The scrotum is located in the perineum between the penis and the anus and is considered the most delicate and painful organ in the male body. For some reason, men protect this place only from blows, forgetting about dangerous urological pathologies that can cause many painful minutes, even if the organ was not injured. Among them, it is worth highlighting scrotal atheromas - cystic formations in the hairline area.
What is atheroma and atheromatosis
The content of the article
The scrotum is a male reproductive organ, which is a skin-muscular sac in which the testicles are located. The peculiarity of the organ is that it is covered with hair.
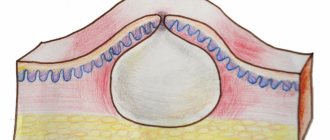
Atheroma is a common subcutaneous formation that is formed as a result of blockage of the sebaceous gland duct located in the hair follicle. The secretion (discharge) of the sebaceous gland accumulates in the pouch, causing stretching of the walls, which visually manifests itself in the form of a dense round formation that can be movable when pressed. If the mouth of the duct is not completely closed, the atheroma may look like a large blackhead.
Such formations most often occur in the area of dense hair, including in women, but in men atheromas are often observed in the scrotum area. This is due to the large number of sweat glands located in this area and poor air access due to tight clothing.
Being benign cystic neoplasms, atheromas often appear in the form of multiple structures, which in medicine is called atheromatosis.
Reasons for the formation of pimples
Light pimples on the testicles: what is it - a common question among male patients. White pimples on the testicles in men can appear at different ages. They have different shades, structures and shapes.
Most often, the formation of light-colored pimples is influenced by the following reasons:
- infectious pathologies;
- allergic reactions;
- unhealthy lifestyle leading to metabolic disorders;
- dysfunction of the sebaceous glands caused by hormonal imbalance and problems with the thyroid gland;
- skin diseases.
The scrotum has a large number of hair follicles that tend to become inflamed when they become infected. Most often this happens due to improper depilation of the groin area. With reduced immunity and hormonal problems, patients often encounter blockage of the sebaceous glands, which is accompanied by a progressive inflammatory process and acute pain.
In case of an allergic reaction, a man initially develops white dots on the scrotum, which subsequently turn red, begin to itch and cause discomfort when walking. When the allergen is eliminated, acne and inflammation quickly disappear. However, if the allergy occurs during long-term therapy with certain medications, auxiliary treatment will be required to remove chemicals from the man’s body.
Other reasons
White spots on the testicles in men can be Fordyce granules, which are cysts of the sebaceous glands. Most often they are formed in adolescents during a period of active hormonal changes in the body, but granules are also found in adult men.
Fordyce granules are localized in the following places:
- scrotum;
- penis;
- foreskin;
- oral mucosa.
Such white pimples are not life-threatening; they require special treatment. They are also not transmitted to the partner through sexual intercourse. If a man experiences psychological discomfort due to white bumps in the groin area, he can remove them using a laser.
Light growths on the testicles can appear as a result of improper hygiene. And this does not depend on the number of showers per day. A man can wash frequently, but use low-quality detergents, which cause dry skin and lead to the appearance of light-colored papules on the testicles. Also, the formation of pimples can be affected by synthetic underwear, which does not allow the skin to breathe and causes blockage of the sebaceous glands. Photos of neoplasms can be found on thematic forums.
Reasons for the formation of atheroma of the scrotum
Statistics say that about 20% of the stronger sex face the problem of atheromatosis of the scrotum, which is explained by the high content of the hormone testosterone in the male body, which is responsible for the functioning of the sebaceous glands.
In addition to the hormonal factor, there are several other reasons that cause the appearance of such an unpleasant neoplasm as atheroma. Most often, a cyst is formed due to:
- mechanical injury to the tissues of the scrotum or excessive friction of too tight underwear;
- inflammation in the area of the hair follicle;
- failure to comply with general hygiene rules;
- increased sweating in the scrotum area;
- spending a long time in trousers while sitting, especially if the room is hot or the car uses heated seats.
Pathology is diagnosed most often in young patients whose age does not exceed 35 years.
Treatment
Which doctor to go to to get a diagnosis is a question for many men. With such a problem, it is advisable to contact a venereologist, urologist, immunologist, or infectious disease specialist. After passing the examination, the doctor will prescribe a comprehensive treatment for the man.
If the whiteheads are found to be Fordyce granules or pearlescent papules, then no therapy will be required. The patient only needs to carefully monitor his lifestyle and prevent infection with inflammatory and infectious pathologies. The fungus is treated with antifungal agents and antimicrobial ointments. For dermatitis, you will need to identify the allergen that caused the disease and eliminate it. You will also need to take antihistamines.
Syphilitic neoplasms are treated with antibiotics, antimicrobial and immunostimulating agents. The patient must abstain from sexual intercourse for the period of treatment and carefully monitor his hygiene and lifestyle. Herpes is treated with antiviral agents, antibiotics, and antiseptic solutions.
If white dots appear due to a hormonal imbalance, the patient must undergo a hormonal examination. Based on its results, treatment tactics will be determined. Most often, men are prescribed hormonal drugs, immunostimulating drugs, and vitamin complexes. If the patient is bothered by regular blockages of the sebaceous glands, this may also indicate a hormonal imbalance, which has led to increased sweating.
Symptoms of atheroma of the scrotum
Initially, atheroma of the scrotum is defined as a small compaction in this area, which may be accompanied by minor pain. In the absence of rational treatment, the risk of formation of adjacent atheromas increases significantly, which ultimately leads to the formation of multiple cysts.
The consistency of the neoplasm is characterized as dense or jelly-like. Quite often, a pigmented point in the center of the compaction becomes a typical symptom of atheroma of the scrotum. As for mobility, an atheromatous neoplasm can be either fixed (linked to epidermal (skin) structures) or freely mobile.
The danger of scrotal atheroma lies in the likelihood of severe inflammation and infection in the area of stagnation of the sebaceous secretion of the gland. As a result, suppuration may develop, which is manifested by redness and intense pain. One of the unfavorable consequences of atheroma is scrotal abscess. This condition requires immediate surgery. If an abscess ruptures, you can lose your testicles.
How to treat acne on the penis
Before treating acne on the penis, you need to conduct a thorough diagnosis with a doctor. During it, the urologist examines and palpates the lumps in the groin area, makes a preliminary conclusion and refers to a dermatologist. He analyzes the pimple scraping using a biopsy, performs a spermogram, ultrasound of the scrotum or MRI. Then he makes a diagnosis and develops a treatment regimen. This is usually drug therapy. In some cases, surgical treatment may be necessary.
If a patient is diagnosed with candidiasis, he is prescribed a course of medications, ointments and creams for external use. Treatment lasts for 2-5 days. Aimed at eliminating discomfort.
In the case of genital herpes, a complete cure is impossible. Here, therapy is aimed at eliminating symptoms, rashes and pain through the use of antiviral drugs and immunomodulatory agents. In addition, the patient is not recommended to become hypothermic. Herbs that increase overall immunity can be used as additional remedies.
If you have herpes, you should not self-medicate or squeeze out pimples, as this will lead to the spread of the infectious disease throughout the body.
If white pimples on the penis are caused by pubic lice, then the doctor recommends anti-parasite creams and the use of antiseptics to the patient.
If trichophytosis or fungus is present, acne under the head is treated with antifungal and antihistamines. In this case, increased attention is directed to enhanced hygiene.
In the presence of painful enlarged lumps or cysts, painful boils with an increase in temperature and deterioration of health, surgical measures are used, medications are taken aimed at eliminating parasitic microorganisms and lowering the temperature. Additionally, vitamins are taken to increase immunity and improve the general condition of the body.
Diagnosis and treatment of atheroma of the scrotum
Diagnosis of atheroma is usually limited to visual and physical (palpation) examination, while treatment of atheroma requires mandatory removal of the cystic neoplasm.
In medical practice, several methods are used to eliminate atheroma of the scrotum:
- surgical opening and cleaning;
- electrocoagulation using an electric loop;
- laser destruction (destruction);
- Radio wave excision is the latest method using a radio wave knife.
Laser and radio wave treatment make it possible to remove atheroma very quickly without affecting healthy tissue. In addition, after using these devices there is no bleeding, since both the laser and radio waves seal the vessels. There is no residue left after removal of tumors or scars—everything heals very quickly. Since the urologist applies anesthesia, the patient does not feel anything.
What does normal look like?
It should be immediately noted that a pimple on an egg is a priori not the norm. But there are some factors due to which we can say that the situation is within reason. So, it is normal if the skin on the testicles resembles goose bumps. Small yellow pimples indicate clogged fatty pores, but this is also acceptable. Bright red blisters with pustules also do not signal danger, since their appearance can be caused by temperature condensation. Regular acne goes away in a few days, matures quickly and causes discomfort, mainly from an aesthetic point of view.
Relapse Prevention
To prevent the problem from recurring, you need to get tested for hormones - it is especially important to measure testosterone and undergo treatment to normalize hormonal levels. You also need to constantly take care of the cleanliness of your genitals and wear loose cotton underwear. This is enough to avoid relapse and another operation on the scrotum.
The choice of the optimal technique, as well as the appropriateness of a particular method of pain relief, is determined by the doctor. Medical offers the services of a highly qualified specialist in the field of urology and andrology. Urologists will perform a full diagnosis and treatment of atheroma of the scrotum. Removal of any tumors is carried out with a laser or radio knife.
The anomaly is in the details
But if pimples on the testicles resemble genital warts, then this is already an alarm bell. In addition, you should pay attention to the appearance of swelling in the genital area. The lion's share of such compactions is not dangerous, but there is always a risk of ordinary formations becoming malignant. If a hard lump is felt, you should consult a doctor. The need for medical consultation is especially clearly felt when the day before there was unprotected sexual intercourse. After all, acne can be a consequence of it and signal an infection with a sexually transmitted disease.
Symptoms of pathology
If the manifestations of formations bother you or there are accompanying symptoms (itching, burning, peeling of the testicles and penis), you should consult a dermatologist. He also prescribes treatment.
Rarely, additional consultation with another specialist (urologist, endocrinologist, vascular surgeon) is needed. This is the only way to make sure that men's health is safe.
You should definitely go to the hospital if:
- concerns about swelling and itching;
- red or flesh-colored spots on the scrotum merge and form ulcers;
- the epithelium on the testicles is painful when touched;
- bubbles filled with bloody fluid appeared;
- the spots do not go away on their own for more than 2 weeks.
Black spots on the scrotum in children
The appearance of dark spots on the testicles of a child or teenager can be caused by the same reasons, but most often it is an allergy or clogged pores. If they do not cause burning, itching, or increase in size, then there is no cause for concern. It is necessary to explain to the child that comedones should not be touched or squeezed out, especially those that itch. Red, white pimples in the groin of newborns are manifestations of prickly heat.
In a boy, the appearance of dark spots may be associated with wearing diapers. Parents should let their baby run around in onesies more often; change the diaper more often. The moist skin of the scrotum is a favorable environment for various types of rashes.
READ ALSO: Possible causes of red rashes on the elbow joints and crook of the arm in children
Rarely, after bathing with potassium permanganate, rough dark patches may appear on the child’s skin. This is due to the fact that the manganese crystals are not completely dissolved and leave pinpoint burns.
Expert opinion: Contact dermatitis is a common cause of red rashes and small pimples on the scrotum and penis. Associated symptoms are burning and itching in the groin and anal area.” Changes in the epithelium of the genital organs in adults and children often result from interaction with synthetic fabrics and household chemicals. Contact dermatitis is a kind of allergic reaction.
What is the treatment for inflammatory diseases of the scrotum?
Treatment of epididymitis, orchitis, orchiepididymitis and deferentitis is carried out primarily with antibiotics, since their main cause is various infections. The choice of antibiotic for an acute inflammatory process is carried out empirically, taking into account the known age-related characteristics of the causative infections. Upon receipt of the results of microbiological studies and analysis of the sensitivity of the isolated microflora to antibiotics, it is possible to adjust antibiotic therapy, change its duration, dosages of drugs, and sometimes the drugs themselves and their combinations.
Along with antibiotics, non-steroidal anti-inflammatory drugs (indomethacin, diclofenac, Celebrex, etc.) are prescribed in order to reduce inflammatory swelling, pain and quickly reverse the development of inflammatory changes. For severe pain, a blockade of the spermatic cord with a local anesthetic (lidocaine, prilocaine, marcaine) is used, which significantly reduces pain. All patients are recommended to wear tight panties (swimming trunks) that tighten the scrotum during treatment. This promotes better blood and lymph flow in the scrotum and accelerates the reverse development of inflammation.
In the presence of ulcers or abscesses of the testicle and its epididymis, as well as in chronic recurrent epididymitis, which is difficult to treat, in the case of testicular tuberculosis, surgical treatment is used. It may involve opening and draining abscesses, partial or complete removal of the testicle and/or its epididymis. The use of various methods of physiotherapy for inflammatory diseases of the scrotal organs has not proven its effectiveness in correctly conducted scientific studies and is not included in the international standards for the treatment of epididymitis, orchitis and orchiepididymitis. In this regard, we do not use physiotherapeutic methods for treating these diseases in our practice.
How is inflammatory diseases of the scrotum organs diagnosed?
The basis for diagnosing diseases of the testicle, its epididymis and spermatic cord is a physical examination (primarily palpation or palpation). The leading auxiliary methods are diaphanoscopy and ultrasound examination of the scrotum. All of these methods are completely painless, and their correct use and proper interpretation allow an accurate diagnosis to be made in the vast majority of cases. In recent years, ultrasound of the scrotum, as a much more informative and accurate method, has practically replaced diaphanoscopy.
To establish the causes of epididymitis, orchitis and orchiepididymitis, a general analysis and culture of urine for microflora are required, and sometimes sperm (ejaculate) is analyzed for the presence of various infections. Tests are performed for the presence of sexually transmitted diseases. If there is suspicion, an examination is carried out for the presence of Mycobacterium tuberculosis in the urine and/or ejaculate. If a testicular tumor is suspected, blood tests are performed for the appropriate tumor markers. Only a correctly constructed set of diagnostic measures makes it possible to establish an accurate diagnosis and carry out the most effective treatment. Be sure to contact a urologist!