- Mechanical damage to the penis can occur during prolonged acts of masturbation or the use of certain sex shop items.
- sexual contact lasting more than two hours.
- with insufficient amount of natural lubricant released from the partner’s vagina (unless, of course, artificial lubricant is used).
- With rashes on the head of the penis and active sexual life, abrasions may also appear.
- long-term use of barrier protection (condoms) without the use of special lubricants.
- a chafed penis can be caused by wearing synthetic underwear and insufficient hygiene. Or vice versa, excessive abuse of antiseptic hygiene products or means for emergency prevention of sexually transmitted diseases.
- Balanoposthitis is a combined disease of balanitis - inflammation of the glans penis and posthitis - inflammation of the foreskin.
Rubbed my dick: why?
A chafed penis can bring more than just a lot of inconvenience to a man.
In addition, sexual life suffers due to severe pain in the affected area.
Possible infection.
Let's look at the reasons for chafing of the penis.
A man's penis is the most sensitive organ.
Due to the fact that the genital organ is covered with thin and delicate skin, which can rub even with slight mechanical impact.
The following are the causes of chafing of the penis:
- Insufficient amount of natural lubrication that is released during sex.
- Prolonged masturbation.
- Prolonged sexual intercourse (lasting more than 1 hour).
- Constant use of condoms without lubricant.
- Tight and poor quality underwear.
- Poor intimate hygiene.
- Use of antiseptics for a long time.
- Presence of inflammatory diseases.
- Rough rubber band of a condom.
Let's celebrate! As a rule, if the penis is rubbed, in addition to redness, swelling and burning are observed, which are painful during sexual intercourse and urination.
In addition, the skin on the penis becomes hot.
Sometimes small blisters or pustules may appear.
Rubbed penis: infection
If, for any of the reasons listed earlier, a man has rubbed his penis, he should visit a specialist.
If you neglect to go to the doctor, infectious agents may become infected.
This will lead to a more complex process and the development of serious diseases.
Remember! Peeling, chafing, pain, all these are not just symptoms that cause discomfort, but an impetus for the appearance of pathological processes on the penis.
The rubbed head of the penis is a good place for the proliferation of pathogenic flora.
This leads to infectious and purulent-inflammatory processes.
When infection occurs, the following diseases may develop:
- Candidiasis.
- HPV.
- Trichomoniasis.
- Syphilis.
- Gonorrhea.
- Mycoplasmosis.
- Ureaplasmosis.
- Balanoposthitis.
Therefore, do not delay your visit to the doctor.
When damage occurs
The penis is an organ covered with very thin and delicate skin.
Its surface is very sensitive to mechanical stress and is easily damaged. This is usually caused by insufficient lubrication during sexual intercourse, as well as by exerting too much effort to obtain pleasure. Chafing can be caused by an unsuccessful position for intercourse, as well as by creating an inappropriate angle for the penis to enter the vagina. Due to the anatomical features of the epithelium of the genital organ, the skin of the foreskin and head of the penis is most often rubbed. Situations predisposing to this are the following:
- Vaginal dryness and lack of lubrication.
- Prolonged and intense sexual intercourse.
- Discrepancy between the size of the partners' genitals.
- Using condoms that are larger or smaller than needed.
- Putting too much effort into masturbation.
- Prolonged masturbation.
- Unsuitable or poor quality underwear.
- Poor care and hygiene.
A man may constantly rub his foreskin due to developing phimosis (excessive narrowing of the foreskin, making it difficult to expose the glans). Interestingly, it is impossible to rub the scrotum during standard types of sex. Damage to this organ occurs due to wearing poor-quality underwear.
Rubbing on the penis at its base rarely appears. Most often this happens if a condom with a thick rubber band has been rubbed or the partner has dense and hard hair on the genitals. Damage to the penis, or more precisely on its shaft, can occur in the following cases:
- Due to the small size of the male genital organ, an unnatural angle of entry is used during sex.
- Copulatory dysfunction, as a result of which the skin does not adhere tightly to the tissues of the cavernous body, but moves freely.
- Spasm of the vaginal muscles in the partner.
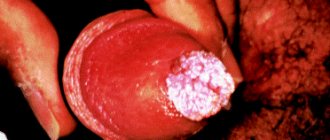
The fact that the skin of the genital organ has been rubbed may be indicated by a red spot, in which small red folds are visible when stretched. Sometimes abrasion appears as a scaly irritation or a small ulcer that tends to become inflamed and exudate. Sometimes increased friction leads to the formation of single blisters of different sizes. Examples of damage and what a rubbed penis looks like can be seen in the photo.
Chafing may appear as a blister
Genital hygiene
Following the rules of genital care will help avoid health problems. Follow these recommendations and the risk of infection will be minimal:
- regular shower - in the morning, in the evening, after playing sports, visiting the pool and sauna;
- Treat the head correctly - simply rinsing it with water is not enough. Use special products to remove smegma from the foreskin - this is where all infections, fungi and microbes accumulate;
- touch the genitals only with clean hands;
- change underwear, bedding and towels regularly;
- take a shower before and after sex;
- Do not have unprotected sex with casual partners.
Treatment
Treatment of any callus should begin with eliminating the etiological factor. To do this, you need to find out what exactly caused its appearance. At the first stage it helps:
- change of underwear and trouser style;
- using lubricants during sex;
- elimination of mental disorder accompanied by perverted masturbation.
If the callus on the foreskin or head of the penis is soft, then in many cases eliminating the cause will allow it to go away on its own. In case of extensive damage, you can apply a soft bandage with an antiseptic. It is recommended to treat a burst bubble several times a day with a disinfecting aqueous solution. Chlorhexidine or Furacilin are best suited.
Treating a hard callus is a longer process. The seal is lubricated with a fat-based cream until it disappears completely (you can use baby cream). Compresses made from infusions of anti-inflammatory herbs and lubricating the area of hyperkeratosis on the foreskin with fresh aloe juice help a lot.
If the cause of the blistering rash is pathogenic microflora, the doctor will prescribe antibiotics, antiviral or antifungal drugs. In this case, both sexual partners should undergo treatment.
Allergies are eliminated by taking antihistamines orally.
Possible complications
If a man, due to one or another of the reasons listed above, has rubbed the skin around the head of the genital organ, then one should not neglect going to the doctor and performing medical procedures. The appearance of peeling, abrasion, and pain can not only cause temporary discomfort, but also provoke the emergence of more serious pathological processes. The presence of microcracks on the skin, wound surface, any ulcerations and rashes in the area of the head and foreskin of the phallus is an open gate for the introduction of infectious agents and pathogenic microorganisms. The microflora of the head of the penis is an excellent natural environment for the reproduction and development of various types of pathogenic flora, which can lead to the development of systemic infectious diseases or purulent-inflammatory local processes with a tendency to systemic infection of the body.
Causes
Sudden appearance of blisters on the foreskin of the penis or a callus on the glans is not as rare as it may seem to many men. According to statistics, every second representative of the stronger sex faces this problem at least once in their life. What are the main reasons for the appearance of calluses on intimate organs and how can this formation be cured?
Every person faces problems with the formation of blisters filled with callus fluid, which over time turn into rough skin layers. This occurs due to wearing shoes that are too narrow or tight.
Calluses appear on the penis for completely different reasons, there are several of them:
- Inflammatory processes of the head of the genital organ (balanoposthitis). The first and most obvious symptom of the pathology is a callus. The onset of the disease is accompanied by pain, burning and rapid redness in the affected area of the mucous membrane of the head. Only a urologist can diagnose the disease and determine the treatment procedure.
- Mechanical influences. Calluses on the penis appear as a result of frequent sex without lubrication, which is more typical for teenagers without proper sexual experience. Watery formations also occur during long and inept masturbation.
- Venereal diseases. This is a rather unpleasant cause of blisters in the area of the foreskin and glans. Visually, calluses resemble herpes, and the pathology is accompanied by general malaise, weakness, and fever. A visit to a specialist in this case is simply necessary, since self-medication will only suppress the disease for a while, and a relapse will give a new, strongest surge in virus activity.
- Allergy. Calluses on the penis may appear if you are prone to allergic reactions and have changed the lubricant during sex or the laundry detergent. The use of cheap, low-quality condoms can also lead to pathology.
All these factors influencing the appearance of calluses on the penis indicate that at the first signs of formation, you will definitely need to consult a specialist with a full examination
In order to communicate with a urologist or dermatologist in detail, it is important to know the main symptoms of serious pathologies that do not require delay
Frequently asked questions about inflammation of the head of the penis
How can balanitis be dangerous?
Balanitis is dangerous, first of all, because of its complications. Complications such as gangrene and the spread of the inflammatory process to the genitourinary system pose a particular threat.
How long does it take to treat inflammation of the head?
How long to treat inflammation of the head of the penis depends on the stage of the disease, clinical manifestations and how to treat balanitis. Pathology in a simple form with proper treatment goes away in about 7 days. Treatment of balanitis is carried out on an outpatient basis, in rare cases - inpatient.
What effective remedies are there?
Ointment for inflammation of the glans penis in men is one of the most effective dosage forms, as it acts directly on the affected area. Depending on the etiology of balanitis, the ointment can be antifungal (Clotrimazole), antiseptic (Levomekol), or glucocorticoid. Antiseptic baths also have a beneficial effect. For severe forms of the disease, antibiotics are used.
Explanation of blisters
Small blisters on the scrotum or penis often indicate the presence of an infectious disease. Naturally, in this case, tests are required and a professional course of treatment is prescribed. Practice shows that the appearance of blisters of infectious etiology is accompanied by other symptoms:
- General weakness.
- Itching of the genitals.
- The appearance of red spots on the head of the penis or its base.
- Painful urination.
- The growth of the rash and the spread of blisters.
Infectious diseases that cause blisters: gonorrhea, chlamydia, syphilis.
Blisters on the penis can occur due to genital herpes. In this case, general signs of malaise are accompanied by the appearance of painless small blisters. When they burst, they form ulcers that are very painful. The rash may spread to the groin and legs. Herpetic blisters also appear on the scrotum.
There are reasons that have nothing to do with viral or bacterial diseases:
- Allergies (using a new contraceptive or intimate care product, wearing synthetic underwear).
- Trauma to the penis (pinching of the head during sexual intercourse, playing sports, impact).
- Balanoposthitis (inflammation localized in the area of the glans penis and foreskin).
- Chafing (during masturbation or overly active sex).
After analyzing the image of everyday and sexual life, a man can himself guess the reason for the appearance of bubbles on the penis and begin self-medication. Considering that the problem may be a symptom of a serious illness, seeing a doctor is still preferable.
Blisters on the penis can have different appearances
Swelling of the labia.
In women, swelling is often combined with itching and burning, discomfort, redness of the mucous membranes, the appearance of erosions, pathological watery discharge mixed with pus or blood, and inflammation of the inguinal lymph nodes. Pain may occur when walking, playing sports, or having sexual intercourse.
Swelling often occurs as a result of abrasions or wearing synthetic underwear, due to insufficient hygiene, allergies and sexual intercourse. But there are also more serious problems.
Why do the labia swell? Causes of swelling of the genital organs.
Various factors can cause swelling of the labia:
Candidiasis (thrush).
A characteristic symptom of the disease is white curd-like discharge, a sour smell, possible itching and burning, swelling, pain during urination and sexual intercourse. Yeast infections most often occur when the immune system is weakened and during pregnancy.
Bacterial vaginosis.
The result of an imbalance in the vagina. Green or gray discharge often appears, a fishy odor is felt, and swelling is possible. But asymptomatic progression of the disease also occurs.
Genital infections. Quite often, the labia become swollen due to irritation from pathological vaginal discharge caused by sexually transmitted diseases (trichomoniasis, ureaplasmosis, chlamydia, mycoplasmosis, gonorrhea). Other signs may appear: itching, irritation, unpleasant odor, painful urination.
Vulvodynia.
Accompanied by pain of varying intensity in the vulva area. It occurs suddenly, worries for a long time and often goes away just as abruptly. May sometimes cause swelling.
Vulvitis.
The main symptoms are swelling of the genitals, redness of the skin and burning. Inflammation of the vulva can occur due to poor hygiene and frequent changes of sexual partners, as a result of allergies, long-term use of medications and certain diseases.
Vulvovaginitis.
The main symptoms are skin flushing, abnormal discharge, pain when urinating, severe itching, causing the desire to scratch, which can lead to swelling. Often, inflammation of the labia develops due to poor hygiene and active masturbation, as a result of allergies or infections.
Bartholinitis.
Bartholin's glands are located in the vestibule of the vagina. When infected, they become inflamed, which is accompanied by redness and swelling of the genitals. If the gland duct is blocked, pus accumulates inside, which contributes to the formation of a cyst. In this case, discomfort and pain occur, which intensifies with movement.
Allergic reactions.
An allergy to fragrances contained in soap or intimate hygiene gel, components of washing powder, spermicides, latex condoms, tampons, low-quality pads, linen fabric, certain foods or medications can cause irritation. In addition to swelling, rashes are often found.
Contact and atopic dermatitis.
It develops with hypothermia, severe depilation of the bikini area, wearing tight synthetic underwear, and exposure to allergens. In the acute form, edema appears unexpectedly and grows rapidly, while in the chronic form it can periodically disappear and then reappear.
Sexual contact.
As a result of rough friction during sexual intercourse due to lack of lubrication (natural or artificial), damage to the labia and vagina is possible, which is accompanied by discomfort and swelling. In some cases, wounds and hematomas may form.
Stressful state.
Sometimes severe stress can cause itching of varying intensity and swelling in the genital area, which makes a woman distracted from the problems that have arisen.
Phthiriasis. (Pubic lice, lice)
You can become infected with lice not only through sexual intercourse, but also through everyday contact. The problem can be diagnosed quite easily by identifying bite marks or parasites. Lice cause severe itching, causing scratching, which causes swelling of the labia and pubis.
In addition to lice, swelling can be caused by mosquito bites, wasps, and bed bugs. In this case, bite marks are clearly visible, and the skin color may be red or bluish.
Hormonal disorders.
During the premenopausal period, the synthesis of estrogen decreases, which is why the woman feels dryness and burning, and possibly swelling of the genitals.
During pregnancy and the premenstrual period, blood flow to the tissues increases, which can lead to increased sensitivity of the mucous membrane. As a result, even the usual gel causes itching, burning and swelling.
Genital herpes.
The virus may not manifest itself in any way until favorable conditions arise (hypothermia, colds, vitamin deficiency, weakened immunity). The main signs are watery blisters, erosions, itching, swelling, twitching.
Tumor.
Quite often, in the initial stages, malignant neoplasms do not cause any symptoms. Occasionally, mild itching and slight swelling may occur, to which women do not attach much importance.
Additional factors.
With dermatological diseases, various parts of the body itch. The genitals are no exception. The woman begins to itch, causing swelling.
Diabetes mellitus causes increased dryness of the labia, which causes cracks and swelling. The wounds are irritated by urine, increasing the itching.
In rare cases, edema can occur due to diseases of the internal organs (heart, kidneys, liver, intestinal dysbiosis).
Treatment methods.
If swelling does not decrease within 24 hours and other symptoms become noticeable, you should visit a gynecologist. He will conduct a diagnosis, determine the cause of the pathology and select an effective treatment method. If necessary, he can refer you for consultation to other specialists (endocrinologist, cardiologist, gastroenterologist, nephrologist, allergist, venereologist).
Most often, local antiseptic treatment is carried out, and antibacterial or antifungal medications are prescribed. For candidiasis, suppositories containing antifungal substances, immunostimulating drugs, and a special diet are used.
For allergies, antihistamines will be helpful. For vulvitis, analgesics are used, and sometimes antihistamines and antidepressants may be needed. Herpes is treated with antiherpetic and immunomodulatory medications.
Timely consultation with a doctor helps to quickly get rid of problems. Self-medication can aggravate the situation, leading to the development of serious diseases and infertility.
And a little about the author’s secrets
Have you ever experienced unbearable joint pain? And you know firsthand what it is:
- inability to move easily and comfortably;
- discomfort when going up and down stairs;
- unpleasant crunching, clicking not of your own accord;
- pain during or after exercise;
- inflammation in the joints and swelling;
- causeless and sometimes unbearable aching pain in the joints...
Now answer the question: are you satisfied with this? Can such pain be tolerated? How much money have you already wasted on ineffective treatment? That's right - it's time to end this! Do you agree? That is why we decided to publish an exclusive interview with Oleg Gazmanov, in which he revealed the secrets of getting rid of joint pain, arthritis and arthrosis.
Attention, TODAY only!
The problem of a callus on the penis becomes an uncomfortable situation for many men, in the sense that the genitals are an intimate part of the body, and contacting a specialist causes unjustified embarrassment. However, except for a urologist who examined the formation that appeared and examined it, no one can make a correct diagnosis and explain the reason why calluses appeared on the penis.
Sudden appearance of blisters on the foreskin of the penis or a callus on the glans is not as rare as it may seem to many men. According to statistics, every second representative of the stronger sex faces this problem at least once in their life. What are the main reasons for the appearance of calluses on intimate organs and how can this formation be cured?
Every person faces problems with the formation of blisters filled with callus fluid, which over time turn into rough skin layers. This occurs due to wearing shoes that are too narrow or tight.
Calluses appear on the penis for completely different reasons, there are several of them:
- Inflammatory processes of the head of the genital organ (balanoposthitis). The first and most obvious symptom of the pathology is a callus. The onset of the disease is accompanied by pain, burning and rapid redness in the affected area of the mucous membrane of the head. Only a urologist can diagnose the disease and determine the treatment procedure.
- Mechanical influences. Calluses on the penis appear as a result of frequent sex without lubrication, which is more typical for teenagers without proper sexual experience. Watery formations also occur during long and inept masturbation.
- Venereal diseases. This is a rather unpleasant cause of blisters in the area of the foreskin and glans. Visually, calluses resemble herpes, and the pathology is accompanied by general malaise, weakness, and fever. A visit to a specialist in this case is simply necessary, since self-medication will only suppress the disease for a while, and a relapse will give a new, strongest surge in virus activity.
- Allergy. Calluses on the penis may appear if you are prone to allergic reactions and have changed the lubricant during sex or the laundry detergent. The use of cheap, low-quality condoms can also lead to pathology.
All these factors influencing the appearance of calluses on the penis indicate that at the first signs of formation, you will definitely need to consult a specialist with a full examination. In order to communicate with a urologist or dermatologist in detail, it is important to know the main symptoms of serious pathologies that do not require delay
Types of calluses on the penis
There are two stages in the development of a callus on the penis:
- soft (wet) - first stage;
- hard (dry) - second stage.
After injury or mechanical damage, a wet callus appears, which manifests itself within 24 hours. Soft tissues swell, the skin becomes inflamed, and turns red. At the same time, small bubbles with liquid inside grow. The patient experiences acute pain, irritation, burning, and it is impossible to touch the penis. This is the most noticeable stage in the development of infection. At this moment you need to consult a doctor; ignoring the disease provokes the transition of the callus to the second, dry stage.
With continued friction or any other mechanical impact on the callus, the growth gradually wears off, the tissue becomes covered with the cornea, and becomes coarser. This is a hard type of growth. The man already feels less pain, which can lead to refusal of treatment. The head of the penis becomes less sensitive, and it becomes more difficult to get rid of this condition. Also, in the chronic version, wounds may appear, in which the pain returns again.
What are calluses?
Everyone has probably encountered the appearance of calluses on their hands or feet - this is a fairly common phenomenon that bothers a person, but rarely leads to complications and is easy to treat.
Calluses are rough areas of skin, or blisters filled with fluid, caused by skin irritation. Most often, this disease appears on the feet as a result of wearing uncomfortable, new or smaller shoes. In addition, the disease can occur on other parts of the body, in particular on the genitals.
Calluses on the penis are the appearance of rashes with liquid inside on the male genital organ. In order to understand how serious this is, you need to know the causes of such rashes.
Features of treatment depending on the manifestation
| Location | Description, treatment |
| Head | If blisters have formed in this part of the penis, then self-medication will not help. Mostly, diseases of herpes, syphilis or HPV manifest themselves in this way, which can only be cured under the supervision of a doctor. If suspicions arose due to the discovery of small pale pink formations on the butt, then this condition is considered normal for men. |
| Pubis | The main cause of blisters on the pubic area in men is poor shaving technique. Formations can be cured by treating the adjacent surface with iodine or brilliant green. If the cause is a fungus, then treatment is carried out with special drugs or traditional medicine. |
| Foreskin | If blisters are found on the foreskin, then the underlying cause is an allergic reaction. Treatment consists of using antihistamines and eliminating the irritant. It could also be a disease called balanopositis, which is characterized by the formation of white blisters. To get rid of white blisters on the penis, it is necessary to take measures to strengthen the immune system, in addition to treating with drugs with antiseptic properties. |
| Blisters on the scrotum and testicles | A disease that causes a blister to form on a man's testicle in this area is usually a fungus or an STD. Treatment should only be carried out under the supervision of a specialist. |
What is lichen sclerosus (LS)?
LS is a chronic inflammatory skin disease, usually of the genital organs in men and women, the causes of which are still far from fully understood and known. However, it is now clear that if LS is not treated, this disease leads to scarring of the genital organs, which can cause serious problems. Men, in particular, may develop a narrowing of the foreskin (phimosis) and difficulty opening the glans penis. In more severe cases, a narrowing (stricture) of the external opening of the urethra and the scaphoid fossa (the part of the urethra closest to the external opening) may form, which leads to urination disorders and impaired urine outflow. Such changes can cause a decrease in quality of life, and sometimes lead to complications such as urinary tract infection (pyelonephritis, cystitis), dilation of the renal cavity system (hydronephrosis), and urolithiasis. In addition, severe forms of LS are considered predisposing conditions for the development of penile cancer.
What synonyms for disease can your doctor use when referring to LS?
Several synonyms can be used to describe SL. As a rule, the names of the diagnosis of LS may vary depending on the specialty of the doctor and the location of the skin lesion. For example, gynecologists often use the term “vulvar kraurosis”, dermatologists - “lichen sclerosus”, urologists - “xerotic balanitis obliterans”. In 1976, the International Society for the Study of Vulvar and Vaginal Diseases (ISSVD) recommended using the term lichen sclerosus to describe this disease. The American Academy of Dermatology (AAD) joined this recommendation of gynecologists in 1995.
To date, unfortunately, none of the professional urological associations have come to unity in the use of the term “lichen sclerosus” (Latin: lichen sclerosus). In Russia, in most educational institutions, LS is not taught at all to urology students as an independent form of inflammation of the glans and foreskin of the penis. In this regard, many urologists simply do not know either the symptoms of this disease or its treatment methods. Very often we have to deal with situations where patients with LS were treated with antibiotics in the form of systemic and local therapy for “banal balanoposthitis”, “fungal balanoposthitis”, “herpes”, “chlamydia”, “acquired phimosis”, etc. However, since antibiotics and antifungals are often not effective for LS, and surgical removal of phimosis (circumcision or circumcision of the foreskin) was not accompanied by further treatment, patients never received adequate care.
Prevention
Prevention methods include getting rid of all the causes that can lead to the formation of calluses on the penis.
First of all
It’s worth
reviewing your wardrobe
and removing from it all items of clothing that can restrict movement and create significant pressure in the perineal area. As for underwear itself, preference should be given to natural fabrics, since they do not interfere with thermoregulation (which will not lead to heavy sweating), allow air to pass through well and do not cause allergic reactions.
Regarding the sexual sphere of life
, here it is worth paying more attention to all aspects. Maintaining hygiene is basic. Shower before and after sex. It would be best to use not ordinary soap, but soap that contains an antiseptic.
During sex, pay attention to the presence of lubrication. If during foreplay a sufficient amount of it is not released, you should turn to the use of lubricants.
You also need to pay attention to the composition of the lubricant. Test it on a small area of skin first by applying a few drops and waiting a couple of minutes. If there are no unpleasant sensations (in the form of itching or tingling), you can safely use it.
If you use, then you should pay attention to the wall thickness and size. There is no need to choose smaller condoms if you are afraid that it will slip off during intercourse
With sufficient excitement, such trouble will not happen. And, as for wall thickness, the smaller it is, the better.
There are also different types of condoms
with pimples, antennae, etc. If you have very sensitive skin on the penis, such that there is a risk of calluses, then it is better to avoid using such rubber products, because despite the fact that these seals are located on the outside of the condom, under pressure they will also affect the penis.
Another interesting point is the fact that before the onset of menstruation, girls experience some roughening of the surface of the vagina. During this period, less lubricant is released, so during sex at such moments you need to be even more careful and don’t give yourself a sex marathon, because it will definitely end with the appearance of calluses on the head of the genital organ.
Finally
I would like to say that in any case you should carefully listen to the sensations of your body. Calluses on the penis, although not the worst injury to the genital organs, may well lead to more serious consequences in the future.
Attention, TODAY only!
Prevention of calluses on the genitals
It is advisable for all men to prevent the appearance of calluses. It is as follows:
- during the treatment period and for some time after it, it is necessary to abstain from sexual intercourse,
- do not have dry sex,
- choose the right clothes,
- Do not use condoms with fluff, pimples and other additional traumatic parts.
It is also important to observe the rules of general and sexual hygiene. If you do everything according to the recommendations, you can avoid the reappearance of calluses.
Treatment methods
Treatment will be most effective if started early. As soon as swelling and blistering have been detected, the skin should be treated with an antiseptic.
ATTENTION: Under no circumstances should you use solutions containing alcohol!
A solution of chlorhexidine or furatsilin is best suited
.
Also, it is necessary to get rid of the original source of the problem, that is, abstain from sex for a while or stop wearing tight clothes that could lead to the formation of calluses.
If you live in an apartment completely alone, then you should not neglect air baths and stop wearing clothes at home for a while. But in this case, it is worth treating the damaged organ with an antiseptic more often so that dust and other contaminants from the environment do not affect the development of infection.
Regarding the treatment of hard calluses
, then the only acceptable outpatient method in this case would be the use of fatty moisturizing creams (for example, baby cream). But if you wish, you can resort to surgical removal of keratinized skin.
Treatment
If calluses on the penis or foreskin are the result of mechanical stress, the doctor will prescribe lotions using special solutions or ointments. As a rule, if you fully act according to the prescribed scheme and regularly treat the penis, the disease goes away within 10-14 days.
If a specialist determines that the cause of the appearance of a callus on the penis is an allergic reaction, recent contacts with objects that touched the organ should be analyzed and its cause should be identified. Most often, taking anti-allergy drugs and lotions quickly relieve the symptom without causing side effects.
If treatment is not started on time or is carried out incorrectly, an infection may occur due to an allergic reaction of the body to medications, and antibiotics will need to be added to the drug complex.
For inflammatory processes, the doctor prescribes medications, medicines and ointments on an individual basis, or prescribes surgical removal of the formation.
Factors influencing the formation of wounds on the foreskin
When wounds form, the patient experiences discomfort when urinating and acute pain in the area of the penis during intimate relations.
There are a number of reasons why this pathology may manifest itself:
- neglect of personal hygiene of the genital organs;
- allergic reactions to contact with an external pathogen;
- diabetes mellitus, which has a direct effect on the nutritional process of the entire skin;
- mechanical damage can occur even from tight underwear;
- urethritis.
The formation of wounds and large cracks in the foreskin can occur at any age, both in children and adults.
Symptoms and diseases of the foreskin:
- Swelling of the foreskin
- Foreskin rupture
- Inflammation of the foreskin
- Redness of the foreskin
- Foreskin removal
- Narrowing of the foreskin
- Ulcers on the foreskin
- Herpes on the foreskin
- Red spots on the foreskin
- Sores on the foreskin
- Dryness of the foreskin
Symptoms
Calluses on the penis manifest themselves as follows:
Diagnosis in complex cases is made using laboratory tests to identify a possible genital infection. An allergic reaction may cause itching and rashes not only on the penis, but also on other parts of the body.
You should definitely consult a doctor if the following symptoms develop:
- the appearance of a formation on the head or foreskin is accompanied by severe discomfort;
- rashes do not disappear after stopping contact with the possible allergen and new ones appear;
- in parallel with the appearance of the bubble, severe swelling and redness begins;
- lymph nodes in the groin enlarge;
- The skin at the site of the blister, after opening it, turns into an ulcer or wound surface and does not harden over time.
Such clinical signs indicate the presence of infection and its further spread.
.
What can be the prevention of genital LS?
Unfortunately, there are no effective preventive measures that could prevent LS disease. However, if you notice the first signs of LS, you should immediately consult a urologist (men) or gynecologist (women). After all, as mentioned above, if LS is not treated in a timely manner, quite serious consequences can occur. Early removal of the affected skin tissue of the genital organs, followed by observation and, if necessary, treatment with ointments can stop the disease and prevent it from causing such dangerous complications. Before consulting a doctor, it is important to make sure (by studying his reputation based on patient reviews) that he is quite knowledgeable in the diagnosis and treatment of LS and other diseases of the genital organs. Men should remember that treatment of advanced forms of LS sometimes requires complex reconstructive operations to restore patency of the urethra. In this regard, the urologist to whom you would entrust your treatment must be fluent in these operations.
The Andros Clinic provides treatment for all forms of lichen sclerosis of the genital organs. If necessary, all operations necessary to get rid of this disease can be performed, from circumcision to complex reconstructive operations on the urethra. If there are lesions suspicious for penile cancer, a biopsy and careful histological examination are performed.
Materials used in preparing the publication: Lazzieri M, Barbagli G, Palmintieri E, Turini D. Lichen sclerosus of the male genitalia. Contemporary Urology 2001; 3.
Actions for rubbing
If a man rubs the head of his penis or its shaft, then, as already mentioned above, the damage may swell, accompanied by swelling, redness and pain. These symptoms cannot be ignored. The recommended action for such symptoms is to visit a doctor. A visit to a specialist is necessary to exclude the possibility of an infectious nature of ulceration or balanoposthitis, since these conditions require systemic therapy with specialized drugs.
If a man is sure that he does not have complex pathologies, and also knows exactly the cause of the chafing, he can begin treatment on his own.
Genital hygiene
When a man has rubbed the head of the penis, it is recommended that he wash himself with regular laundry soap or intimate hygiene product. Such measures do not lead to increased dryness of the mucous membranes and ensure cleanliness of the genitals without additional irritation.
For chafing of the genitals in any place, antiseptic and anti-inflammatory sitz baths are recommended:
In a weak warm solution of potassium permanganate (the solution should have a very pale pink color, before taking it is important to make sure there are no undissolved crystals). Add chamomile infusion (pour three tablespoons of the raw material into half a liter of boiling water, leave for an hour, dilute in three liters of water for a bath). In the infusion of a series (brewed like chamomile).
After hygiene procedures, it is important not to wipe the genitals with a towel, but to blot them with a thick paper napkin
Use of antiseptics
After hygiene procedures, the use of local antiseptics in the form of solutions is possible and recommended. This will ensure disinfection of the genital organs and prevent complications of chafing in the form of suppuration or inflammation. You can use Chlorhexidine, Miramistin. The treatment is carried out by watering the genital organ from all sides. It is advisable not to remove the remaining product, but to leave it until it dries completely on its own.
Healing agents
A healing cream or ointment may be needed if the skin is severely damaged or if there are symptoms of inflammation. It is recommended to treat wounds with ointments containing not only a regenerating component, but also a local antiseptic or antibiotic, as well as an anesthetic to eliminate pain (Trimistin, Miramistin).
It is most effective to smear the damage immediately after rubbing the organ. The layer of medicine should be quite dense. A fresh wound can be lubricated with a product with only a healing effect:
- Bepanten.
- Solcoseryl.
- Methyluracil.
If you ignore the problem, a callus will form on the constantly rubbing area, reducing the sensitivity of the genital organ and leading to its deformation. After an examination, your doctor will tell you what to do with an existing callus.
Proper therapy can get rid of the problem in a few days.
Chafed penis: how to treat?
Before you start using any medications, you should definitely find out the reason for the appearance of chafing on the penis.
If the cause is insufficient lubrication, then treatment is based on treating the penis with antiseptics and soothing ointment.
The doctor will recommend medications with local effects.
Treatment of chafing of the penis is carried out by using:
- Bath with potassium permanganate.
- Chamomile decoction.
- Ointments with anti-inflammatory action.
The most effective are ointments containing dexpanthenol.
It accelerates the process of healing and regeneration of the skin.
Therefore, reparation will occur quite quickly.
To prevent the development of infection, you can use Miramistin and Chlorhexidine.
These medications should be applied several times a day to clean skin of the penis.
If there is a suspicion of the addition of pathogenic flora, laboratory tests should be done.
After receiving the result, treatment begins.
Depending on the flora, antibacterial or antifungal drugs are prescribed (Diflucan, Nystatin, Fluconazole).
In addition, products that stimulate the immune system and vitamin complexes are mandatory.
If necessary, hormonal levels are corrected.
Symptoms
You will need a doctor's help if you experience:
- The appearance of blisters and calluses on the surface of the penis is accompanied by severe itching and burning;
- The rash does not go away within 10-12 days, and in addition, new formations appear nearby in large quantities. (those calluses that arise as a result of mechanical stress usually disappear within 2 weeks, and already on the 5th day you can notice improvements);
- The glans penis and foreskin began to become inflamed and swollen;
- There was an increase in lymph nodes in the groin;
- The skin at the site of watery formations does not become rough, but turns into ulcers;
- In place of the burst calluses, non-healing wet wounds remain.
Be sure to pay attention to these signs and rush to see a specialist. Such symptoms, first of all, indicate the spread of infection in the body or the onset of a serious urological or venereal disease
Where does penile mycosis occur?
Genital mycoses usually develop in the female genital tract. In men, infection most often occurs through sexual contact. You can also become infected with the yeast Candida albicans from a towel, toilet, swimming pool or sauna. In the male body, mycosis of the penis rarely develops independently, although such situations also occur.
Factors contributing to this include:
- taking certain medications, especially antibiotics and steroids;
- neglect of hygiene of intimate places - too infrequent or careless washing;
- anatomical problems, especially phimosis, preventing free access to the glans penis;
- inaccurate drying of the penis after swimming, before getting dressed;
- use of wet towels;
- wearing thick, windproof clothing and underwear made of synthetic materials.
Remember that the ideal conditions for yeast development are a combination of heat and moisture. It is also easier for people with weakened immune systems (such as HIV-infected people) and diabetics to develop infections.