Pathogenesis of lentigo. Types of disease Treatment of the disease and prevention of lentigo
Many of us have to deal with the appearance of pigment spots of various sizes on our bodies throughout our lives. Pigmented spots on the body or lentigo
– pathology of hereditary or acquired origin. The appearance of spots is associated with the activation at a certain stage of external and internal factors that are directly and indirectly related to the development of the disease. Pigment spots arise as a result of an increase in the level of the skin pigment melanin in the basal layer of the epidermis, in the upper chromatophores of the skin.
The main reasons for the development of lentigo
There are many factors, each of which has a decisive influence on the appearance of age spots.
Medicine has not definitively established the true causes of age spots on the human body. It has been established that most of the spots appear on the human body due to age-related changes, under the influence of active ultraviolet radiation of solar origin. The appearance of age spots in adolescence, the so-called juvenile lentigo
, has a different clinical nature.
The pathology is observed throughout the life of almost every person. The appearance of age spots in adolescence is quite rare. The number of cases of juvenile lentigo
is 5-10% of the total number of cases of pathology development. With age, the damage to the skin increases markedly, depending on the person’s age and lifestyle.
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Solar lentigo (solar lentigosis, age-related lentigosis, actinic lentigine, sun spots) is a hypermelanosis, manifested by foci of darkening of various diameters as a result of prolonged exposure to ultraviolet radiation on the skin.
In our company you can purchase the following equipment for the treatment of solar lentigo:
- M22 (Lumenis)
- Fraxel (Solta Medical)
- FotoFinder (FotoFinder)
Solar lentigo is a widespread pigmentary pathology. For example, in the United States, lentigenic changes are observed in 90% of people with fair skin over the age of 60 years and in 20% under 35 years of age. The risk of solar lentigo is increased in people who spend a lot of time in the sun. Moreover, a separate part of the body can be affected - for example, the left hand of professional drivers. It was also noted that lentigo appears in 50% of patients after long-term PUVA therapy for psoriasis (for at least 5 years).
Question answer
Yes, but initially it is recommended to consult a dermatologist. He will prescribe suitable medications. For example, whitening creams with hydroquinone 4% or retinol have worked well. You can supplement therapy with traditional methods, but they will not be able to fully cope with the problem. You should also understand that treatment with such creams will take a lot of time.
Yes it is possible. Therefore, go to the doctor for diagnosis in a timely manner. Degeneration is observed in 4% of patients. A malignant formation usually has smooth edges and is dark in color. The size usually grows and can reach up to 20 cm.
In the table of classification of pathologies, lentigo was included in the group of diseases associated with increased levels of melanin and pigmentation disorders. Assigned number L81.
Etiology and pathogenesis of lentigo
The main cause of solar lentigo is chronic exposure solar radiation . Changes do not occur immediately - they accumulate over many years of ultraviolet irradiation of exposed areas of the face and body. The likelihood of lentigo increases if a person has light skin of Fitzpatrick phototype I or II. Solar lentigo can also occur after long periods of visiting a solarium .
Quite often, lentigo appears after PUVA therapy (psoralen (P) + ultraviolet A (UVA) = PUVA or PUVA) - therapeutic exposure of the skin to ultraviolet A (UVA) with preliminary intake of a photosensitizer (psoralen). These pigmented lesions are called PUVA lentigo, and they are a side effect of phototherapy for psoriasis.
Microscopy of solar lentigo lesions reveals elongation of the epidermal ridges (lentiginous hyperplasia), an increase in the number of melanocytes that produce excess pigment, as well as an increase in the number of melanophages - macrophages that have absorbed the pigment and turned dark. Atypical melanocytes are not normally detected in solar lentigo.
In addition to solar and PUVA lentigo, simple lentigo (lentigo simplex), the causes of which have not been established, as well as radiation lentigo (radiation lentigo) after high-dose radiotherapy can occur on the skin. In the future, any of these neoplasms can transform into lentigo maligna, so they should be treated with special attention. Primary differential diagnosis between ordinary and malignant lentigo is carried out with high efficiency using FotoFinder .
In some cases, lentigo is a sign of a hereditary disease - for example, LEOPARD syndrome. LEOPARD is an acronym whose letters describe the symptoms of the disease: L (lentigo), E (cardiac conduction disorder), O (ocular hypertelorism), P (pulmonary stenosis), A (genital anomalies), R (slow growth), D (deafness).
Diagnosis of the disease
All changes that occur on the surface of the skin, first of all, should not be ignored by the patient himself. The appearance of suspicious lesions in the form of rashes, spots, swellings requires the use of a biopsy (diagnostic method) to determine the causes and the presence of malignant melanocytes. When performing a biopsy, the following information must be included in the report:
- Place of defeat.
- Diagnosis.
- Engaging research boundaries.
- Breslau level.
Additional research methods for biopsy are:
- A morphological method of research in which a fragment of infected tissue taken by excision is studied.
- Dermatoscuopia. This involves studying the pigment spot under an electron microscope.
- Calculation of tumor marker levels.
During the study, the condition of the patient’s entire body, the diseases that exist or previously existed, and the area of skin (a layer is removed) where the tumor is present are studied. Blood is taken for analysis to identify the presence of material in it that can create all the necessary conditions for the formation of a tumor in the cell. If the result is positive, after a biopsy, specialists prescribe a course of complex treatment with chemotherapy, radiation therapy, and, if necessary, surgery with the use of cytostatics.
Clinical manifestations of lentiginosis
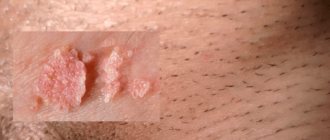
Lentigenic lesions appear as flat or slightly concave round spots of varying diameters and colors ranging from light brown to dark brown. They usually appear on open areas of the skin—the face, the backs of the arms and hands, and the upper half of the torso ( Fig. 1 ).
Immediately after their appearance, their size does not exceed 5 mm, but as they “age”, solar lentigines become larger, darker and gradually merge into large spots. They may contain areas of normal skin or be separated by fine wrinkles. Skin affected by lentigo appears loose and inelastic—in general, it looks worse than it should for its age ( Fig. 2 ). The epidermis becomes thinner and dry, and the skin color becomes unevenly patchy.
Lentigo can occur after a long course of PUVA therapy for psoriasis - from six months or more. In this case, pigment spots are similar to solar lentigo, but have irregular contours - sometimes they can be confused with freckles. After cessation of phototherapy sessions, small PUVA lentigoes usually remain on the skin for about 3-6 months, while large star-shaped lesions last up to 2 years.
Solar lentigo can appear after long and/or multiple courses of visiting a solarium - usually such pigmentation occurs in women prone to abuse of artificial ultraviolet radiation. Externally, these lesions are similar to PUVA lentigo and may be present in areas not naturally tanned (for example, in the armpit).
In some people, solar lentigo transforms from smooth spots into rough lesions, which can later develop into malignant tumors (for example, lentigo maligna). And although the likelihood of such an event is small, the problem is relevant and requires attention from both the patient himself and his attending physician.
A special type of benign neoplasm is macular nevus . It is both a lentigo and a melanocytic nevus, where multiple dark spots are located in the area of a large and lighter congenital or acquired spot ( Fig. 3 ). A spotted nevus can transform into melanoma, which is something to keep in mind.
Rice. 1. A lesion of solar lentigo on a woman’s cheek (www.medscape.com)
Rice. 2. Solar (senile) lentigo on aging skin of the hands (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/7-130-2.html
Rice . 3. Spotted nevus (Danish national service on dermato-venereology)
https://www.danderm-pdv.is.kkh.dk/atlas/7-150.html
Preventive measures (5 tips)
To minimize the risk of lentigo, you should adhere to certain preventive measures:
- before each exit to fresh air, lubricate the skin with cream with an SPF value of at least 30;
- people over 50 years old should try to spend less time in the sun and not visit the solarium;
- in the summer, always wear a hat and sunglasses;
- regularly undergo examination by a dermatologist to detect atypical moles or other pigmentation;
- immediately go to the doctor if dark spots of unknown etiology are detected on the body.
These spots usually appear due to constant sun exposure, so daily use of sunscreen is important for prevention.
Dermatological surgeon Mitchell Schwartz
If a stain on the skin does not cause discomfort, but is constantly subject to friction from clothing, then it is advisable to remove it.
Principles of treatment of solar lentigo
Before starting treatment for solar lentigo, you should perform a thorough diagnosis of pigmented formations and make sure that they are not malignant.
You can use creams with arbutin . This ingredient blocks the synthesis of pigment in melanocytes, which leads to blanching of solar lentigo lesions and evening out skin tone. Arbutin products usually contain several brightening agents, which makes them more effective.
For solar lentigo, creams with tretinoin and other retinoids . 33% trichloroacetic acid - to a greater extent in people with dark phototypes (IV-VI) according to Fitzpatrick. On the contrary, in patients with light phototypes (I–III), cryotherapy .
There is evidence of the use of a combination of 0.01% fluocinolone acetonide, 4% hydroquinone and 0.05% tretinoin as an adjuvant method in the fight against solar lentigo. The main treatment procedure in this case was cryotherapy. There is also evidence of using a product containing 2% mequinol and 0.01% tretinoin twice daily for 3 months. A pronounced result was achieved already in 2 months and lasted for at least 2 months after the end of therapy.
Among the new skin lightening products, Phalaenopsis Orchid Extract may be promising. So far, its capabilities have been tested in vitro on a cell line, but have shown good results.
Hardware cosmetology methods are successfully used to remove senile lentigo . The most common is IPL therapy, which uses high-intensity pulsed light to selectively destroy melanin. Another method is surface fractional photothermolysis, for example using a fractional Tm:fiber laser 1927 nm (Fraxel re:store DUAL). It is aimed at fractional destruction of the epidermis and all the structures that it contains. Taking into account the fact that lentigo lies in the epidermal layer, superficial fractional photothermolysis can significantly lighten the pigment spot and smooth its boundaries. As a result of several procedures using a non-ablative fractional laser, solar lentigo can be completely eliminated.
Note! Since foci of solar lentigo can transform into malignant tumors, and can also hide the appearance of melanoma, dynamic monitoring of the affected areas is necessary. The traditional method is regular examination of the skin by the patient himself and his attending physician. However, a more modern and reliable technique is the use of digital dermatoscopy and body mapping techniques, such as those presented by FotoFinder. Such systems make it possible to monitor the emergence of new tumors and monitor the dynamics of changes in existing ones.
Digital dermatoscopy itself allows the doctor to make a diagnosis based on the image. But it works even more effectively when coupled with a tumor image analysis program that uses the power of artificial intelligence. To date, the only such program is Moleanalyser pro.
Expert opinion
- Cosmetologist
- Surgeon
Anna Avaliani
practicing cosmetologist
I recommend paying attention to Q-Switch technologies (VersaPulse C laser or ConBio laser). Either of these two options should be better than IPL phototherapy, peels, or retinol. I would recommend starting with QS532 if the lentigines are superficial, or QS755 if they are deeper lesions. Usually 1-3 procedures are required.
Aisha Baron
plastic surgeon
Take a comprehensive approach to the problem.
Go to a dermatologist who will select the appropriate procedure. Indeed, laser technologies have proven themselves to be the best. Use creams recommended by a specialist. In addition, don't forget to protect your skin from the sun. Now it is more or less clear what lentigo is. But this pathology was considered only in relation to humans.
It turns out that this disease is common in dogs and cats. You can find out more about this on veterinary forums.
Summarizing all that has been said, the conclusion suggests itself that timely diagnosis of the disease is the key to successful treatment and a guarantee of safety from oncology.
Care
The lentigines themselves are benign,[4] but some may wish to be removed or treated for cosmetic purposes. In this case, they can be removed surgically,[4][5] or alleviated using topical depigmentation agents. Some common depigmentation agents, such as azelaic acid and kojic acid, do not appear to be effective in this case.[6] however, other agents may work well (4% hydroquinone,[7] topical 5% cysteamine,[8] topical 10% ascorbic acid[9]).
Causes
Medicine cannot yet say exactly why this disease occurs. But doctors identify certain factors that cause these spots to appear more often:
- Sunburn in childhood;
- Light hair and skin;
- Advanced age;
- Weakened immunity due to taking immunosuppressants;
- Human papillomavirus;
- Regular visits to the solarium;
- Increased sensitivity to ultraviolet radiation;
- Prolonged exposure to the sun;
- Hormonal changes;
- Pregnancy.