wide spectrum of antimicrobial activity, or modern iodophors, dioxidine, which enhance the antimicrobial effect of drugs prescribed for general antibacterial therapy.
In case of extensive purulent foci or sepsis, it is necessary to increase the dose of antibiotics to the maximum, taking into account the species composition of the microflora isolated from different biological environments. It is advisable to use combinations of 2-3 drugs. The drugs must be administered through catheters installed in the central veins, which allows, when treating generalized forms, to create and long-term maintain at the required level the concentration of the antibiotic not only in the lesion, but throughout the patient’s entire body.
When the purulent focus is localized on the lower extremities, intra-arterial administration of drugs into the inferior epigastric artery using round-the-clock infusion using perfusors is effective.
Long-term intra-arterial infusion allows you to create and maintain a sufficiently high concentration of drugs in the tissues of the injured limb, while leaving the concentration of antibiotics in the general bloodstream at a lower level. This helps to increase the effectiveness of antibacterial therapy and reduces the possibility of overall toxic effects of antibiotics.
Purulent wound - symptoms and treatment
An infected wound should be treated immediately. It requires an integrated approach, i.e. it must affect both the wound and the body as a whole.
To combat the causative agent of wound infection, use:
- antibacterial drugs;
- antiseptics (miramistin, chlorhexidine, prontosan, betadine);
- immunological preparations (pentaglobin, gabryoglobin, imbioglobulin).
On the first day, empirical antibacterial therapy (amoxicillin/clavulanic acid, ciprofloxacin) is most often prescribed. Therapy is then adjusted depending on the results of bacterial cultures, taking into account the sensitivity of the identified infection to antibiotics. In addition to antibacterial drugs, patients are prescribed bacteriophages (viruses that selectively kill bacterial cells).
Also, in the case of a purulent wound, a comprehensive detoxification of the body :
- hemodilution - dosed dilution of blood with plasma-substituting fluids;
- accelerated neutralization, destruction and elimination of toxins, metabolites and biologically active substances using forced diuresis (increased urine volume), intravenous administration of solutions and blood purification methods - plasmapheresis, hemofiltration and hemodialysis.
Symptomatic therapy includes pain relief and correction of damaged organs and systems.
In addition to surgical treatment, wound drainage . It allows you to improve the outflow of pus. To do this, various tubes, half-tubes and glove drains are installed in the damaged area.
Hypertonic solutions, hydrogels, proteolytic enzymes in the form of powders or solutions, UHF therapy, various methods of cavitation (ultrasonic exposure), plasma and laser treatment of the wound can be used locally to cleanse the wound. In particular, proteolytic enzymes, acting as a “biological scalpel,” help remove dead tissue from the wound [14].
Treatment of a purulent wound should only be carried out under the supervision of a physician, since the drugs used can cause an allergic reaction [6].
To stimulate regeneration, zinc-containing ointments, vitamins, ultraviolet irradiation, sea buckthorn and rose hip oil are used. The method of applying secondary sutures is also widely used . They are applied only after the wound has been cleansed of pus. To speed up healing and prevent the formation of a hypertrophic scar, it is possible to use a laser, a pulsating magnetic field and electrophoresis with lidase (a special enzyme).
Modern treatment methods include systemic ozone therapy . It improves the utilization of oxygen in the body, has a detoxifying and immunostimulating effect [16].
There are several methods of ozone therapy. The most commonly used in the treatment of purulent wounds include:
- external use of a gaseous ozone-oxygen mixture (direct exposure to a device that supplies ozone to the wound);
- the use of special caps with normal or reduced gas pressure (for example, “ozone boots” - the limbs are placed in a hermetically sealed plastic bag, into which an ozone-oxygen mixture is then supplied at a certain pressure for 15-30 minutes).
Hyperbaric oxygenation (HBO) has also shown good results in the treatment of purulent wounds . It is carried out in special medical pressure chambers: the patient is placed for a certain period of time in a pressure chamber containing oxygen under high pressure. In addition to eliminating tissue hypoxia (lack of oxygen), HBOT suppresses the proliferation of anaerobic bacteria and destroys aerobic bacteria. This method also reduces the formation of toxins and increases the body's immunity.
Dermoplastic surgeries are used:
- with extensive defects against the background of a satisfactory general condition of the patient;
- after cleansing the wound;
- in the absence of inflammation and circulatory disorders in the tissues surrounding the wound;
- when bright granulations appear (young connective tissue with an abundance of blood vessels);
- in the presence of a small amount of serous discharge from the wound;
- when self-healing is impossible.
There is full-thickness skin grafting, which allows you to completely restore the skin, providing good cosmetic and functional results. It is divided into plasty using local tissues and a displaced skin flap (Indian plasty, Italian plasty on a feeding pedicle, as well as microvascular plasty techniques). These methods of surgical wound closure are not always feasible (for example, with extensive soft tissue defects, localization of wounds in sedentary areas of the skin). Therefore, in some cases, plastic surgery with a free split skin flap is used [12]. After this operation, the wound heals through a scar - the skin is not completely restored.
The choice of skin grafting method is carried out taking into account the type and location of the wound, the individual characteristics of the patient, the condition of the surrounding skin and the nature of the tissue.
The modern and most effective method of treating purulent wounds is the VAC (vacuum therapy) method [18]. Due to the effect of negative pressure on the bottom and edges of the wound, it accelerates the formation of granulation tissue, improves local blood supply and reduces swelling. All this promotes rapid wound healing and enhances the effect of drug treatment [20].
Vacuum therapy is carried out as follows:
- to begin with, dead and damaged tissue is completely removed from the wound;
- the cleaned wound cavity is filled with special foam (polyurethane sponge);
- a drainage tube is attached to the surface of the sponge to remove air and exudate;
- to fix the bandage and maintain the vacuum, the resulting structure, together with the edges of healthy skin, is covered with an adhesive transparent film;
- the drainage tube is connected to an aspirator (VAC device), which creates the required level of pressure and draws fluid from the wound [19].
Unlike aseptic gauze dressings, which need to be changed every day, vacuum dressings can be left in the wound for 3-7 days. Due to their tightness, they reduce the risk of new infection [17]. In this case, the destruction and removal of pathogenic microorganisms occurs two times faster than with other methods of treating a purulent wound [20].
Contraindications to vacuum therapy:
- incomplete cleansing of the wound;
- osteomyelitis (inflammation of bone tissue);
- blood clotting disorder;
- malignant tumor in the wound;
- skin fistulas;
- allergic reaction to the components used [20].
DURATION OF ANTIBACTERIAL THERAPY
In case of local purulent process, administration of an antibiotic for 3-5 days is sufficient. Longer therapy is carried out in groups of patients with acute purulent diseases of soft tissues, with generalization of the infectious process. The criterion for the need to continue therapy or discontinue drugs should be bacteriological control data, as well as the dynamics of clinical indicators.
The main criteria for discontinuation of therapy are the disappearance of pathogenic microflora from the purulent focus or a decrease in the number of microbes in 1 g of wound tissue, clear positive dynamics of clinical and laboratory parameters of the wound process, normalization of temperature, improvement in the general condition of the patient, etc.
Early withdrawal of antibacterial therapy before achieving a stable clinical effect can lead to relapse or protracted course of the disease and significantly complicate further treatment.
Reasons for visiting a doctor
You should consult a doctor if the wound or abrasion is accompanied by problems. In the following cases, you should definitely visit a specialist:
- The wound was caused by a rusty object - it could be a simple nail, but in such cases a tetanus vaccine may be required.
- If the edges of the wound diverge greatly and require suturing. If stitches are not applied, the result will be a strong and deep scar, and healing will be slow.
- If the wound is accompanied by severe bleeding that cannot be stopped within 20-30 minutes. In such cases, either blood clotting may be impaired or a large and important vessel may be damaged.
- If the area around the wound is very swollen, swelling and suppuration appear, all this is accompanied by twitching pain and fever. In such cases, surgical debridement and, probably, drug therapy are necessary, since the symptoms indicate infection of the wound.
IMPORTANT : even the smallest and most insignificant wound is a violation of the skin, which pathogenic microbes and bacteria can use as an entrance gate. Tetanus bacteria are especially dangerous. Be sure to treat everything, even minor abrasions and cuts.
STEP ANTIBACTERIAL THERAPY FOR WOUND INFECTION
Currently, antibiotics are produced in dosage forms intended for both parenteral administration and oral administration (for example, ofloxacin, ciprofloxacin, pefloxacin, etc.)
The presence of two dosage forms of the same drug allows them to be used sequentially (first parenterally and then orally). Focusing on the dynamics of the clinical signs of the wound process, it is possible to reduce the time of administration of the drug parenterally and switch to oral administration, which significantly reduces the total costs of treatment (consumables, labor costs of medical staff), improves the comfort of treatment, and shortens the length of the patient’s stay in the hospital.