Composition of Terbinafine ointment
The main component is terbinafine hydrochloride. In one tube it is contained in the amount of 1g per 100g of composition. As additional substances, it contains rare cross-linked polyacrylic acid in the amount of 1.5 g, as well as 10 g of propylene glycol, 5 g of petroleum jelly, 0.4 g of sodium hydroxide. A large share of the volume is purified water - here it is 81g.
Terbinafine is available both as an ointment and as a gel or cream. The product for topical use is packaged in aluminum tubes, which are placed in cardboard packages, 1 piece each.
Components of Terbinafine
The instructions indicate the following ingredients of the medication:
- Tablets - presented with terbinafine hydrochloride, lactose monohydrate, potato starch, talc, aerosil, magnesium stearate, MCC;
- Ointment - terbinafine hydrochloride, carbomer, vaseline oil, polysorbate, sodium hydroxide, water, propylene glycol, methyl parahydroxybenzoate.
Terbinafine is produced not only in ointments and tablets, but also in cream and spray. The choice of the appropriate form to combat fungal infection is the responsibility of the attending physician. External forms are used for mild lesions, oral forms for systemic infection.
pharmachologic effect
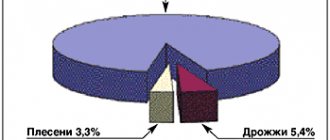
Terbinafine has a pronounced antifungal effect. The ointment is intended for topical use. It is effective in combating dermatophytes, varieties of molds and dimorphic fungi. When applying a small amount of the product, it is possible to achieve a fungicidal effect.
In relation to yeast fungi, Terbinafine can have both fungicidal and fungistatic effects. Its activity is mainly manifested in the treatment of skin lesions by representatives of the genus Candida albicans. The ointment affects biosynthesis processes during the early stage of sterol formation, namely, a deficiency of ergosterol is formed and a simultaneous increase in squalene content. This imbalance of chemical bonds leads to the death of fungal cells. The ointment is safe in relation to the cell membrane of the human body. It does not have any effect on the production of hormones, the functioning of internal organs and the effect of other medications. No more than 5% of the drug is absorbed into the bloodstream if a dense layer is applied. The systemic effect in this case is insignificant.
Contraindications to treatment
Terbinafine tablets are not used:
- for acute or chronic liver pathologies;
- renal failure;
- allergies to lactose, lactase deficiency;
- intolerance to the component composition;
- body weight less than 20 kg or under 3 years of age;
- breastfeeding.
Particular care is needed when carrying out therapeutic measures for people:
- with chronic renal failure, neoplasms;
- alcohol addiction;
- problems with the functionality of the hematopoietic system;
- diseases of the endocrine department;
- psoriasis, narrowing of the lumens in the blood vessels of the legs, etc.
Therapy is carried out with monitoring of the functioning of the kidneys and liver. Terbinafine is discontinued if:
- discomfort in the abdomen, jaundice;
- weakness, nausea;
- changes in the color of urine to dark, and stool to a light shade.
Local forms of the medication are not used for allergies or hypersensitivity to components.
The list of relative contraindications to the use of Terbinafine is presented:
- insufficient performance of the liver and kidneys;
- alcohol addiction;
- diseases of the endocrine department;
- tumor-like processes.
The drug is not recommended for patients under 12 years of age.
Indications for use of Terbinafine
The main indication for prescribing Terbinafine ointment is damage to the skin by a fungal infection. First of all, these are mycoses of the skin of the foot. In addition to fungus on the legs, the remedy treats fungal infections of the groin area, which experts call tinea cruris. In addition, smooth areas of the body infected with fungus can also be treated with ointment.
Diaper rash, in the absence of timely and adequate skin care, can become a breeding ground for the proliferation of pathogenic microorganisms. Fungi of the genus Candida especially love this humid environment. This is a yeast type that quickly spreads in folds, on the crooks of the arms and fingers, as well as on hairy areas of the body (head, armpits, groin). Treatment with Terbinafine ointment makes it possible to get rid of this pathogen.
Signs of lichen versicolor are also a reason to prescribe Terbinafine. Mycosis is a common skin disease that affects not only adults, but also children. The first signs of the spread of a fungal infection are the following markers:
- Redness on the skin, usually with clearly defined boundaries of the source of infection. The borders may be uneven and irregular in shape.
- The edges of the lesion often have a whitish tint, especially for lesions of fungi of the genus Candida.
- The inflamed area is itchy.
- The surface of the skin of the affected area peels off.
- At the site of inflammation, vesicles with serous contents appear. Violation of the surface of the bubbles leads to the separation of liquid and the formation of crusts.
Fungal infections are transmitted by contact and airborne droplets. In addition, failure to comply with hygiene standards provokes the spread of mycoses. Therefore, when visiting baths, saunas, public showers and other public places with high humidity, it is necessary to avoid contact of bare feet with the floor.
Mycosis can also appear as a result of wearing low-quality shoes made from non-breathable materials. It is also not recommended to wear synthetic socks in closed shoes.
Overdose symptoms
Accidental use of large quantities of Terbinafine tablets may cause:
- dermatological rash, cephalalgia;
- frequent urination;
- attacks of vomiting with dizziness;
- discomfort from the gastrointestinal tract.
Therapy includes gastric lavage with activated charcoal. In difficult cases, symptomatic treatment is prescribed.
There is no information in the annotation about cases of ointment overdose. These adverse reactions occur when an external agent is accidentally taken orally.
Instructions
The ointment is used strictly externally. Recommended for use by adults and children over 12 years of age. Before applying the product, it is necessary to remove all contaminants from the surface of the skin and dry it. A small amount of cream is rubbed into the lesion, covering a small area beyond the edges of the inflammation. Repeat the procedure in the morning and evening.
The course of treatment depends on the degree of damage and the type of fungal infection:
- smooth skin, including areas on the back, abdomen and lower legs, require 1 week of treatment;
- foot fungus goes away within 8-9 days of using Terbinafine ointment;
- treatment of candidiasis can last up to 2 weeks;
- It also takes 10 to 14 days to get rid of tinea versicolor.
If the use of the ointment does not give the desired effect over time, or during treatment there is a clear progression of the disease, accompanied by growth of the affected area, it is necessary to contact a specialist to prescribe systemic antifungal agents or to change the treatment regimen with local agents.
Terbinafine
The drug is generally well tolerated. Side effects are usually mild or moderate and transient.
When assessing the frequency of side effects, the following gradations were used: “very often” (≥ 1/10), “often” (≥1/100 <1/10), “infrequently” (≥1/1000 <1/100), “ rarely" (≥1/10000 <1/1000), "very rarely" (<1/10000), including isolated reports.
Disorders of the hematopoietic system: infrequently - anemia, very rarely - neutropenia, agranulocytosis, thrombocytopenia, pancytopenia.
Immune system disorders: very rarely - anaphylactoid reactions (including angioedema), cutaneous and systemic lupus erythematosus (or their exacerbation).
Nervous system disorders: very often - headache; often - dizziness, disturbances in taste, up to their loss (usually recovery occurs within a few weeks after stopping treatment); infrequently - paresthesia, hypoesthesia. There are isolated reports of cases of long-term disturbances in taste. In some cases, while taking the drug, exhaustion was noted.
Mental disorders: often - depression; infrequently - anxiety.
Visual disturbances: infrequently - visual disturbances.
Hearing and labyrinthine disorders: uncommon - tinnitus.
Disorders of the liver and biliary tract: rarely - hepatobiliary dysfunction (mainly of cholestatic nature), incl. liver failure, including very rare cases of severe liver failure (some fatal or requiring liver transplantation; in most cases where liver failure developed, the patients had serious underlying systemic diseases and the causal relationship of liver failure to terbinafine was questionable), hepatitis, jaundice, cholestasis, increased activity of liver enzymes.
Disorders of the digestive system: very often - bloating, loss of appetite, dyspepsia, nausea, mild abdominal pain, diarrhea.
Disorders of the skin and subcutaneous tissues: very often - rash, urticaria, infrequently - photosensitivity reactions; very rarely - Stevens-Johnson syndrome, toxic epidermal necrolysis, acute generalized exanthematous pustulosis, erythema multiforme, toxic skin rash, exfoliative dermatitis, bullous dermatitis, psoriasis-like skin rashes or exacerbations of psoriasis, alopecia.
Musculoskeletal and connective tissue disorders: very often - arthralgia, myalgia.
General disorders: often - feeling of fatigue; infrequently - increased body temperature.
Laboratory and instrumental data: infrequently - loss of body weight (secondary to a disturbance in the sense of taste).
Based on spontaneous reports received during the post-registration period and literature data, the following adverse events were identified, the frequency of which, due to the inaccurate number of patients, cannot be established:
Immune system disorders: anaphylactic reactions, serum sickness-like syndrome.
Visual disturbances: blurred vision, decreased visual acuity.
Skin and subcutaneous tissue disorders: drug rash with eosinophilia and systemic symptoms (rash, swelling, fever, and swollen lymph nodes).
Hearing and labyrinthine disorders: hearing loss, hearing impairment.
Vascular disorders: vasculitis.
Nervous system disorders: loss of smell, including for a long period of time, decreased sense of smell.
Digestive system disorders: pancreatitis.
Disorder of the musculoskeletal and connective tissue side: rhabdomyolysis.
General disorders: influenza-like syndrome.
Blood and lymphatic system disorders: anemia.
Laboratory and instrumental data: increased activity of creatine phosphokinase in blood plasma.
If any of the side effects indicated in the instructions get worse, or you notice any other side effects not listed in the instructions, tell your doctor.
Terbinafine cream - instructions
Unlike ointment, cream does not penetrate so deeply into the skin. Part of the applied layer is often rubbed off on clothing and surfaces with which the affected area of the body comes into contact. Therefore, the use of cream can be increased up to 3 times a day.
The advantage of the cream is its effectiveness even on moderately wet surfaces, which is especially important for fungal skin infections. If it is not possible to dry the surface due to the constant release of liquid, it is better to buy a cream, since the ointment in this case will be ineffective.
Terbinafine in the treatment of onychomycosis in patients with somatic diseases
Onychomycosis of the feet and hands is one of the most common diseases. In the UK, 2.7% of the population suffers from onychomycosis: this figure accounts for 15–40% of all nail diseases and 10–30% of all dermatophytoses. 13% of men and 4.3% of women in Finland are diagnosed with onychomycosis [1, 2]. In Russia, 30–70% of people have onychomycosis pathogens isolated from the skin of their feet.
The source of onychomycosis pathogens is always a person who is sick or has recovered from this disease. And infection can occur in two ways: through direct contact with a patient (less often) or through the use of objects contaminated with pathogenic fungi (more often). Fungal cells are stable in the external environment: they can survive for a long time in socks and shoes, carpets, cracks in the floors of residential premises and public institutions (hotels, baths, showers, swimming pools, gyms), where sanitary and hygienic conditions are not observed. Pathogens of onychomycosis can persist even on particularly popular, heavily visited beaches. The high incidence of onychomycosis is explained not only by the widespread distribution of its pathogens and the contagiousness of the disease, but also by the low effectiveness of its treatment. Before the introduction of modern systemic antifungal drugs into medical practice, the possibility of obtaining a lasting therapeutic effect for onychomycosis did not exceed 40–50%.
Among the causative agents of foot mycoses, the most important are dermatophytes: Trichophyton rubrum (up to 80%) and Trichophyton mentagrophites. Onychomycosis, caused by dermatophytes, is a contagious disease. Its pathogens develop on keratinizing epithelium. In conditions of human immunodeficiency, they acquire parasitic properties and begin to feed not only on obsolete skin elements, but also on living tissues, causing an inflammatory reaction.
The threat of developing fungal infections of the feet increases with injuries, poor circulation in the lower extremities, and excessive sweating of the skin of the feet and hands. The state of the nervous and endocrine systems, type of metabolism, and body weight also matter. Women suffer from onychomycosis more often than men. Curvature of the fingers, deformation of the joints, abrasions, calluses lead to a change in the shape of the entire foot and a greater or lesser loss of its functions. The occurrence of an imbalance between the structure and function of the foot is accompanied by impaired blood circulation in it and a reduction in the supply of foot tissue with nutrients. This leads to a weakening of the protective functions of the skin of the foot.
The likelihood of nail disease increases with a combination of several risk factors, for example: increased function of the adrenal cortex, associated increase in body weight and sweat production, decreased immunity and contact with the source of the pathogen. Of the common diseases that most often make up the background of fungal nail diseases, the following should be indicated: Cushing’s disease or syndrome, diabetes mellitus, varicose veins of the lower extremities, thrombophlebitis, swelling in the legs of various origins, vitamin deficiencies. In recent years, one of the common causes of onychomycosis has become AIDS, which is generally characterized by fungal complications.
Treatment of onychomycosis
The use of local treatments for onychomycosis, even the most modern, makes it possible to obtain the desired result only with limited lesions of the nail plate. Cure of total nail damage is possible only by surgical removal of the nail plates or through the use of modern systemic agents. The choice of such products from a dermatologist and general practitioner is limited. The list includes only three names: itraconazole, fluconazole and terbinafine. Griseofulvin and ketoconazole, used in past years, are not currently used for the treatment of onychomycosis due to their low effectiveness and the risk of developing side effects and complications with long-term use. Only with the development of triazole derivatives and then allylamines was there a real breakthrough in the drug treatment of onychomycosis. The first such drug, itraconazole, was synthesized in 1980 [3].
In Russia, itraconazole in the form of orungal has been successfully used since 1996. And the first of the three listed drugs for systemic action in Russia was terbinafine, marketed under the name Lamisil [4].
The pharmacokinetics of terbinafine does not depend on the age, gender and other characteristics of the person. After oral administration, 40% of the drug is metabolized in the liver, then 90% binds to proteins and concentrates in tissues rich in proteins and keratin. The drug is easily absorbed in the small intestine, leaves the blood plasma in the next few hours and accumulates in keratin tissues, where it persists for weeks. Its fungistatic and fungicidal activity is realized by inhibiting squalene epoxidase, an enzyme system involved in the synthesis of ergosterol, which is responsible for the permeability of the fungal cell membrane. Impaired ergosterol synthesis leads to loss of cell cytoplasm. The cell loses its ability to reproduce and develop.
In 2000, a new terbinafine drug, exifin, was registered in Russia (Dr. Reddy,s Laboratories). When a new drug, an analogue of an existing one, appears, the question of its quality usually arises. There is an opinion that a new drug certainly has low therapeutic capabilities compared to the original drug and is capable of producing side effects that were not characteristic of the original drug.
In order to study the effectiveness of treatment and tolerability of exifin, we conducted an open, non-randomized clinical study of the results of its use in 54 patients with onychomycosis of the feet and hands caused by Tr. rubrum [8].
The condition for inclusion in the study group was the absence of treatment of patients with systemic antimycotic, hormonal, cytostatic or antibacterial drugs for a period of at least 4 weeks before the start of treatment with exifin. Our further studies were devoted to the peculiarities of the use and action of exifin in patients with underlying somatic pathology. A total of 27 such patients aged from 18 to 68 years received treatment with exifin, of which 15 were women, 12 were men.
The examination revealed the following background diseases: arterial hypertension - 5, diabetes mellitus type 1 - 6, diabetes mellitus type 2 - 8, bronchial asthma - 1, atherosclerosis of the aorta, coronary, cerebral vessels and great vessels of the extremities - 5, traumatic spondylitis with radicular syndrome and impaired motor function of the limbs - 1, Itsenko-Cushing syndrome - 1. Of particular interest were patients with diabetes mellitus, in whom carbohydrate metabolism disorders are accompanied by angiopathy of the peripheral vascular areas and polyneuropathy with impaired tissue trophism. Among patients with diabetes, every third person suffers from onychomycosis of the feet [9].
The duration of onychomycosis in the group ranged from 10 months to 30 years, the average duration was about 5 years. In all patients, the diagnosis of onychomycosis was verified by microscopic examination of scrapings from the nail plates in a 10% KOH solution and culture on Sabouraud's medium. Culture revealed the growth of the fungus Tr. in all patients. rubrum. Patients with other pathogens were not included in the study group.
The effectiveness of treatment was monitored once a month. Tolerability of the drug was monitored during the first 10 days of treatment. The treatment outcome was assessed after 3–4 months, and then after 8–9 months from the start of treatment.
Exifin was prescribed in tablets of 250 mg once a day. Treatment of onychomycosis of the feet was carried out for 80–112 days, depending on the severity of the disease. The given numbers are multiples of 16 - the number of tablets of the drug in one package. If necessary, exifin cream was additionally prescribed to the skin. The patient was advised to trim his nails as they grow and clean the affected part of the nail.
Recovery (good result) was confirmed by the restoration of the nail plates and the absence of the pathogen during microscopic examination of the material and growth in a nutrient medium. Incomplete restoration of the nail plates, detection of the pathogen by microscopy of scrapings in the absence of its growth on the nutrient medium made it possible to evaluate the result as satisfactory and was the basis for prolonging treatment. 3–4 months after the start of treatment with exifin, a clinical analysis of its results revealed a positive effect in most patients, but only after 8–9 months could the final result be assessed: during this time, natural regrowth (restoration) of the nail plates occurred in patients with a positive effect of treatment (25 patients out of 27). During mycological examination in the group of convalescents, the pathogen was not detected either microscopically or by cultural method.
The drug was well tolerated in all patients. Assessment of biochemical blood parameters during the course of therapy did not reveal negative dynamics. Thus, the present study, conducted on a limited number of patients, confirmed the high effectiveness of exifin in patients with onychomycosis of the feet caused by Tr. rubrum, against the background of somatic diseases with circulatory disorders in the extremities.
The research revealed the following conditions for the successful use of exifin in patients with diabetes mellitus and other underlying diseases:
- maximum compensation of impaired functions;
- study of the condition of the liver and kidneys (aminotransferases, bilirubin, creatinine) before and during treatment;
- readiness to extend the duration of treatment - up to 112 days or more;
- local therapy with exifin cream or other external antifungal drugs;
- means that increase microcirculation;
- vitamin therapy.
Based on the above, the following conclusions can be drawn.
- Exifin tablets in terms of effectiveness, harmlessness to the patient, and ease of use meet the requirements for modern drugs for the treatment of onychomycosis of the feet and hands.
- Exifin can be recommended by dermatologists and general practitioners for systemic treatment of onychomycosis caused by Tr. rubrum, in patients with underlying pathology accompanied by metabolic disorders and circulatory tissue disorders.
- In patients with diabetes mellitus and other underlying diseases, compared with patients without them, an increase in the duration of treatment for onychomycosis with exifin may be required.
- To optimize the results of treatment of onychomycosis with exifin, it is necessary to use vitamins and agents that improve the rheological properties of blood.
V. B. Antonov , Doctor of Medical Sciences, Professor of the Research Institute of Medical Mycology named after. P. N. Kashkina, SPbMAPO, St. Petersburg
Interaction with other drugs
Combination with foreign drugs provokes:
- influence on the clearance of drugs - Cyclosporine, oral contraceptives, Tolbutamide;
- increased concentration of histamine blockers in the blood;
- slowing down the excretion of Rifampicin;
- changes in the menstrual cycle - when combined with oral contraceptives.
Drug-induced liver damage occurs when taken with hepatotoxic drugs or ethanol.