Montgomery's tubercles are found around the breast halos and appear differently throughout a woman's life. Clearly visible in the photo, small nodular formations around the nipple appear in girls in the womb, but are almost invisible.
During pregnancy and hormonal changes, the tubercles become distinct, which sometimes alarms women. A completely physiological phenomenon can cause discomfort or may indicate problems in the body.
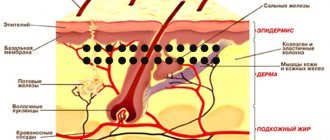
Montgomery tubercles are faint glandular formations around the colored areola of the nipple. Normally, the nodules are distinguished by color (much darker or lighter) or rise above the surface of the skin.
Montgomery tubercles: photo
The number of formations is individual and can range from 4 to 15 pieces. Less commonly, up to 30 tubercles are observed on each breast. The formations are neither sweat glands nor mammary glands.
Microscopic ducts secrete a liquid secretion that lubricates and disinfects the delicate skin of the halos, preventing drying out, cracking and infection of the surface. The presence of Montgomery tubercles is a physiological norm. Pathology is any pain, inflammation or suppuration of the glands.
Kinds
Natural anatomical formations have a wide range of norms: from quantity to size and appearance. In different women, Montgomery's tubercles can be pronounced and resemble small nipples or be almost invisible on the skin. Differences in their structure and appearance are noted during the period of hormonal changes in a woman’s body.
Photos of Montgomery tubercles during pregnancy, which proceeds without deviations from the norm, show round or elongated formations with a diameter of 2 to 8 mm.
The nodules have limited mobility when the skin is pulled or displaced, have a soft consistency, easily move deep into the tissue when pressed and immediately return to their original place on their own.
For the first time, the nodules around the areola were described by obstetrician William Montgomery in 1937, calling them “a constellation of decorative nipples” and for the first time linking their occurrence in women with the fact of pregnancy. The name of the physiological phenomenon is still strongly associated with the name of the Irish professor.
4.Prevention of breast diseases
There are a number of simple rules that, if followed, will help maintain breast health and promptly identify possible problems:
- Women over 40 years of age should have an annual mammogram.
- Women at risk for breast disease should have screening mammography, starting at a younger age, at least once a year. Additionally, it is recommended to do an ultrasound of the mammary glands. In particularly high-risk cases, such as women who have a greater than 20% risk of developing breast cancer, an annual breast MRI may be required. Your doctor will help you decide on a set of specific diagnostic methods after analyzing all the information about your health.
- During an annual preventive examination of the body, women over 20 years of age should visit a mammologist who will examine the mammary glands.
Stages and degrees
The appearance and functions of the secretory glands around the nipples naturally change throughout life and have the following stages:
- Montgomery's tubercles actively appear during puberty, at the beginning of the formation and active growth of mammary glands in adolescents. When the active growth phase ends, the secretory function decreases and the formations become less noticeable.
- Photos of Montgomery's tubercles during pregnancy are shown differently. During the period of activation of reproductive functions, formations become noticeable in almost all expectant mothers. They may increase in size, swell to resemble pimples, or change color under the skin.
- The formations significantly change their appearance already in the first decade of conception and can serve as the first diagnostic sign of pregnancy. The pigmentation becomes brighter, the tubercles under the skin swell and increase in size.
- The glands are also activated immediately after childbirth, as a sign of the readiness of the mammary glands for lactation. Doctors note increased milk production and active feeding of infants in women with a large number of Montgomery formations.
- Sometimes there is swelling and enlargement of micro glands on the breast before the start of the monthly cycle. This individual feature also refers to the physiological norm. After the end of menstruation, such symptoms quickly disappear.
- Sometimes a regular increase in tubercles in women who have given birth reflects the onset of ovulation.
Any change in the Montgomery tubercles outside of these cycles indicates either hormonal changes in the body or warns of possible trouble, which requires mandatory examination.
Normal sexual development, pregnancy, and breastfeeding in some cases occur without obvious activation of the tubercles. The increased size of the Montgomery glands, their large number and prominence against the background of the nipple are not necessary conditions for the success of reproductive functions or breastfeeding.
How to get rid of Montgomery tubercles?
If Montgomery's tubercles become noticeable as pregnancy progresses, this is considered normal and no special action is required. If in some women they increase in the first weeks of pregnancy, and in others almost with the onset of lactation, then normally in all they return to their normal appearance with the cessation of the lactation period.
When Montgomery's tubercles attract attention not just because of their increased size, but because of inflammation, itching or pain, then getting rid of them should be entrusted to a professional physician.
Local bactericidal and anti-inflammatory drugs are usually prescribed, as well as various methods of herbal medicine and homeopathy. The latter are especially relevant if inflammation develops during pregnancy. Physiotherapeutic procedures may also be prescribed to treat inflamed Montgomery tubercles
Modern medicine also offers women such a service as surgical of Montgomery tubercles An indication for this is aesthetically unsightly bumps left after lactation or formed during puberty. At the woman’s request, the work will be carried out by a plastic surgeon, leaving scars that are almost invisible to the human eye. However, no matter how attractive this prospect may be, it is worth thinking carefully - although the glands are recognized as rudimentary, they still serve some purpose during the period of feeding a child.
Symptoms
After pregnancy, most women first notice the appearance of Montgomery formations in the nipple halo. The tubercles become lighter or darker than the surrounding tissues, protrude or take the form of micro-papillae. Natural changes may be accompanied by slight discomfort or temporary itching.
Quite rarely, the development of inflammatory processes at the exit sites of secretory channels is noted. The liquid secreted by the Montgomery tubercles has little antibacterial activity, is quite fluid and is excreted in minimal, almost imperceptible quantities, so pathologies of these glands are extremely rare.
Inflammation of the Montgomery tubercles: symptoms
The following symptoms indicate the presence of inflammation:
- Pain with minor mechanical impact.
- Change in skin color over the tubercles: redness, sometimes cyanosis.
- Increased body temperature (fever) or a feeling of overheating in the nipple area.
- The presence of cloudy or bloody discharge when pressed.
- Small rash around the nipple, cracks or growths.
- Change in color of the halos (usually redness).
Any of the listed symptoms is a deviation from the norm and requires consultation with a mammologist or dermatologist.
Fibroadenoma - tests and diagnosis
During a clinical physical examination, your doctor will examine both breasts. A fibroadenoma usually feels like a moving lump.
The examination is followed by an ultrasound examination, which accurately determines the size of the fibroadenoma, its shape, the appearance of the edge, its relationship to the surrounding tissue and a rough estimate of the structure of the fibroadenoma.
When a more precise analysis of the structure is required, cytological and pathohistological examination of fibroadenoma is performed.
During a cytological puncture (biopsy), a sample is taken for histological analysis. A biopsy is used to exclude or confirm malignancy of the tumor.
Fibroadenomas can be very durable in structure. Therefore, it is difficult to obtain cells with a thin needle that can be used to make a real diagnosis. A wide needle biopsy is performed under local anesthesia.
A thick needle is inserted into the fibroadenoma tissue approximately 5-6 times. The procedure is painless, there is no risk of complications. The applied bandage can be removed the very next day.
Reasons for appearance
The prerequisite for the appearance of Montgomery tubercles in pregnant women is exclusively hormonal changes in the body, preparing the mammary glands for the process of lactation and feeding.
In the case of the development of an inflammatory process diagnosed as a disease, there are several reasons:
- Blockage of the gland's excretory channel is the most common cause of complaints. The nodules turn into pimples with white contents, like acne.
- More serious and deep blockage leads to the formation of atheroma - a subcutaneous vesicle filled with exudate. It is most often formed in the sebaceous glands and milk ducts.
- Due to trauma to thin skin or cracked nipples, boils similar to inflamed Montgomery tubercles may appear.
- Malignant moles in the nipple halo, the presence of benign or pathological tissues under the skin also lead to inflammation of the nodules.
The immune system of a pregnant woman is vulnerable, the body copes worse with even minor infections. Thus, the natural itching of the nipples from an increase in the volume of the mammary gland can provoke microtraumas; the delicate skin dries out and cracks during the feeding period. Microorganisms entering wounds easily provoke inflammation and suppuration.
What types of seals are there?
Diseases that cause chest pain are varied. The main ones:
- Benign neoplasm, for example, adenoma and others. Several such neoplasms can form and, accordingly, be accompanied by pain. In some cases, pain in the chest appears during menstruation.
- Cyst formation. This is a spherical and oval pathological cavity that has a wall and contents. As a rule, the presence of a cyst is manifested by pain and discharge from the nipple.
- Mastopathy. The pathology can be nodular or diffuse. Hormonal imbalance leads to the appearance of compactions, of which there may be several. They can be palpated, pain occurs, the mammary gland swells, and discharge is observed from the nipple.
- Neoplasm of a malignant nature. It is characterized by the presence of a compaction, the shape of the breast changes, the nipple is deformed, there is discharge from it, the skin texture in the projection of the compaction changes. With significant development of the disease and the presence of metastases, the size of neighboring lymph nodes increases. They also become denser, and pain occurs on palpation. If we are talking about the initial stages of oncology, the symptoms are often mild.
Diagnostics
The presence of a pathological process is determined by a gynecologist observing the pregnancy.
Primary diagnosis of Montgomery tubercles is carried out visually and by palpation of inflamed areas of the chest and lymph nodes.
To determine the cause and extent of damage to the areola nodules, procedures may be prescribed:
- ultrasound examination;
- mammography (breast x-ray);
- blood test and bacterial culture of secretions.
Mammography
Based on the test results, the presence or absence of the disease, its degree and the need for further examinations are determined.
What to do if you don’t have your period and the test is negative
If your period is delayed by only a couple of days, do not rush to draw conclusions about the onset of pregnancy or the appearance of any diseases. When menstruation does not start for 5-7 days, you can take 1-2 pregnancy tests to ensure the accuracy of the result. If both tests turn out to be negative, this is a reason to contact a gynecologist as soon as possible. In this case, you should not wait long in line at a public clinic; it is best to make an appointment at a paid hospital.
The most important thing in such a situation is not to try to induce menstruation yourself using traditional methods, as this can lead to severe uncontrolled bleeding and exacerbation of a gynecological disease, if any. The menstrual cycle is regulated by hormones, so it is possible to interfere with its course only with the help of special medications prescribed by the attending physician.
When to see a doctor
Reasons for seeking advice from a therapist or gynecologist monitoring pregnancy include the following conditions:
- pain, burning, itching or feeling of fullness in the breast tissue;
- change in color of the tubercles themselves, nipples, halos or surrounding skin;
- a sharp increase in the size of the Montgomery glands without provoking factors;
- the appearance of red or pink sinuous stripes on the surface of the chest, halos.
When carrying out diagnostics, inflammation of Montgomery's nodules is differentiated from the following pathologies that are not related to the glandular tubercles:
- acne as a result of blockage of the sebaceous glands;
- dermatological problems: eczema, dermatitis, psoriasis;
- allergic rash.
Based on the results of the initial examination, a consultation with a more specialized specialist may be scheduled: a dermatologist, allergist, endocrinologist. The appearance of small, growing warts may be associated with hormonal imbalances, wearing uncomfortable, synthetic clothing, or require consultation with an oncologist.
If your chest hurts, but the test is negative and your period is late
The most common cause of chest pain due to a delay in menstruation is pregnancy. But if the test turns out to be negative, the unpleasant condition could appear for one of the following reasons:
- mastopathy;
- frequent and prolonged stress;
- consequences of recent infectious diseases;
- consequences of heavy physical activity;
- consequences of breast surgery;
- acclimatization period;
- diseases of the female genital organs;
- starting new oral contraceptives or other hormonal medications;
- ovarian dysfunction;
- oncology.
IMPORTANT! If a delay in menstruation with chest pain repeats several cycles in a row, you should consult a gynecologist and mammologist as soon as possible.
Prevention
It is impossible to avoid the manifestation of physiological changes during pregnancy. After lactation ends, Montgomery's tubercles usually shrink and return to their pre-pregnancy state.
Proper breast care during pregnancy helps prevent clogged or infected glands:
- daily washing of the glands with warm water without soap and shower gels;
- using glycerin compounds, baby cream, or a doctor-recommended product to soften the skin of the breasts and nipples;
- contrast shower for the chest to increase blood flow and strengthen delicate skin;
- Regular use of pads in your bra if your milk is leaking or your nipples are sensitive.
Mammologists and gynecologists strongly recommend that pregnant women carefully select underwear for their growing breasts. Squeezing, tugging of the mammary glands or constant contact of the skin with synthetic fabric is unacceptable.
Montgomery bumps are normal, pimple-like pores on the surface of the areola. Named after the Irish obstetrician who first described them in medical literature in 1837, these bumps on the areola extend from the areolar glands (also known as Montgomery's glands) and are often most noticeable during pregnancy and breastfeeding.
As a type of sebaceous gland, these parts of the nipple function primarily to produce secretions that moisturize and protect the skin. Along with the occasional small amount of milk, Montgomery's bumps secrete a clear or cloudy oily substance that helps prevent infection.
What are the tubercles of Montgomery?
Montgomery's tubercles are located on the surface of the areola, the round area of skin surrounding the nipple. They can be flesh-colored, pink, red, white or yellowish in color and are usually 1 to 2 millimeters in diameter.
One breast may have more bumps than the other. They can be invisible or, on the contrary, be pronounced depending on certain factors - from temperature to hormonal fluctuations.
Some have more Montgomery tubercles than others. Typically, a woman may have between four and 28 Montgomery tubercles.
Why can Montgomery's tubercles get larger?
Montgomery's tubercles become noticeable under certain conditions:
- When the bumps are touched: stimulation or even pressure from clothing can cause the tiny bumps to swell.
- In the cold: A sudden drop in temperature can cause the areolar glands to become more visible, like goosebumps on the skin.
- During puberty: Montgomery tubercles may appear during puberty and during certain phases of the menstrual cycle, as the activity of the areolar glands increases with the amount of estrogen in the female body.
- During pregnancy: Along with darkening of the nipples and breast enlargement, the appearance of Montgomery's bumps is an early sign of pregnancy. These areolas become noticeable in 30-50% of pregnant women.
Breast changes during pregnancy and breastfeeding
Montgomery's tubercles serve a primary purpose when feeding a baby. They produce more oil after birth, which helps keep nipples moist and elastic for easier breastfeeding.
These secretions also contain antibacterial properties that protect the mother's breasts and the baby from a number of infections.
The fluid that comes from Montgomery's tubercles may even aid in feeding. Research shows that babies eat more from the breast when the areolar glands secrete more fluid. The oils are believed to include olfactory (aromatic) compounds that help stimulate the baby to feed on breast milk.
Sometimes Montgomery's bumps become so large that they look like pimples filled with fluid. You may even want to try to squeeze them out, but you shouldn’t do this: this can lead to infection.
To keep your nipples and areolas clean and moist during pregnancy and breastfeeding, try these tips:
- Wash your breasts with clean water and a mild cleanser. Avoid using soaps and disinfectants, which can dry out and irritate your skin.
- Do not use astringents to clean your nipples as this may interfere with the production of oils from the areolar glands.
- If your nipples and areolas are cracked and sore, use modified lanolin in moderation. This will help with healing.
- You can express a few drops of milk after breastfeeding and rub it into your nipple and areola for extra hydration.
- Breast shells can also help protect sore nipples between breastfeeding sessions. Nipple shields, on the other hand, provide protection during breastfeeding.
Signs of infection
Although they produce germ-fighting secretions, Montgomery's tubercles can become clogged and become infected. This usually occurs when bacteria from the baby's hands, ointments or toiletries, clothing, or even the baby's mouth enters small breaks in the mother's skin while breastfeeding.
The glands can become inflamed not necessarily during breastfeeding. Diabetes, smoking, or nipple piercings increase the risk of developing subareolar abscesses, which are infected tumors in the areolar glands.
Less commonly, Montgomery cysts can occur when the glands are blocked. Typically found in teenagers, Montgomery cysts are often harmless and go away on their own, but may require treatment if they become infected.
Signs that you should seek treatment:
- Swollen, tender lump under the areola;
- Redness and itching;
- Brown or cloudy discharge from Montgomery's tubercles or nipple;
- Fever or general feeling of malaise.
Sometimes other sebaceous glands on the areola can become enlarged in a harmless condition called sebaceous gland hyperplasia. While Montgomery's tubercles usually appear as uniformly sized bumps throughout the areola, sebaceous gland hyperplasia usually appears as a flat, whitish patch.
Treatment methods
Montgomery's tubercles, when slightly inflamed, often return to normal on their own if hygiene rules are observed, without requiring special treatment.
For more serious disorders shown in the photo, after establishing the infectious cause of the disease and its causative agent, complex therapy will be required. Any medications during pregnancy are used strictly as prescribed by the doctor in the indicated dosages.
It is prohibited to smear the breasts with creams and ointments, as well as warm the breasts if the Montgomery tubercles are inflamed.
In case of inflammation of the Montgomery tubercles, the following is prohibited:
- warm up the inflamed area;
- squeeze out or cauterize the place of suppuration with alcohol compounds;
- apply any creams, ointments (including Vishnevsky ointment) before visiting a doctor;
- take homeopathic medicines or home remedies or traditional medicine internally or externally.
Acceptable breast treatment before visiting a specialist consists of washing with warm water and soap and a single treatment of the nipples with hydrogen peroxide. Further treatment is prescribed after an accurate diagnosis has been established.
Medications
Any medications during pregnancy are, if possible, replaced with herbal medicine, physiotherapy, and hygiene procedures. After establishing the causes of the disease, the doctor will be able to advise the most effective of these methods. If there is persistent damage to the Montgomery tubercles, drug treatment will be required.
To treat inflammation, use:
| antibiotics | Prescribed in extreme cases, only from the 2nd trimester of pregnancy. |
| ointments: Levomekol, Dioxidin, Bepanten | During lactation, the issue of stopping breastfeeding is considered individually. |
| washing or lotion | With antibiotic solutions in ampoules: Ceftriaxone, Cefepime. |
| vitamin complexes: Multitabs, Vitrum, Alphabet | Preference is given to drugs created specifically for use during pregnancy. |
If necessary, antihistamines may be prescribed. Any medications for inflammation of the Montgomery tubercles are taken under the supervision of the doctor who prescribed the treatment. In pregnant women, adverse and allergic reactions to medications occur more often than in general cases.
Traditional methods
Any warming procedures, hot compresses and cauterization are contraindicated for inflammation of the Montgomery glands. Such treatment aggravates the problem, stimulating the spread of infection from the tubercles into the soft tissues and skin. The use of medicinal herbs and folk remedies externally or internally should be agreed with a doctor and serve as an addition to therapy.
Home remedies to speed up the treatment of inflammation of Montgomery's tubercles:
- to relieve pain, itching, heaviness in the mammary glands, it is allowed to apply a cloth soaked in slightly warm water to the affected areas for 20 minutes several times a day or at night;
- strengthening the drinking regime and reducing sugar consumption helps to quickly cleanse the blood and remove toxic substances from the body;
- Hydrogen peroxide is chosen from disinfectants as the most gentle option for delicate areas of the skin;
- temporarily refrain from washing with soap or shower products, reducing drying of the affected areas and contact with chemical components.
The use of aloe gel and vegetable oils (lavender, coconut) with healing properties is possible only if the cause of inflammation is not fungus or bacteria. When breastfeeding, any substance applied to the nipple and areola should be recommended by a doctor.
Other methods
In rare cases, when inflammation threatens to infect healthy tissues, atheroma or painful boils form, surgical intervention is recommended. Modern methods make it possible to remove such formations without bleeding, long postoperative recovery and the danger of sepsis. Surgery is performed using the traditional method or laser.
Montgomery tubercles, photos during pregnancy and after childbirth show that the glands do not always return to their original state. For some women, nodules cause aesthetic discomfort. In such cases, surgical removal is indicated. The cosmetic surgery is minimally invasive, takes place without complications and leaves behind subtle white marks on the halo.
Before deciding to undergo surgery for aesthetic reasons, you should consider the risks of loss of sensation in the nipple area, as well as possible problems when breastfeeding your next child.
Pathological conditions
Some pimples around and inside the nipple of the breast are a consequence of the development of pathology.
- Eczema. A complicated form of allergy, the result of excessive friction or hormonal imbalance.
- Neurodermatitis. An allergic reaction develops after nervous stress and mental disorders.
- Atheroma. A subcutaneous clot of adipose tissue forms not only on the dermis, but also on the nipples. Blockage of the duct leads to the accumulation of secretions, which leads to the formation of a wen. The symptom is the presence of a rolling ball inside.
- Telit. Redness of the entire surface of the nipple is called by this medical term.
- Mastitis. The inflammation is located inside the mammary gland and spreads to the nipple and areola (blood is often released from them).
White pimples that appear around the nipples in women are a sign of furunculosis. Entering the epidermis through wounds, pathogenic microflora causes inflammation, often transforming into a purulent process.
READ ALSO: Pimples on the nipples: causes and treatment of whiteheads
If they appear, then urgent treatment is needed: some nodules lead to necrotic processes and abscesses. Doctors recommend opening pustules, but only under the supervision of a specialist.
There are three answers to the question of which doctor you should contact. When there is a suspicion that the activity of the mammary gland is impaired, then go to a mammologist, or a skin specialist - a dermatologist. If you suspect the development of a neoplasm, it is better to visit an oncologist.
Paget's disease is a malignant disease that is accompanied by the appearance of ulcers and pain. In most patients, the pathology is localized on the nipple, less often - near the areola.
Conclusion
Suddenly appearing pimples on the nipples in women are mainly related to anatomical formations, but there are also manifestations that are caused by diseases.
Doctors warn! Shocking statistics - it has been established that more than 74% of skin diseases are a sign of parasite infection (Accarida, Giardia, Toxocara). Worms cause enormous harm to the body, and the first to suffer is our immune system, which should protect the body from various diseases. The head of the Institute of Parasitology shared the secret of how to quickly get rid of them and cleanse your skin, it turns out that’s enough. Read more .
White bumps are the consequences of the effects of herpes on the body, and doctors can only eliminate them with medication. Purulent processes are also dangerous, so they should be neutralized as soon as possible.
News MirTesen
Possible complications
Any alarming changes in the condition of the breasts, nipples and halos should be a reason to consult a gynecologist. If the infection is left unattended, if the pregnant woman has insufficient immunity, it can quickly spread to neighboring tissues. Atheromas and boils, with improper external healing, tend to flow inward rather than outward.
A slight inflammation threatens to turn into a source of infection for the woman’s body and the unborn child. Even more alarming consequences can await a woman if the cause of inflammation of the Montgomery tubercles is benign or malignant tissue degeneration.
As the tumor grows, it compresses and poisons neighboring tissues, causing protrusion and painful nodules. Such a sign can help make a diagnosis at an early stage, when treatment is more effective, less traumatic, and gives a chance to maintain the pregnancy and prolong the woman’s life.
Montgomery tubercles are a natural evolutionary adaptation of the human body to breastfeeding offspring. Photos of nodules that increase during pregnancy, lactation and disappear afterwards prove this connection.
Many scientists call the Montgomery glands rudimentary, without important functions. Others are working to use enzymes produced by the tubercles to improve survival and weight gain in premature babies.
Article design: Natalie Podolskaya
Diagnosis of the reasons for the delay
To make an accurate diagnosis and identify the cause of the delay, the doctor will need additional examinations:
- Examination in a gynecological chair;
- Blood tests: beta HCG, TSH, T4, a complex of gynecological hormones (6 indicators);
- Ultrasound of the pelvic organs. This will help eliminate the possibility of pregnancy, tumor formations in the genital organs and other reasons that can lead to a delay in menstruation.
Based on the examination results, the doctor will conduct a consultation, adjust the prescribed treatment or prescribe a new one. After treatment and the onset of a new cycle, you will definitely need to come to the doctor for a second consultation for examination.
The most important thing when your period is late is not to start panicking. If menstruation is delayed by only 2-3 days, this is a minor and completely natural deviation. If your period does not come after 5-7 days, do not try to solve the problem yourself and immediately contact a gynecologist.
Montgomery glands during menstruation
The process of puberty is accompanied by hormonal changes. The tubercles first become noticeable when the mammary glands are actively developing and take on an “adult” appearance. If such lumps become noticeable in a girl, it means that the process of egg formation has begun in her body; the uterus and ovaries are ready for conception. The glands are influenced by the same hormones (FSH and LH) as the reproductive organs, so the tubercles are especially noticeable during the menstrual cycle (during the formation period).
While the maturation period lasts, the glands protrude especially. This is due to hormonal activity. But after menstruation is established and the hormonal levels return to normal, the tubercles become almost invisible. In the future, until the moment of conception, they should not change. Before menstruation, the glands remain invisible.
If on critical days they swell or thicken, this indicates either a disruption in the production of hormones, or the individual characteristics of the body . In this case, the girl should have her mammary glands and thyroid gland examined. If the lumps are clearly visible without pregnancy and this is not related to hormones or the specifics of the body, then this is a sign of a pathological process developing in the mammary gland.
Fibroadenoma - surgery
Fibroadenomas of very large sizes (the relative ratio of the size of the fibroadenoma and the breast itself is important), which grow quickly and are painful, must be removed surgically. Sometimes this is done for psychological reasons.
Your doctor may recommend surgery to remove fibroadenoma if you think the test results are alarming.
Fibroadenoma removal procedures include:
- With cryoablation, the doctor inserts a thin “stick” through the skin into the fibroadenoma and freezes the tissue with gas.
- Some fibroadenomas are too large to be frozen, and cryoablation is only used if the diagnosis confirms that it is a fibroadenoma.
- The surgeon sends the removed breast tissue to the laboratory for examination.
After fibroadenoma is removed, it is possible for them to develop again - they recur.
It is necessary to check your breasts regularly, regardless of whether there was fibroadenoma or not.
If lumps form on your breasts, consult your doctor to rule out the possibility of a malignant neoplasm.
Breast ultrasound
If the woman is under 30 years old, the doctor may recommend an ultrasound instead of a mammogram because dense breast tissue in younger women is more difficult to examine with a mammograph.
If the woman is over 30 years old, the doctor will recommend a mammogram of both breasts followed by an ultrasound to evaluate the tumor.
Using an ultrasound, your doctor can determine whether a breast lump is solid or filled with fluid. When the mass is hard, there is a high probability that it is a fibroadenoma. A mass full of fluid indicates a cyst.