The penis, or penis, is an organ of the male genitourinary system. It performs a double function: the urethra passes through the thickness of the penis, through which urine and sperm are excreted. Anatomically, the penis has the following parts:
- The body, which starts from the trunk and passes from the front to the head.
- The glans is the terminal part of the penis, covered with thin, sensitive skin.
- The foreskin is a fold of skin that runs transversely in a circle and protects the head.
- The frenulum is a fold of skin that runs from below the head in the longitudinal direction and connects it to the skin.
Inside the penis there are two cavernous bodies - during sexual intercourse they fill with blood and provide an erection - and one spongy body - the urethra passes through it.
Is there such a thing as penile cancer? Penile cancer refers to malignant tumors that develop from the skin that covers it. They are rare. According to American and European statistics, penile cancer is diagnosed in one in 100,000 men every year, accounting for 1% of all cancers in men.
Causes and risk factors for penile cancer
The exact causes of penis cancer are unknown, but doctors and scientists know about some risk factors:
- Human papillomavirus. The pathogen is sexually transmitted and many people are currently infected. There are more than a hundred types of HPV. Only a few of them are dangerous. In women, they increase the risk of cancer of the vagina and cervix, in men - the risk of penile cancer (viruses of types 16 and 18 are found in patients).
- Promiscuous sexual intercourse. Apparently, this factor is directly related to human papillomavirus infection. Research shows that men who have had two or more sexual partners before the age of 20 have a 4-5 times increased risk.
- Age. The disease mainly occurs in men over 50. Before the age of 40, penile cancer is extremely unlikely to develop.
- Smoking . Tobacco smoke contains carcinogens that penetrate into the blood and can cause mutations in the DNA of cells in any organ. In addition, smokers have worse local defense mechanisms, so they are more likely to become infected with HPV.
- Immunodeficiency states. The immune system destroys not only pathogenic viruses and bacteria, but also defective ones, including cancer cells. If the immune system does not work well, the risk of any cancer increases.
- Phimosis . This is a condition in which the foreskin narrows and prevents the head of the penis from being exposed. According to statistics, men with phimosis are more often diagnosed with penile cancer.
If a man has any risk factors from this list, this does not mean that he will necessarily develop a malignant tumor. At the same time, sometimes the disease is diagnosed in men who do not have any risk factors.
1.General information
The term “polyp” in medicine refers to the growth of tissue in an area where nature does not provide any bulges. Polyps (for example, in the intestines, nose, etc.) are benign neoplasms. Often they do not manifest themselves in any way, and are discovered purely by chance, during a preventive or diagnostic examination for another reason. However, when they reach a certain size, polyps can cause serious problems associated, in particular, with pressure on surrounding tissues, the risk of traumatic injury and malignant degeneration.
All of the above fully applies to such an unpleasant formation as a urethral polyp. The urethra, or urethra, is the terminal portion of the urinary tract; Through the external opening of the urethra, renal filtration waste accumulated in the bladder is evacuated from the body to the outside. Any interference along this path complicates the passage (free flow) of urine, which ultimately leads to dysfunction and pathological changes in the entire genitourinary system, and sometimes, if the lumen of the urethra is completely blocked and the so-called develops. acute urinary retention creates a direct threat to life.
The peculiarities of the anatomical structure of the male and female body determine significant differences in the distal (most distant) segment of the urinary tract: in women, the urethra is thicker, straighter and several times shorter. This circumstance makes the female urethra, in general, more vulnerable to diseases, primarily infectious ones. Urethral polyps are also much more common in women than in men. In addition, polypous growths on the internal mucous surface of the urethra in male patients are usually detected deeper, i.e. closer to the bladder, namely in the part of the urethra that passes through the prostate.
However, in representatives of both sexes, a polyp can develop directly in the external opening, where it is, of course, easier to detect.
A must read! Help with treatment and hospitalization!
Symptoms of penile cancer
Sometimes penile cancer does not cause symptoms. A malignant tumor may be indicated by such signs as strange spots and rashes, thickening of the skin, ulcers, accumulation of contents with an unpleasant odor under the foreskin, bleeding from the urethra or from under the foreskin, lumps, warts. One of the possible symptoms of cancer of the head of the penis is its swelling. The “bump” in the groin may be enlarged due to damage to the lymph node by cancer cells.
All of these signs do not necessarily indicate penile cancer. This is how other, less dangerous diseases can manifest themselves. You need to visit a doctor as soon as possible. If changes on the penis turn out to be a malignant tumor, it is important to begin treatment as soon as possible.
For foreign citizens we offer a preliminary free consultation
Leading specialists of the Center will answer your questions.
To get a consultation
Find out the price
The penis (penis) is the external organ of the male genitourinary system, intended for the excretion of urine, intercourse and ejaculation.
The penis consists of two cavernous bodies surrounded by a dense membrane of connective tissue, and a spongy body from which the glans penis is formed, located around the urethra (urethra).
The fold of skin that covers the head of the penis is called the foreskin. It has an inner and outer surface. The space that encloses the foreskin is called the preputial sac.
Diagnostics
The most accurate method for diagnosing penile cancer is a biopsy. The doctor removes the entire pathological tissue ( excisional biopsy ) or a fragment of it ( incisional biopsy ) and sends it to the laboratory for examination under a microscope. If cancer cells are found in the sample, the diagnosis leaves little doubt.
If enlarged lymph nodes are found, a biopsy may also be performed. The material for research is obtained using a needle or by surgically removing lymph nodes.
After penile cancer is diagnosed, the doctor may prescribe an ultrasound, computed tomography, MRI - these studies help assess how much the tumor has invaded neighboring tissues and spread to the lymph nodes.
Classification, stages of penile cancer
In 95% of cases, the tumor is squamous cell carcinoma of the penis , or squamous cell carcinoma . It usually grows slowly and is often diagnosed in its early stages and treated successfully. A malignant neoplasm can be located on any part of the penis; the most common is squamous cell carcinoma of the head of the penis and foreskin.
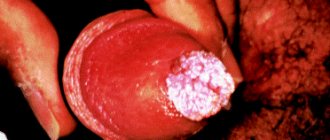
Much less common are warty carcinomas , or Buschke-Lowenstein tumors . Outwardly, they resemble large warts. This cancer also grows slowly, can reach large sizes, grow deeply into neighboring tissues, but rarely spreads to other parts of the body.
Melanomas occur on the skin of the penis, as in other places . This localization is not very typical, since melanoma most often appears on areas of the skin exposed to sunlight. This is an aggressive tumor, it metastasizes early and often has a poor prognosis.
Another slow-growing and very rare type of penile skin cancer is basal cell carcinoma , or basal cell carcinoma . Adenocarcinomas, malignant tumors from sweat gland cells, are extremely rare on the skin of the penis.
Depending on the size of the main tumor (T), the spread of cells to nearby lymph nodes (N) and the presence of distant metastases (M), the following stages of penile cancer are distinguished:
- Stage 0 : a tumor that is located in the superficial layers of the skin and does not spread deeper. This is the so-called “cancer in situ”.
- Stage I : the tumor has grown into the skin somewhat more strongly, but has not yet invaded adjacent tissues.
- Stage II : a tumor that has grown into the blood vessels, lymphatic vessels, spongy body, cavernous body, or into the urethra, or cancer cells have a low degree of differentiation and have completely lost their resemblance to normal ones.
- Stage III : The tumor has not grown beyond the penis, and the tumor cells have spread to one (substage IIIA) or more (substage IIIB) lymph nodes in the groin.
- Stage IV: the tumor has grown into the scrotum, prostate, pubic bones, or cancer cells have spread to the inguinal lymph nodes and have grown from them into surrounding tissues, or there are distant metastases.
Write to an oncologist
Surgery for penile cancer
Surgical removal of the tumor is the main treatment for penile cancer and can be used at almost any stage. If the cancer is within the foreskin, circumcision is performed. If the tumor is small and has not had time to grow deeply, it is removed with a small amount of surrounding healthy tissue. Such interventions are organ-preserving, after which all functions of the penis are preserved.
For large, deeply growing tumors, it is necessary to remove part of the penis or the entire organ. The consequences of such operations for penile cancer: disruption of the appearance of the genital organs and the ability to perform sexual intercourse, psychological discomfort.
When the entire penis is removed, the doctor creates a new hole in the perineum for the outflow of urine. After surgery, a man can still control the process of urination, but from now on he will have to urinate while sitting. Sometimes the scrotum and testicles have to be removed along with the penis, that is, castration must be performed.
Surgical intervention can be supplemented by removal of lymph nodes in the groin area. Previously, such operations were performed more often and on a larger scale, since the surgeon could not know for sure how many nodes were affected by cancer cells. Many men experienced a complication - lymphedema , swelling of the leg due to impaired lymph outflow.
Currently, there is a study that can be performed directly during surgery - sentinel biopsy , or sentinel lymph node biopsy . The surgeon injects a special dye into the tumor and looks at which lymph node it goes to first. This lymph node is called the sentinel lymph node. It is removed and examined for the presence of cancer cells. Depending on the result, a decision is made about the need to remove other lymph nodes.
Thanks to sentinel biopsy, surgeons remove inguinal lymph nodes only in cases where it is actually necessary.
4.Treatment
Traditionally, and for a long time, the only method of removing polyps was to cut off their stems with a special loop. However, medical technologies are developing rapidly, and today the methodology has stepped far forward. If the polyp is located externally, an electrocoagulator or liquid nitrogen (cryodestructor) can be used; deeper growths are removed using modern minimally invasive endoscopic instruments. Currently, various models and designs of radioknives, medical lasers, etc. are widely used in urological practice.
It is important to emphasize that therapeutic success directly depends on the timeliness of seeking help, and the likelihood of relapse is determined by how adequately and effectively all existing foci of infections were treated. To suppress the activity of the papillomavirus, one should, in particular, follow all immunostimulating instructions, and to avoid re-infection and scarring urogenital inflammation, strictly adhere to the principles of personal hygiene and safe sex.
The possibilities of conservative treatment of urethral polyps are currently not seriously discussed.
Chemotherapy
Chemotherapy for penile cancer is used before surgery to reduce the size of the tumor, after surgery to prevent relapse, and in case of metastatic cancer. The drugs used are: capecitabine, mitomycin C, ifosfamide, paclitaxel, 5-fluorouracil, cisplatin. Usually a combination of 2-3 drugs is used. Treatment is carried out in cycles: after each administration of the drug there is a break of several days. Cycles can last 3–4 weeks, the general course of treatment includes several cycles.
Find out the exact cost of treatment
Relapse problem
Performing organ-sparing operations provides a higher quality of life, but is associated with a higher risk of local relapse compared to amputation of the penis. In this regard, regular monitoring of the patient (physical and instrumental examination) is necessary in the postoperative period. As a rule, relapses are superficial, and their timely detection allows for minimally invasive intervention and preservation of the organ, which will provide a good chance of long-term remission.
Signs of Penis Cancer
The earliest symptom of penile cancer is a change in the condition of the skin on the head or shaft of the penis, which at first may appear as a small, inconspicuous lump. The area of changed skin may be flat or raised above its surface, have unchanged color or be pigmented. Gradually, as the lesion increases, the compaction loses its mobility, blisters and ulcerations may appear. Seals and ulcers can be painless or cause some discomfort (itching, burning, pain).
You should immediately consult a doctor at this stage. Attempts at self-treatment using traditional methods or on the advice of friends can lead to irreparable consequences.
As the neoplasm grows and develops, it infiltrates the underlying tissues and penetrates the corpus cavernosum and/or spongiosum. The primary tumor may bleed and have serous discharge. Infection of the disintegrating lesion leads to the appearance of an unpleasant odor, and there is a risk of developing urethral fistulas, soft tissue phlegmon, and sepsis. In advanced cases, self-amputation of the penis is not excluded.
Subsequently, regional lymph nodes are involved in the process, which enlarge, fuse together, forming conglomerates. The development of infectious lymphadenitis and purulent fistulas cannot be ruled out. As a result of impaired lymphatic drainage, elephantiasis may develop - severe swelling of one or both legs.
Further growth of the tumor and the appearance of metastases cause disruption of the general condition. Patients note weakness, fatigue, loss of appetite, and weight loss. Metastases in distant organs cause symptoms consistent with damage to these organs.
Prevention of penile cancer
The likelihood of developing the disease sharply decreases after circumcision (in medical parlance - circumcision) - an operation during which the foreskin is removed. There is virtually no incidence of squamous cell carcinoma of the penis in circumcised men. Other preventive measures:
- Careful personal hygiene.
- To give up smoking.
- Avoiding promiscuity and using condoms: This reduces the risk of contracting HIV and HPV.
| More information about treatment at Euroonco: | |
| Urologists-oncologists | from 5,100 rub. |
| Chemotherapy appointment | RUB 6,900 |
| Radiologist consultation | RUB 11,500 |
| Palliative care in Moscow | from 44,300 rubles per day |
Book a consultation 24 hours a day
+7+7+78