A benign neoplasm, which is formed from the synovial (articular) membranes, is called “hygroma” or “tendon ganglion”. This bulge inside is filled with mucus and fibrin protein strands. The tumor can appear on any joint (fingers, hands, feet).
Hygroma on the finger is one of the most unpleasant types of pathology. As a rule, the formation appears near the distal joints between the phalanges or in the area of the flexor muscles. The lump looks unsightly and causes pain. If left untreated, the mobility of the joint worsens and the nail becomes deformed.
Types of hygroma
A synovial cyst is usually located in the tendon sheath or joint capsule. It looks like a ball with a soft, flesh-colored consistency. Inside the formation there is serous fluid, mucus, and fibrin protein fibers.
Reference. A cyst of the phalanx of the thumb rarely causes discomfort. A mass in the knuckle of the index, middle, or little finger can limit mobility.
The tendon ganglion never becomes malignant, but requires proper therapy. Otherwise, the likelihood of spontaneous opening increases, which threatens the formation of new tumors.
Finger hygromas are divided into types according to location, number of capsules formed and type.
Types of synovial cysts depending on the number of capsules:
- Single-chamber are single growths.
- Multilocular – multiple tumors.
Types of formations by capsule type:
- Valve. In the area where the capsule connects to the maternal shell, a valve is formed, as a result of injury to which the viscous contents flow out or in from time to time.
- Anastomosis. The cyst cavity connects to the joint, while its contents periodically flow out and fill the maternal membrane.
- Isolated formation. The cavity of the tendon ganglion is separated from the maternal membrane.
Hygroma of the finger appears relatively rarely; it is often confused with nodes that form in rheumatoid arthritis, osteoarthritis, and rickets. To determine the nature of the tumor, you need to conduct a thorough diagnosis.
How to recognize the disease?
The following changes indicate the development of a bone in the leg:
- the thumb deviates outward, while forming a “ball” at its base;
- there is constant aching pain in the area of deformity;
- fast fatiguability;
- difficulties with choosing shoes.
In the absence of treatment and progression of the pathology, a hammer-shaped shape of the remaining toes is observed. The appearance of the slightest signs of disease should be a reason to contact an orthopedist.
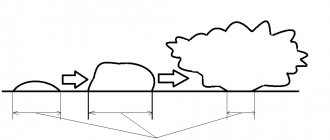
Formation mechanism
A synovial cyst is formed in this way:
- The elasticity and endurance of damaged tissue decreases.
- The joint is unable to retain joint fluid.
- The contents of the synovial membrane are poured into the surrounding tissues.
As a result, an elastic and dense tumor-like formation appears, filled with thick liquid inside.
Doctors still cannot accurately answer the question of why a synovial cyst occurs. However, they identify several factors that can trigger the appearance of a lump:
- Hereditary predisposition. If close relatives had a hygroma on the finger, then the likelihood of its occurrence in the child also increases.
- Systematic load on the hands.
- Inflammatory diseases and injuries (microtraumas, bruises, sprains, dislocations, fractures) of tendons and joints.
- Metaplasia is the pathological replacement of normal tissues with abnormal ones.
- Excessive tension in the arm muscles.
- Calluses on the fingers that appear regularly.
- Lack of adequate treatment for finger injuries and diseases.
Finger hygromas, which form after injuries, are diagnosed in 30% of patients. Tumors that are inherited occur in 50% of cases. In other cases, growths are formed due to repeated injuries and constant overstrain of the damaged area.
Reference. Tendon ganglion most often appears in women between 20 and 30 years of age. In children and the elderly, pathology is observed extremely rarely.
Symptoms
A synovial cyst is a dense, elastic formation with a smooth surface in the shape of a ball. The tumor shell is attached to the surrounding tissue, so it does not move. But sometimes during palpation you can notice that the growth moves.
When you feel the cyst, you may feel clots, cholesterol crystals, and “rice bodies” inside. They are quite mobile, often changing their position. Usually, when you press on the tumor, there is no pain or minor discomfort.
Reference. If painful sensations occur during palpation, this indicates that the pathology has become chronic. The formation increases gradually; at the early stage, there are no pronounced unpleasant sensations.
Hygroma on the finger has the following external signs:
- spherical shape, size - about 5 cm, sometimes more;
- the surface of the cyst is elastic, smooth;
- when pressing, a slight nagging pain appears in the area of the damaged joint;
- the skin over the tumor is thick and rough;
- During the inflammatory process, the skin turns red.
Symptoms depend on the stage of the pathological process: at first there are no pronounced signs, and in advanced cases they are clearly expressed. Clinical manifestations of hygroma (early stage):
- tumor size – from 5 mm;
- the cyst is inactive;
- the growth is soft, elastic;
- there are no painful sensations;
- the skin over the capsule is smooth and even.
The hygroma on the finger is practically invisible. At first, the tumor does not affect surrounding structures and is not accompanied by other pathologies.
Symptoms of an advanced stage of pathology:
- growth size – from 10 cm;
- when palpated, the tumor practically does not move;
- the cyst is dense and hard;
- nagging or sharp pain, which sometimes radiates to the arm;
- the skin over the cyst turns red, becomes rough, rough.
The hygroma on the finger is clearly visible, as its size has increased. It compresses the surrounding nearby joints, nerves, tendons, and blood vessels. The pathology is accompanied by limited mobility in the affected joint, numbness, tingling, redness of the skin, inflammatory, purulent process.
Types of hygroma
As we mentioned above, hygroma can occur in the form of a single formation, delimited from other tissues by a membrane. It is also possible for several cysts to appear, fused or independent of each other.
However, most often the disease is classified according to the location of the lump. So, doctors distinguish the following types of it:
- hygroma of the wrist joint
; - hand hygroma
; - hygroma on fingers
.
Much less common:
- hygroma of the knee joint
(formed in the knee fossa, also known as Becker’s cyst); - hygroma of the ankle joint
; - hygroma of the foot
(located on the dorsal, i.e., upper, side of the foot, usually at its outer edge).
The tendon ganglion, located in the wrist and hands, accounts for up to 88% of the total number of cases of the disease. The ankle joint and foot bothers up to 11% of patients who suffer from hygroma. A synovial cyst in the neck, shoulder, shoulder blade or knee occurs in only 1% of patients. It is extremely rare for patients to see a doctor with formations in the bones, muscles or spine.
Hygroma of the wrist
Hygroma of the wrist joint
- the most common type of synovial cyst. It becomes clearly visible in a bent position of the wrist joint (for visual diagnosis, you need to move the hand forward and back, and then left and right). Often, hygroma of the wrist joint is located on the front or back side of the joint, but it can also grow on the lateral surfaces or at the very base of the palm.
If the lump is located under the ligament, it may not cause any concern and may not even cause any aesthetic discomfort.
As a rule, the consistency of hygroma of the wrist joint is felt as soft or springy, “rubbery”.
Hygroma of the hand
Tendon ganglion in the hand area
(hygroma of the hand) usually occurs on the fingers (from the side of the palm), the palm itself, the back of the hand, or closer to the wrist joint. Typically, hand hygroma does not bother the patient until it reaches a large enough size and does not interfere with everyday activities.
Hygroma on the finger
Synovial cyst on fingers
often occurs on their back side, in the area of the distal phalanx (i.e., the last one on which the nail is located). Often it is located in close proximity to the cuticle or nail fold.
The skin over the hygroma on the finger, as a rule, looks thinned, stretched, and its natural pattern is smoothed out. Under the skin, as a rule, a rounded formation can be easily felt, which does not cause pain, except in case of injury. It is quite dense to the touch, so it can be perceived as a bone or cartilage growth.
Hygromas on the palmar side of the phalanx are usually larger than on the back, and can spread to the entire phalanx and even occupy the adjacent one. They can be quite painful due to compression of the nerves that run along the sides of the fingers. This type of hygroma often prevents patients from performing household chores.
Ganglions also appear at the proximal phalanges
(near the base of the finger). Such cysts are also quite painful, despite their small (about the size of a pea) size. Pain with a hygroma on the finger usually occurs when trying to tightly grasp a hard object (for example, the handle of a shovel, a rolling pin, etc.).
Hygroma of the lower extremities
Synovial cysts of the lower extremities are typically localized on the back of the foot or fingers, as well as on the front of the ankle joint. Such hygroma rarely bothers patients with pain. As a rule, discomfort occurs when the foot is compressed by tight shoes, the foot is rubbed or stuffed, and also when the lump is located in close proximity to the nerve.
Hygroma of the lower extremities
Establishing diagnosis
If a patient notices a suspicious tumor on his finger, he should contact a traumatologist, surgeon or orthopedist.
Reference. The specialist will conduct a differential diagnosis to distinguish the hygroma from the leak (capsule with purulent contents), ganglion (nerve ganglion), epithelial cyst, chondroma (cartilaginous tumor), osteoma (bone tumor), aneurysm (protrusion of the artery wall), malignant formations, etc. d.
First, the doctor collects anamnesis, conducts a visual examination, and palpates the neoplasm.
To clarify the diagnosis, the patient is prescribed the following studies:
- Ultrasound helps evaluate the structure of the formation.
- Magnetic resonance imaging and computed tomography are performed if nodular structure is suspected.
- X-ray.
To analyze the contents of the formation, a puncture is performed. During the examination, the pathological formation is punctured, the necessary cellular material is collected, and then it is studied in the laboratory.
To clarify the diagnosis and create an effective treatment regimen, doctors prescribe the following tests:
- Clinical examination of blood and urine.
- Biochemistry of blood.
- X-ray of the lungs.
- Tests to detect sexually transmitted infections, hepatitis, HIV.
- Electrocardiography.
Once the diagnosis is made, treatment is necessary.
Hygroma removal
Causes of hygroma formation and symptoms of the disease
The etiology of the development of this pathology is not fully understood. However, there are basic assumptions for the formation of hygromas, such as:
- excessive loads on the joints, as well as frequent trauma to the distal bone joints;
- hereditary predisposition to connective tissue diseases;
- increased secretion of synovial fluid (for example, in autoimmune diseases);
- other inflammatory processes of articular elements or nearby tissues (bursitis, tenosynovitis).
A synovial cyst (hygroma) is most often localized on the dorsum and palmar surface of the wrist, less often on the foot, in the area of the phalanges of the fingers and other joints. Visually, at the initial stage of development, the formation resembles an oval protrusion the size of a pea, which gradually increases, has a soft, densely elastic consistency and over time can significantly increase in volume. The skin over the formation remains unchanged.
Typically, the development of hygroma is not accompanied by pain or any discomfort (if you do not take into account the appearance). However, in an advanced form or with long-term development of the pathology, an inflammatory process of the synovial cyst can be observed, which is accompanied by pain, swelling of the tissues, numbness of the distal parts due to local disruption of innervation and blood circulation.
Diagnosis of the disease
To make a diagnosis, a traumatologist performs a visual examination and palpation of the affected area.
However, in some cases, in order to exclude diseases with similar clinical manifestations (secondary manifestations of rheumatoid arthritis (Heberden’s and Bouchard’s nodes), fibromatous formations, small lipomas, molluscum contagiosum, ecchondromas, osteomas, osteosarcomas), additional methods for determining the morphological structure of the formation will be required:
- Ultrasound – allows you to clearly differentiate and structure formations of non-osseous origin from cysts, as well as perform topical preoperative preparation;
- - one of the most informative research methods for bone formations, providing an accurate amount of information about the pathological process;
- X-ray is the most common and inexpensive method of examination to determine the nature of the bone abnormality;
- puncture biopsy - performed by an oncologist in cases of suspected malignant tumor.
Surgical treatment of hygroma
In the absence of contraindications and the topical location of the formation is clarified, the doctor proceeds to surgically remove the hygroma. This operation can be divided into the following stages:
- preparation for surgery: processing of the surgical field, marking the future surgical approach;
- carrying out anesthesia. Most often, local anesthesia is used, but in difficult cases, with a deep formation with access to the joint or articulation of the bones of the wrist, general anesthesia is used;
- depending on the size of the formation and the depth of its occurrence, the doctor can first pump out the serous fluid from the synovial cyst and then excise it, or remove the entire hygroma along with the contents. An important point is the complete removal of the hygroma capsule. Incomplete removal of the capsule may cause recurrence of the pathology and lead to reoperation. The removed material must be sent for histological examination to exclude any possible oncological pathology;
- the doctor inspects the postoperative wound with careful hemostasis (stopping bleeding) and layer-by-layer restoration of the tissues dissected during access;
- step-by-step treatment of the surgical wound with an antibacterial solution with sutures (sutures are removed after 14 days);
- fixation of the joint (stabilization of the operated joint) with a splint bandage for a period of 1 to 2 weeks.
After removal of the hygroma, subsequent treatment is carried out on an outpatient basis, under the supervision of an operating doctor. If necessary, the doctor can prescribe a set of rehabilitation measures.
During the rehabilitation period, it is extremely important to limit the load on the operated limb segment. After removing the sutures and splints, in order to prevent the adhesive process of contracture, which can lead to a decrease in the function of the operated area, it is recommended to perform special gymnastic exercises (physical therapy) under the supervision of specialists, as well as undergo an appropriate course of physiotherapeutic treatment: magnetic therapy, laser therapy, phonophoresis with hydrocortisone, UVT therapy. Sanatorium-resort treatment of diseases of the musculoskeletal system is also considered an effective method of rehabilitation.
Treatment
Conservative therapy
Treatment of finger hygiroma at an early stage is carried out using medications and physiotherapy. The patient should refuse physical activity.
Reference. Conservative treatment is associated with frequent relapses.
Medicines are used for non-purulent inflammation:
- Nimesil is a non-steroidal anti-inflammatory drug.
- Diclofenac in the form of an ointment demonstrates a pronounced analgesic and anti-inflammatory effect.
- Clemastine in tablet form is an antihistamine that accelerates the destruction of histamine and reduces its concentration in tissues.
Physical therapy is carried out to reduce the size of the tumor, relieve or eliminate inflammation that has arisen due to compression of the surrounding tissues by the formation.
For hygroma, the following physiotherapeutic techniques are used:
- Deep heating of tissues with high frequency and intensity current. After the procedure, the inflammatory process is alleviated, blood circulation is normalized, and tissue restoration is accelerated.
- Ultrasound therapy improves blood circulation in small vessels, reduces the tone of striated and smooth muscles. Under the influence of ultrasound, more oxygen enters the tissues, and they recover faster.
- Magnetic therapy weakens the inflammatory process in cartilage and bones.
- Balneotherapy is treatment with mineral waters (sodium chloride, radon, hydrogen sulfide baths). After the procedures, adhesions and structures become softer, lengthen, and the severity of the inflammatory process decreases.
In addition, electrophoresis with glucocorticosteroids, radiotherapy, mud or paraffin wraps are used to eliminate the tumor.
To remove the tendon ganglion without surgery, a puncture is prescribed. To do this, the joint capsule is punctured, the contents of the cyst are pumped out, after which the cavity is treated with antiseptics or glucocorticosteroids (Diprospan). If the hygroma becomes infected, antibacterial drugs (Neomycin, Amicil) are injected into its cavity after aspiration (suction of the contents). The puncture is performed under local anesthesia, so the patient does not feel pain.
After the procedure, a pressure bandage and an orthosis (a medical device that relieves stress on the joints) are put on the affected area. During the rehabilitation period, it is forbidden to subject the finger to stress.
The most dangerous methods include crushing the hygroma. During the procedure, the doctor squeezes the tumor with his hands or plastic objects. When the membrane ruptures, the fluid spreads throughout the surrounding tissues, which is accompanied by intense pain.
Carefully. Crushing a hygroma is a painful method that provokes dangerous complications (inflammation, suppuration) and frequent relapses. After the procedure, the cyst shell remains inside, so the risk of new ganglia forming is high.
Surgical intervention
If conservative treatment is unsuccessful, which happens in most cases, then doctors prescribe surgery.
Bursectomy is an effective method for removing finger hygroma.
It is necessary to treat the growth surgically in the following cases:
- Education is increasing rapidly.
- Painful sensations occur that intensify during movement.
- The mobility of the joint is limited.
- Aesthetic discomfort.
Removing the growth lasts no more than 30 minutes. The area around the tumor is numbed. The surgeon excises the formation along with the membrane and fluid and carefully separates it from the joint. Then stitches are placed on the surgical wound and removed after 7–10 days.
Reference. If the tumor is large, then bursectomy is performed under general anesthesia in the hospital.
Laser treatment is an effective alternative to classical surgery. The procedure is performed under local anesthesia, so there is no pain.
Using a laser beam, the skin over the cyst is cut, and the membrane with liquid is removed. Then the cavity is treated with antiseptics, stitches are placed on the wound, and the top is covered with a sterile bandage to prevent infection.
After treatment, the affected joint is fixed with brace and immobilizing plaster orthoses. They are comfortable and do not interfere with joint mobility.
Reference. After laser removal of hygroma, there are no scars. The procedure lasts approximately 15 minutes, after which the patient can go home.
Alternative Treatment
In the early stages of development of the tendon ganglion, you can use traditional medicine (complex therapy). They will not replace traditional treatment, but can speed up recovery.
Folk remedies against synovial cysts:
- Take a copper coin, heat it on a fire, and dip it in an aqueous solution of salt. Then bandage it to the damaged area. After 3 days, remove the bandage, rinse your finger and repeat the procedure.
- Take a piece of the jellyfish’s body and secure it on your finger with a bandage. After 3 hours, remove. Repeat the procedure every day. Kombucha can be used in the same way.
- Grind the cabbage leaves using a blender or meat grinder, squeeze out the juice through cheesecloth. Drink it 200 ml per day for 4 weeks.
- Squeeze the juice from celandine leaves (25 ml), apply to the tumor, after steaming your finger in hot water. Bandage it, cover it with cling film, and then wrap it in a warm cloth. Treatment lasts about 20 days.
There are many more recipes for the treatment of pathology, but they can only be used after the approval of a doctor.
Prevention
To prevent cyst formation, you must follow the following rules:
- If there is a hereditary predisposition to hygroma, you need to avoid injuring your hands, protect your joints, and limit monotonous mechanical loads on your hands.
- During physical work, distribute the load evenly between your hands. If you regularly engage in such activities, then use elastic bandages.
- Treat tendovaginitis (inflammation of the tendon sheath) and bursitis (inflammation of the mucous bursae of the joints) with a chronic course in a timely manner.
The latter pathologies often cause the appearance of a tumor.
As you can see, finger hygroma is not a dangerous pathology. But in order to avoid unpleasant consequences, you need to seek medical help in time and carry out competent therapy. You should not self-medicate, as this will only worsen your condition.