It is quite difficult for a person who has never encountered “skin” problems to determine whether the formation that appears on his skin is a condyloma or a papilloma. There are frequent cases of panic, attempts to get rid of the formation using folk methods and other things that are far from an ordinary consultation with a dermatovenerologist. In fact, distinguishing condyloma from papilloma is not so difficult; you just need to familiarize yourself with the main differences.
In this article we will talk about how papillomas differ from condylomas, learn about the characteristic signs and routes of transmission of these diseases, and also get acquainted with the principles of their diagnosis.
The type and symptoms of papillomas depend on the type of virus
About the development of the disease
According to WHO statistics, there are about 100 types of human papillomavirus, 80 of which have been studied in detail. This pathogen is considered to be the cause of the following diseases of the skin and mucous membranes:
- genital warts (papillomas) - type 6, 11, 42, 54;
- cervical dysplasia with a high risk of its degeneration into cancer (types 6, 11, 16, 18 and more than 16 varieties);
- malignant neoplasms of the external genitalia and perineum (about a dozen viruses, including type 54).
HPV is transmitted primarily through sexual contact. Men and women are susceptible to infection at the same rate. The virus is located on the skin of the genital organ, and the use of condoms does not always prevent infection. The risk of infection increases when changing sexual partners. There is an individual, genetically predisposed predisposition to developing the disease when infected with a virus. Increased hormonal levels, for example, during pregnancy or when taking hormonal contraceptive drugs, make the skin of the external genitalia, vaginal mucosa and cervix more susceptible to the effects of the virus. In most cases, the viruses that cause genital warts are not highly oncogenic.
{Anchor::title('Clinic')}
Make an appointment with a gynecologist
Laser removal of papillomas and condylomas in Vladivostok
With this method of removal, papillomas and condylomas are burned using a carbon dioxide laser beam. The procedure usually leaves a microscopic wound that heals within 3–4 weeks. Removal occurs precisely, without damaging adjacent areas of the skin. Rehabilitation as such is not provided - the skin recovers on its own, leaving no scars. You can use a laser to remove both single and multiple formations located on the face and body, including in delicate places (on the eyelids, armpits, perineum). Laser removal is not performed in the presence of wounds or local inflammation of the skin, herpes, general infections, or pregnancy.
Genital warts - clinical picture
Genital condylomas (papillomas) are papillary formations resembling cauliflower, the favorite localization of which is the skin and mucous membranes of the external genital organs and the perianal area. Less commonly, they are found around the external opening of the urethra, on the walls of the vagina or the cervix.
The appearance of genital warts is associated with rapid growth of tissues of the mucous membranes and skin under the influence of changes in cells caused by the human papillomavirus. In fact, condylomas are a type of benign tumor that grows and sometimes affects a large surface. These growths are pink-red or flesh-colored, they are painless, and only in some cases do patients notice the appearance of a feeling of itching or burning; even more rarely, condylomas can bleed. Sometimes condylomas disappear on their own without treatment.
{Anchor::title('Diagnostics')}
Warts and papillomas: what is the difference and how not to confuse them
Warts, as well as papillomas and genital warts, are the most common manifestations of the human papillomavirus. The general nature of these neoplasms determines their many common features. For example, both warts and papillomas can disappear and appear depending on the state of the human body and its immunity. However, there are also many differences... However, in order to talk about the differences and common features of warts and papillomas, you need to clearly understand what exactly we are talking about.
Warts: what you need to know
Warts are benign skin growths that can reach from 2 to 10 mm in diameter. Warts have an uneven surface and clear boundaries; they can have an irregular or rounded shape and color, from light gray to brown or even grayish-black.
The localization of warts is most often observed in places subject to mechanical trauma: these can be elbows, knees, fingers, scalp, however, warts often appear on other parts of the body.
Warts can be transmitted through household contact with an infected person.
Conventionally, the variety of varieties of warts can be divided into three groups:
- simple warts. About 70% of all warts fall into this group;
- plantar warts. Slightly less than 30% of the total number of warts. Adolescents and young adults are at risk;
- flat warts. The smallest category: occurs in 4% of cases.
Papillomas: what you need to know
Papillomas are represented by benign soft formations of a round shape. They typically have a wide base or stalk and are light brown or flesh-colored. As for the size of papillomas, it can vary within a fairly wide range: from 0.2 to 10 mm.
As is the case with any other viral skin lesions, over time the number of papillomas on the body increases, they affect an increasingly larger area of the skin. The main “habitat” is the armpits, groin area, face or neck.
People with weakened immune systems are at risk. Usually, papillomas appear after acute gastrointestinal diseases, after long-term use of medications, after stress, and so on.
As for the routes of infection, the highest risk of infection is observed in places with high humidity, and human skin is not protected by clothing: we can talk about swimming pools, baths, saunas, and so on.
Differences between warts and papillomas
1. Location. Warts often appear on the arms and legs, while papillomas often choose “secret places”: the genitals, the area under the breasts in women, the armpits.
2. Visually, it can be difficult to distinguish a wart from a papilloma. A distinctive feature of papillomas are legs or wide bases, that is, if we are talking about bulges hanging on legs, similar to warts, then most likely these are papillomas. In addition, the surface and edges of the papilloma are torn and rough, visually similar to a mini head of cauliflower. As for the wart, it has clear boundaries.
If you cannot distinguish a wart from a papilloma on your own, if you are not sure of your opinion, you should consult a specialist. But often even a professional is not able to visually determine what type of human papillomavirus we are talking about.
In order to accurately determine the diagnosis, the patient must undergo tests to determine the type of virus. The PCR method is usually used, the classic DNA diagnosis of human papillomavirus; more about it in the article “Human papillomavirus”.
In addition to the PCR method, other diagnostic methods for determining the human papillomavirus can also be used, including biopsy and colposcopic examination (if the tumor is localized in the vaginal area).
A biopsy is the removal of tissue from an affected organ for examination. Today, a biopsy is the most common and accurate research method: it must be carried out without fail if there is a suspicion of papilloma, since in this case it is necessary to exclude the risk of oncology.
Diagnosis of HPV implies the possibility of conducting histological and cytological studies. The main thing is a cytological examination, which allows one to determine under a microscope changes in cells under the influence of a viral infection.
To clarify the diagnosis, a histological examination is carried out, in which the subject of study is not a scraping of surface cells (as for a cytological examination), but a piece of the affected tissue.
As a conclusion, I would like to say: even if you think that you have made up your mind and know for sure whether a wart or papilloma has appeared on your body, it is better to seek advice from a specialist, since the human papillomavirus is represented not only by these two types of neoplasms, but also by dozens, hundreds of other species, many of which are oncogenic. Read more about various neoplasms on the body in the article “Growts on the skin: benign, malignant and borderline.” To eliminate the risk of developing a malignant tumor, it is enough to consult a doctor in time and undergo the necessary tests.
Removal of tumors at Lazmed Clinic
Diagnosis of genital warts (papillomas)
Genital warts are easy to identify by visual examination and it is rarely necessary to resort to laboratory diagnosis using biopsy and histological examination. It must be remembered that the cause of condylomas is the human papilloma virus, which can also affect the cervix. Despite the fact that the types of virus responsible for the formation of genital warts rarely have oncogenic potential, it is imperative to be vigilant and carry out oncological screening - cytological diagnosis of the cervix, determination of the type of virus by examining its DNA and colposcopy if indicated. You can read more about the cancer screening program at the Yauza Clinical Hospital here.
Removal of papillomas with liquid nitrogen (cryodestruction)
The method involves short-term exposure of the papilloma to very low temperatures. The tissue being removed is destroyed by flash freezing. The area of skin treated with nitrogen loses sensitivity and becomes white. Complete healing occurs after 5–6 weeks. The advantages of this method are that the procedure is easily tolerated by the patient, there is no need for anesthesia and there is no risk of scarring. However, with nitrogen removal it is difficult to determine the depth of impact on papilloma or condyloma.
Where to go to remove papillomas and condylomas in Vladivostok?
To carry out the procedure for removing an unwanted tumor, you should contact the Clinic on Komarova. But how to choose from the variety of public and private clinics the one that will provide the service of the required quality at an affordable price?
It is worth choosing a clinic where they can provide a range of services: both for diagnosis and treatment. Pay attention to the level of equipment of the clinic, the level of service and, of course, the pricing policy.
The clinic on Komarova is equipped with the latest equipment. For example, diagnosis of neoplasms is carried out using SEAscope. The clinic provides a wide range of medical services: from diagnostic to surgical treatment. At the same time, we maintain affordable prices and a humane attitude towards each patient.
Skin care after the procedure
Try not to wet the skin after removing the tumor, do not treat it with lotions, creams, or decorative cosmetics. Under no circumstances should you peel off the crust formed after the procedure! This can lead to infection of the wound, prolongation of healing time, and noticeable scarring. After the crust comes off, young skin needs to be protected from sunlight with a cream with a UV filter. This will help avoid the appearance of age spots. Do not touch this area with a washcloth until the crust completely falls off.
Cost of removing papillomas or condylomas
Before removing skin tumors, you must consult a dermatologist or dermato-oncologist, undergo the necessary tests and obtain a medical opinion. Only after this can you begin the removal procedure. It is advisable to do all this in one clinic. An initial examination by a dermatologist or dermatologist at the Clinic on Komarova costs about 1,000 rubles, and a dermato-oncologist costs 1,400 rubles.
Removal of benign skin tumors at the Clinic on Komarova is carried out using a CO2 laser.
Removal of moles, keratomas, warts: from 700 to 5,000 rubles.
Removal of papillomas from 1 to 5 pieces (for one): 250 rubles.
- From 6 to 20 pieces - 5% discount.
- From 21 to 30 pieces - 7% discount.
- From 31 to 50 pieces - 10% discount.
- From 51 or more pieces - 20% discount.
Traditional methods for removing papillomas and condylomas
There are also folk remedies for removing papillomas and condylomas. A well-known method is to treat them with celandine juice. To protect the skin around the papilloma from being burned by the poisonous juice of this plant, it is lubricated with baby cream, then a drop of medicinal liquid is applied to the very center of the skin tumor. Another remedy is an infusion of dandelions in alcohol; it dries and disinfects the skin. The flower heads are tightly filled into a small glass container and filled with ethyl alcohol. Leave for about two weeks, store the solution in a dark place. They lubricate the affected area up to five times a day. It is difficult to say how safe and effective all of these methods are, so it is better not to tempt fate and consult a doctor.
Electrocoagulation of papillomas and condylomas in Vladivostok
Another common method for removing tumors, in which the destruction of pathological tissue is achieved by exposing it to electric current using EHF devices. The destruction of papillomas and condylomas occurs under the influence of high temperature and, as a result, adjacent areas of the skin are also damaged. Electrocoagulation is usually inexpensive, but it can cause injury and poor healing. The advantage is that with this type of removal it is possible to control the depth of impact on the skin.
What are the goals of treatment for diseases caused by HPV, and how is it carried out?
Diagnosis, treatment and prevention of genital diseases caused by HPV in men is carried out by urologists, in women - by gynecologists. Unfortunately, there are currently no methods of systemic action on HPV in the human body (antiviral agents) that could be used to completely destroy the virus. The main goal of treatment for OCs is their removal using electro- or laser coagulation, excision, cryodestruction (destruction by cold), as well as using chemicals, cell toxins (podophyllin) or immunomodulators applied topically. Removing OK solves mainly a cosmetic problem; there is no data confirming that removing OK helps to completely remove HPV from the body or reduce the risk of its sexual transmission or infection of the fetus during childbirth. There is no evidence that OC treatment has any effect on the likelihood of developing cancer. However, from a common sense point of view, removal of OCs should reduce the risk of development and recurrence of diseases caused by HPV.
The main goal of treatment of squamous epithelial lesions of the cervix is the prevention of cervical cancer. If a cytological Pap smear shows the presence of a lesion of unknown significance at the risk of malignancy, dynamic observation with Pap smears performed every 4 to 6 months for 2 years is indicated until there are 3 consecutive negative (without any pathological changes) smears. Women with high-risk intraepithelial lesions require immediate colposcopy and possibly biopsy of the detected lesions for more detailed histological evaluation. If CIN 1 is identified as a result of histological examination, dynamic observation is indicated, because the vast majority of such lesions undergo spontaneous regression to normal. For lesions of CIN 2/3, active treatment is required, which consists of cryodestruction, laser evaporation or loop electrosurgical excision (conical excision or conization) of the cervix.
Recent randomized clinical trials have shown that all three methods have similar rates of complications (2 - 8%), persistence (3 - 5%) and recurrence (13 - 19%) of lesions. Risk factors for persistence (lack of treatment effect) were a large affected area, relapse - older age, the presence of oncogenic HPV types 16 and 18, as well as previous treatment.
Surgical removal of papillomas and condylomas in Vladivostok
Surgical excision is used in cases of removal of large tumors. Removal occurs in the operating room under local anesthesia. During surgical excision, a small portion of healthy tissue is also captured. After the operation, cosmetic sutures are applied, which are removed after approximately 7 days, depending on individual indications. When removing tumors on the face, this method is used only in cases of extreme necessity. The method is quite effective in removing malignant tumors.
Radio wave removal of papillomas and condylomas in Vladivostok
This newest method uses the Surgitron device. The main working part of the device is the electrode, which is a thin tungsten filament. Depending on the depth of exposure required, different electrodes are selected. High frequency radio waves - from 3.8 to 4 MHz - are concentrated at the end of the electrode. The neoplasm is destroyed by energy that heats the papilloma from the inside without damaging surrounding tissue. The electrode is heated by an electrical discharge, and the tumor is instantly “cut off” with one movement. Under the influence of ultra-high temperatures, nearby tissues are cauterized, and the vessels are “sealed,” which avoids blood loss and associated unpleasant consequences. There is no pain, adjacent tissues are not damaged. Healing occurs quickly, there are no traces of removal. This is the optimal way to remove not only papillomas and condylomas, but also any other skin formations.
Features of the development of warts
Warts are benign skin growths measuring 2-10 cm in diameter. The growths have a rough, uneven surface, a rounded shape and clearly defined edges. The color varies from light gray to darker brown or grayish-black. As a rule, they are localized on the elbows, knees, fingers and soles, and therefore are at increased risk of mechanical injury. In such cases, removal of warts to avoid complications in the form of malignant tissue degeneration.
According to the nature of the clinical picture, they are divided into 3 categories:
- Simple. About 70% of all neoplasms.
- Plantar. Diagnosed in 25-26% of patients. Typically appear in adolescence and young adulthood.
- Flat. Occurs only in 4% of cases.
Treatment of condylomas and papillomas - examination by a dermatovenerologist is mandatory
The above fully applies to human papillomavirus (HPV, sometimes written HPV, from “human papillomavirus”, or HPV).
Acellular, or precellular, or smaller-than-cellular viruses appeared simultaneously (or earlier, or later) with organic cellular life (or were brought to Earth from outside); they parasitize it to this day, for billions of years and in millions of varieties. Viruses are the smallest known (or even possible) life forms.
Or not life, but some strange existence inherent in fragments of ribonucleic acids - carriers of genetic information. Being an obligate parasite of a living cell, the virus outside organic matter is absolutely and perfectly dead, because in such a small, nanometer volume there is simply nothing to live.
However, in living tissue, the virus begins to rearrange other people's genetic codes in its own way; For the host organism, this activity is, at best, harmless, at worst, fatal.
The inherent ability of viruses to self-replicate is one of the fundamental criteria of life as such, but the same ability was discovered in 1982 in prion proteins, which, not being viruses (and unlike the latter), do not even contain nucleic acids...
The previous paragraph reflects, in an extremely brief and simplified form, the content of modern scientific ideas, discussions, hypotheses about the nature of viruses. The human papillomavirus makes its own remarkable contribution to this confusion. Warts, papillomas, and condylomas have been known since the birth of what we call medicine today.
Then ancient doctors, observant people with remarkable analytical intelligence, established that these skin formations can be transmitted sexually.
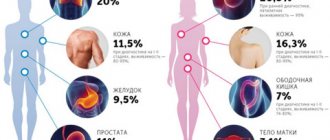
In recent decades, when the statistical, histological, microbiological and clinical relationships began to be finally clarified, the WHO declared a “red alert level” for cervical cancer and some other cancers, clearly and conclusively linking the horrific epidemiological situation with HPV. However, A.D.
Rigoni-Stern, in fact, proved the same thing back in the middle of the 19th century - when scientists already guessed about the existence of viruses, but were not sure - and over the next century, many specialists (including domestic ones, e.g. L.A. Zilber) have repeatedly confirmed this conclusion.
When reviewing the literature, one gets the impression that the virus is capable of confusing even such an accurate, dispassionate and rigorous science as mathematical statistics. WHO estimates the prevalence of HPV in the general population of earthlings at 60-70%.
However, other sources clarify: in an actively pathogenic form, this virus is detected with a frequency of approximately 1:2,000, in 30% of cases the activity remains at a subclinical level, in 90% of those infected the immune system suppresses this activity within 0.5-2 years, but in general and in general, it is likely that the papillomavirus is present in the body of any person. The WHO lists the two most aggressive subtypes of HPV as the direct cause of cervical cancer in 90% of cases. According to H. zur Hausen, who was awarded the Nobel Prize for his research on HPV, cervical cancer is caused by these subtypes in 95%, and by all of them together – in 99.8%. The opposite statement is also true: in the absence of active HPV, cervical cancer does not occur.
The totality of HPV varieties known to date includes about two hundred types and strains (and this, apparently, is not all), more than thirty of which are oncogenic, and ten are characterized by high oncogenicity (especially HPV-16 and HPV-18).
“Ordinary” warts, papillomas and genital warts, the most typical manifestations of the presence of HPV, in the light of the above, no longer look quite ordinary. And it's certainly not harmless.