Acanthosis nigricans (ICD-10 code - L 83) is a rather rare type of dermatosis. From this it is clear that this is a disease of a dermatological nature.
To date, its etiology has not yet been fully established. Externally, it makes itself felt by blackening and roughening of the skin in those places where it forms natural folds: the groin, armpits, neck.
The problem is not only aesthetics, it is much more serious. Presumably the disease is associated with oncology, which is a serious statement. So this article will be useful to everyone who cares about their health.
Acanthosis nigricans: probable causes of the disease
Although the reasons for the coarsening and darkening of individual areas on the skin are not yet precisely known, there are scientific assumptions in this regard.
Damage to acanthosis nigricans is possible as a result of the following provoking factors:
- Predisposition to this disease at the genetic level. More often, the disease is activated due to congenital anomalies leading to metabolic and mental disorders. There is a high probability of acanthosis in Miescher-Rood syndrome.
- Neoplasms of a malignant nature. Immune disruptions are observed in the body. In men, cancer most often affects the pancreas, prostate or stomach, in women - the appendages and mammary glands. Acanthosis can also be diagnosed in malignant tumors of other organs of the gastrointestinal tract and reproductive system.
- Disturbances in the functioning of the endocrine system, which is caused by hormonal and metabolic disruptions. These may be the following pathologies: obesity, insulin resistance, cellulite, Addison's and Cushing's diseases.
- Taking potent hormonal drugs and other pharmaceuticals without following the prescribed dosages (for example, nicotinic acid).
This disease occurs not only in humans, but also in dogs.
Family doctor Jenny Weiler
This disease affects people of any age group, but the reasons for each are generally different. Thus, in young people, the development of acanthosis nigricans is possible due to heredity and due to endocrine dysfunction, and in older people and the elderly - as a symptom of oncology.
Since this dermatological disease is directly related to insulin resistance, people with type 2 diabetes are more susceptible to it. But in children the opposite is true - acanthosis can cause diabetes in the future.
Any hyperpigmentation on the skin, even minor, should be taken as an alarming signal about hidden health problems.
Therefore, you should not postpone your visit to the clinic, where you should definitely undergo a full examination.
Diagnostics
It is very important to differentiate acanthosis nigricans associated with malignant neoplasms from diseases associated with benign conditions. Tumors in malignant acanthosis nigricans are usually very aggressive and spread quickly. Death often comes very quickly. If malignant acanthosis nigricans is suspected in a patient without a known internal cancer, it is essential to perform a thorough examination to identify malignancy and occult tumors. If the tumor can be successfully treated, the condition may be eliminated.
Other causes of acanthosis nigricans can be identified by screening for insulin resistance and diabetes.
General symptoms of the disease
With acanthosis nigricans in a person, the clinic will be as follows:
- compaction and peeling of individual areas of the epidermis;
- the appearance of hyperpigmentation (brown-black spots);
- formation of papillomas or fibromas (popularly such neoplasms are called warts).
Localization of acanthosis nigricans:
| Place | Photos of symptoms |
| In the armpits | |
| On the neck | |
| Under the knees | |
| On the elbows |
This disease also occurs in the groin, gluteal area, thighs, and near the mammary glands (in women). But not so often.
Even less commonly, signs of the disease may appear near the navel and on the face. In especially severe cases, damage to the mucous membranes, esophagus, rectum and vagina is noted.
First, in a sick person, individual areas of the epidermis turn yellow, which gradually become darker. Outwardly, it looks like banal pollution.
That's why many people try to wash it off. But, if you do not resort to appropriate treatment, the disease progresses. As a result, the skin becomes rough and constantly flakes, and pigmentation intensifies.
In the final stages, the skin becomes covered with small papillary-shaped compactions, sometimes also black. Their accumulation is quite large.
When the lesion affects the mucous components of pigmentation, no pigmentation is observed, but the formation of papillomas is likely.
The mucous membranes are covered with small villi and shallow grooves. If the disease affects the tongue, it becomes excessively wrinkled.
Family doctor Mohammed Ahmad
It is rare, but it happens when all these symptoms are accompanied by itching and tingling. The affected areas also lose hair.
It is important not to ignore any of these signs, since detecting this disease in the early stages makes treatment easier.
What are the forms of acanthosis (3 options)
Depending on the symptoms and severity, acanthosis nigricans comes in three types:
- Benign (juvenile).
- Malignant (parneoplastic).
- Pseudoacanthosis.
Malignant form
Acanthosis nigricans in its malignant form is more often diagnosed in adults. Usually the impetus for its development is a malignant tumor inside the body.
This is a kind of harbinger of cancer, sometimes notifying the appearance of a tumor several years in advance. According to statistics, this happens in 20%, in another 20% skin changes occur after, in the remaining 60% - against the background of progressive cancer.
At this stage of acanthosis nigricans, patients note the following changes in their general condition:
- increased fatigue;
- depression;
- desire to sleep;
- physical weakness;
- fast weight loss;
- loss of appetite.
It should be noted that these signs arise spontaneously and begin to progress intensively. The mucous membranes of the vagina and digestive tract are gradually captured.
On the hands (outside), papules (small warts) may form, sometimes merging into large plaques. They can be reddish in color or the same as the rest of the skin. Moreover, the dermis underneath becomes rough and compacted.
When the original source (tumor) is surgically removed, then all accompanying manifestations in the form of hyperpigmentation and papillomas are leveled out.
Plastic surgeon Michael Zenn
Benign form
A similar type of acanthosis nigricans occurs with congenital dysfunctions and can manifest itself in a child.
It differs from the previous version in the absence of pronounced symptoms, and most importantly, cancerous tumors.
Often, after growing up, the disease goes away on its own without any negative consequences for the body.
Pseudoacanthosis
This form of acanthosis nigricans suffers from obesity. The development of the disease occurs due to endocrine disruptions, which are not uncommon in women due to dysfunction of the appendages.
On the skin, where they form large folds, blurry “dirty” spots appear. At the same time, there are no papillomas. If you lose weight, then everything goes away.
Skin reactions to medications. How to recognize?
Part 2. Read the beginning of the article in No. 10, 2022.
Urticaria and angioedema
This is the only form of toxicerma caused by type I hypersensitivity with the participation of IgE. The reaction develops from a few seconds to a day after administration of the medicine. The most common cause is penicillin.
Latex most often causes contact urticaria and angioedema. Non-IgE-mediated skin manifestations are most often caused by acetylsalicylic acid and other NSAIDs, narcotic analgesics, and iodinated radiocontrast agents. Angiotensin-converting enzyme inhibitors can also cause edema by increasing the level of bradykinin in the blood [24]. Due to the fact that angioedema in response to the administration of radiocontrast drugs is caused by the involvement of mast cells [25] or by the release of factor XII from the vascular endothelium [26], scientists allow the possibility, if necessary, of repeated administration of these drugs after appropriate preparation (administration of systemic glucocorticosteroids and antihistamines before and after the administration of radiocontrast agents).
Toxicoderma similar to pemphigus vulgaris
The disease is mainly caused by drugs that have a thiol (sulfhydryl) group. Clinically and histologically, it is indistinguishable from autoimmune pemphigus vulgaris, but sometimes the development of rashes may be preceded by urticaria and eczematization of the skin. When studying direct immunofluorescence of skin biopsies, IgG fluorescence on the walls of keratinocytes of the basal layer is less pronounced than in autoimmune pemphigus. The disease has a good prognosis after discontinuation of the drug. The main drugs that can contribute to the reaction are acetylcholinesterase inhibitors, interleukin-2, nifedipine, penicillamine, penicillin, piroxicam, rifampicin [27].
Acanthosis nigricans
Along with malignant tumors and endocrinopathies, it can be caused by hormonal contraceptives, corticosteroids, nicotinamide, and testosterone. Drug-induced acanthosis nigricans has been associated with activation of insulin-like growth factor.
Lichen planus
There are many medications that can cause lichen planus (LP), or “lichenoid toxicoderma” (Table 6). The cause of the disease is unknown. It is interesting to note that hydroxychloroquine is one of the drugs that can cause LP on the skin, but at the same time it is the drug of choice in the treatment of erosive LP on the oral mucosa [28].
Psoriasis and medications
Psoriasis affects about 4% of the world's population. Therefore, special attention should be paid to medications that can cause or worsen psoriasis. These drugs are easy to remember if you use the English acronym “NAILS”: each letter represents a group of drugs that can worsen psoriasis. In particular, the letter N stands for NSAIDs (to a lesser extent these include acetylsalicylic acid, paracetamol and selective inhibitors of cyclooxygenase type 1); letter A - antimalarial drugs (chloroquine, hydroxychloroquine); letter I - interferon (any systemic interferon preparations such as Viferon, Genferon, etc.; interferonogens (Cycloferon, Tiloron, etc.), as well as nonspecific stimulators of T-lymphocytes aggravate psoriasis, since interferon is one of the important cytokines in the development of the disease); letter L—lithium carbonate; letter S - systemic corticosteroids. Although topical corticosteroids are an integral part of the treatment of psoriasis, the use of systemic forms of corticosteroids is not advisable. Of course, systemic corticosteroids can relieve exacerbation of psoriasis, but after their withdrawal the disease not only recurs, but also takes a more severe course. Another drug to consider is oral terbinafine. It is the drug of choice for onychomycosis caused by trichophyton red. Fungal nail infections are common in patients with psoriasis. Because terbinafine may worsen psoriasis, it is better to use other medications for these patients.
Granulomatous interstitial reaction (sarcoidosis-like rash)
Granulomatous interstitial reaction (rash similar to sarcoidosis) is rare, but many drugs can cause it (Table 4).
Hemorrhagic rashes
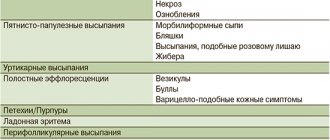
Hemorrhagic rashes caused by drugs are quite varied.
Leukocytoclastic vasculitis
If such vasculitis is caused by a drug, then clinically it corresponds to Henoch-Schönlein purpura. Occurs in 10% of cases among other causes of vasculitis with damage to small vessels. The disease occurs 1–3 weeks after the start of drug administration, but if the same drug is re-prescribed, it occurs within less than three days from the start of treatment [29].
Antibody-dependent thrombocytopenia
Antibody-dependent thrombocytopenia is manifested by increased bleeding, multiple petechiae and ecchymoses (non-palpable purpura). The cause may be heparin, minocycline, penicillin, sulfonamides, terbinafine, itraconazole, thiazide diuretics, cephalosporins, etanercept [28].
Thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura (TTP) is a serious disease accompanied by thrombocytopenia and multiple thromboses affecting all organs, especially the kidneys and central nervous system. The development of hemolytic uremic syndrome is possible. Tissue necrosis occurs due to arterial embolization.
Medicines that contribute to the development of TTP: mitomycin, cyclosporine A, cisplatin, bleomycin, quinine, antihyperlipidemic drugs, clopidogrel, tacrolimus.
Warfarin necrosis
Warfarin necrosis is caused by congenital deficiency of protein C and/or S. It develops 2–5 days after the start of treatment.
Heparin necrosis
Heparin necrosis is a rare drug-induced complication. Represents type III hypersensitivity, involving platelet factor 4, antibodies to heparin and platelets. Develops on average one week after the start of heparin treatment.
Iatrogenic calciphylaxis
Calciphylaxis occurs suddenly and develops rapidly. Early lesions of calciphylaxis appear as livedo reticularis or erythematous papules, plaques, or nodules. Subsequently, stellate purpura develops with central skin necrosis. Less commonly, you can see hemorrhagic blisters or individual subcutaneous erythematous nodes resembling erythema nodosum. The rash on palpation is very dense. Lesions may be proximal or distal. Proximal location occurs in 44–68% of patients, developing predominantly on the thighs, buttocks and lower abdomen. This location of lesions may be accompanied by visceral lesions and, accordingly, have a high incidence of death, in contrast to distal skin lesions. Ulceration is considered a late sign and is associated with higher mortality.
Occurs with intravenous administration of calcium preparations, more often in patients with hypercalcemia. Hypercalcemia is typical for patients with renal failure, systemic collagen diseases, certain malignant tumors (for example, small cell lung cancer), and hyperparathyroidism [28].
Calcification of the skin
A milder form of skin lesions, manifested by single papules and nodules, is called calcification of the skin.
Erythema nodosum
Erythema nodosum is a vasculitis of the deep veins of the lower extremities and is more common in women. In such cases, you should immediately clarify whether she is taking hormonal contraceptives or hormone replacement therapy. These drugs are quite often the cause of the development of erythema nodosum. Other drugs that can cause this disease: iodide, bromide, sulfonamides, echinacea.
Acneiform toxicoderma
Acneiform toxicoderma is clinically a papulopustular rash, very similar to acne vulgaris. Unlike acne vulgaris, this disease is characterized by damage to patients of any age group, sudden onset, localization mainly on the torso and less often on the face, absence of comedones, regression of rashes when the corresponding medication is discontinued [30]. This form of toxicoderma can be caused by anticonvulsants, tyrosine kinase inhibitors (in particular, imatinib mesylate), iodine, bromides, corticosteroids, testosterone, danazol, isoniazid, actinomycin D, cyclosporine, and especially epidermal growth factor receptor inhibitors (EGFR). Moreover, it is characteristic that the development of acne during treatment with antitumor drugs from the IEPF group is an indicator of their effectiveness. Oncologists note that there is a clear regression of the tumor. But sometimes the severity of acne is so pronounced that it forces you to stop taking the drug and treat the drug-induced complication itself.
Oral diseases as a manifestation of a reaction to medications
It should be remembered that there are dose-dependent side effects of drugs that are used when applied directly to the mucous membranes. Lichenoid eruptions, MEE, SSD, LS and pemphigus vulgaris, caused by drugs and also manifested by damage to the mucous membrane, were mentioned above.
Erosion and ulceration of mucous membranes
Unlike aphthous stomatitis, such reactions usually develop in patients of an older age group and are not prone to recurrence after discontinuation of the corresponding medication [31]. Mucosal erosions can be caused by sulfonamides, barbiturates, beta blockers, NSAIDs, phenolphthalein, dapsone, salicylates and tetracycline.
Hyperpigmentation of mucous membranes
Hyperpigmentation of the mucous membranes is possible when taking doxycycline, clofazimine, hormonal contraceptives (they stimulate melanogenesis), amiodarone, and antimalarial drugs.
Gingival hyperplasia
Gingival hyperplasia can be caused by cyclosporine, angiotensin-converting enzyme inhibitors (especially when the patient receives these two medications together), anticonvulsants, and large doses of progesterone. Gum hypertrophy is usually dense, appears several months after the start of treatment, is not accompanied by pain and is most pronounced between the teeth. Sometimes patients experience erythema and soreness in the oral cavity [32].
Conclusion
Thus, reactions to medications with skin manifestations are extremely varied. In the presence of dermatosis, the question of drug therapy, regardless of whether it is related to this dermatosis, should be mandatory when collecting anamnesis. It is the anamnesis that is decisive in recognizing the “culprit” drug. In this case, it should be clarified when the patient began taking these medications. If the period from the start of taking the medicine is no more than two months from the moment of the rash, it is worth clarifying whether there is a connection between the skin rash and taking the medicine. If a patient takes a medicine for six months or more, it is almost impossible that the skin rash is caused by this drug. But there are exceptions: for example, angioedema due to angiotensin-converting enzyme inhibitors can develop 10 years after the start of treatment.
If there is an assumption about the possible role of the drug, an appropriate examination should be carried out. In a real situation this is not always possible.
And then the next important question for the doctor: is it possible to cancel or replace this medicine? In some cases (for example, during chemotherapy for a tumor), the doctor cannot stop the drug, and the doctor’s task is to prescribe treatment in order to alleviate the side effects of the drug or find a replacement for this drug. Regression of rashes after discontinuation of the drug also helps to find the cause of the disease.
Literature
- Gerogianni K., Tsezou A., Dimas K. Drug-Induced Skin Adverse Reactions: The Role of Pharmacogenomics in Their Prevention // Mol Diagn Ther. 2022, Jun; 22(3):297–314.
- C. de la Torre, Oh H. J. Suh. Advances in the diagnosis of drug eruptions // Actas Dermosifiliogr. 2013, Nov; 104(9):782–788.
- James WD, Berger TG, Elston DM Andrews Diseases of the Skin. Clinical Dermatology // Saunders Elsevier. 2006, 10th edit.: 123.
- Schneider JA, Cohen PR Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A Concise Review with a Comprehensive Summary of Therapeutic Interventions Emphasizing Supportive Measures // Adv Ther. 2017; 34(6):1235–1244.
- Renn CN, Straff W., Dorfmüller A., Al-Masaoudi T., Merk HF, Sachs B. Amoxicillin-induced Exanthema in Young Adults with Infectious Mononucleosis: Demonstration of Drug-specific Lymphocyte Reactivity // Br J Dermatol. 2002, Dec; 147(6):1166–1170.
- Ramirez A., Perez-Perez L., Fernandez-Redondo V., Toribio J. Photoallergic Dermatitis Induced by Diltiazem // Contact Dermatitis. 2007: 56: 118–119.
- Weyers W., Metze D. Histopathology of Drug Eruptions - General Criteria, Common Patterns, and Differential Diagnosis // Dermatol Pract Concept. 2011; 1(1):9:33–47.
- Ackerman AB, Chongchitnant N, Sanchez J et al. Histologic Diagnosis of Inflammatory Skin Diseases. 2nd ed. Baltimore: Williams & Wilkins, 1997: 317.
- Majdy N., Weyers W., Metze D. Histopathologic Features of Exanthematous Drug Eruptions of the Macular and Papular Type // Am J Dermatopathol. 2011; 33(7):695–704.
- Busam KJ Dermatopathology E-Book: A Volume in the Series: Foundations in Diagnostic Pathology (Expert Consult - Online), 2nd ed, 2016. Elsevier/Saunders. Chapter 14. Hematopoetic Neoplasms: 603.
- Goldberg I., Hanson M., Chodick G., Shirazi I., Brenner S. In Vitro Release of Interferon-Gamma from Peripheral Blood Lymphocytes in Cutaneous Adverse Drug Reactions // Clin Dev Immunol. 2012: 687532.
- Barbaud A. Drug Patch Testing in Systemic Cutaneous Drug Allergy // Toxicology. 2005; 209(2):209–216.
- Schulz JT, Sheridan RL, Ryan CM, MacKool B., Tompkins RG A 10-Year Experience with Toxic Epidermal Necrolysis // J Burn Care Rehabil. 2000; 21 (3): 199–204.
- Bastuji-Garin S., Fouchard N., Bertocchi M., Roujeau JC, Revuz J., Wolkenstein P. SCORTEN: a Severity-of-illness Score for Toxic Epidermal Necrolysis // J. Invest. Dermatol. 2000; 115:149–153.
- Ruble J., Matsuo F. Anticonvulsant-Induced Cutaneous Reactions. Incidence, Mechanisms and Management // CNS Drugs. 1999, Sep; 12 (3): 215–236.
- Walsh SA, Creamer D. Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS): a Clinical Update and Review of Current Thinking // Clinical and Experimental Dermatology. 36:6–11.
- Sheikh JS, Farah S, Mohd A. Drug Reaction with Eosinophilia and Systemic Symptoms: Manifestations, Treatment, and Outcome in 17 Patients. Int J Dermatol. 2015, 54: 537–542.
- Shiohara T., Inaoka M., Kano Y. Drug-induced Hypersensitivity Syndrome (DIHS): A Reaction Induced by a Complex Interplay among Herpesviruses and Antiviral and Antidrug Immune Responses // Allergol. Int. 2006; 55:1–8.
- Koumantaki-Mathioudaki E., Papadavid E., Katsambas A. Generalized pustular drug eruptions // JADV. 1999, 12: 196–197.
- Ardeshna KP, Rohatgi S, Jerajani HR Fixed Drug Eruption to Cetirizine: An Unusual Villain // Indian Dermatol Online J. 2018, Jan-Feb; 9 (1): 55–57.
- Mi-Yeong K., Eun-Jung J., Yoon-Seok C., Sang-Heon C., Kyung-Up M., Sae-Hoon K. A Case of Levocetirizine-induced Fixed Drug Eruption and Cross-reaction with Piperazine Derivatives // Asia Pac Allergy. 2013, Oct; 3 (4): 281–284.
- Drucker AM, Rosen CF Drug-Induced Photosensitivity. Culprit Drugs, Management and Prevention // Drug Safety. 2011; 34(10):821–837.
- Sehgal VN, Jain S., Bhattacharya SN Cutaneous drug reactions // JEADV. 1993, 2: 281–295.
- Frigas E., Nzeako UC Angioedema. Pathogenesis, differential diagnosis, and treatment // Clin Rev Allergy Immunol. 2002; 23(2):217–231.
- Lasser EC Chasing Contrast Molecules: A 45 Year Quixotic Quest // Acad Radiol. 2004; 11: 1190–1196.
- Bush WH, Segal AJ Recognition and Treatment of Acute Contrast Reactions // Appl Radiol December. 2009: 21.16–21.
- Brenner S., Bialy-Golan A., Ruocco V. Drug-induced Pemphigus // Clin Dermatol. 1998; 6 (3): 393–397.
- Khaliulin Yu. G., Urbansky A. S. Modern approaches to the diagnosis and drug therapy of dermatoses. A textbook for the system of postgraduate and additional professional education of doctors. Kemerovo: KemGMA, 2011. 165 p.
- Valleyrie-Allanore L., Sassolas B., Roujeau J.-C. Drug-Induced Skin, Nail and Hair Disorders // Drug Safety. 2007; 30 (11): 1011–1030.
- Virendra NS, Sanjiv J., Sambit NB Cutaneous drug reactions // JEADV. 1993, 2: 281–295.
- Femiano F., Lanza A., Buonaiuto C. et al. Oral Manifestations of Adverse Drug Reactions: Guidelines // JEADV. 2008, 22: 681–691.
- Tack DA, Rogers RS Oral Drug Reactions // Dermatologic Therapy 2002, 15: 236–250.
- Moore DE Drug-Induced Cutaneous Photosensitivity. Incidence, Mechanism, Prevention and Management // Drug Safety. 2002; 25 (5), p. 356.
Yu. G. Khaliulin1, Candidate of Medical Sciences D. Sh. Macharadze, Doctor of Medical Sciences, Professor
Federal State Autonomous Educational Institution of Higher Education RUDN University, Moscow
1 Contact information
Skin reactions to medications. How to recognize? (Part 2) / Yu. G. Khaliulin, D. Sh. Macharadze For citation: Attending physician No. 11/2018; Issue page numbers: 79-83 Tags: skin, allergic reactions, hypersensitivity
How can a disease be detected?
Before treating acanthosis nigricans, it must be accurately diagnosed. To do this, contact a specialist in skin problems (dermatologist).
Otherwise, you can confuse this disease with another due to the similarity of some symptoms, thereby harming your health with inappropriate therapy.
The final diagnosis is made based on histological analysis (histology) of a tissue sample (biopsy) taken from the affected area.
In the case of acanthosis nigricans, it is found:
- Hyperkeratosis.
- Excess pigment.
- Acanthosis to a small extent.
The stage of the lesion is determined depending on a number of factors: the onset of the disease, the age of the patient and his general condition, the severity of symptoms.
If cancer is suspected, they are sent to consult an oncologist. He gives directions for a comprehensive examination to detect a malignant tumor. You will also need to visit an endocrinologist and a number of other doctors.
Is it possible to recover and how?
People often wonder what to apply to the affected area. But you should not self-medicate, as the problem should be approached comprehensively.
Treatment for acanthosis nigricans occurs exclusively in a dispensary under the supervision of a doctor. An integrated approach is used here, since it is necessary to simultaneously eliminate the symptoms and the immediate cause of the disease.
In the case of juvenile acanthosis, patients are prescribed the following therapy:
- preparations with a general strengthening spectrum of effects: vitamin and mineral compounds, ginseng and echinacea;
- ointments with anti-inflammatory and antiseptic effects;
- nourishing creams;
- baths with the addition of potassium permanganate;
- zinc preparations;
- biological products: lactobacillin, bifidumbacterin and others;
- cytostatics (for severe disease);
- hormones (for endocrine disorders);
- neurotropic drugs and antibiotics (if indicated).
If the development of acanthosis is caused by excess weight, then an appropriate diet is prescribed. It is important to reduce carbohydrate-containing foods in your diet. The frequency of meals should be increased, but the portion size should be reduced.
Such patients must adhere to personal hygiene.
Dermatologist Jason Emer
In a situation where the cause of acanthosis is the uncontrolled use of certain medications, they are discontinued and replaced with safe ones with a similar effect. Sometimes, reducing the dosage is enough.
When the skin becomes overgrown with papillomas on a large scale, surgical intervention to remove them is inevitable.
Usually the method of cryodestruction or electrocoagulation is used (selected individually in each case).
The fight against malignant acanthosis is primarily aimed at getting rid of the tumor. Chemotherapy (if inoperable) or radiotherapy is usually prescribed.
If the cancer is successfully removed, all external signs will disappear on their own. Otherwise, they appear again after a while.
Treatment
In many situations, treatment of the underlying condition can restore normal skin pigmentation. Management of the benign form associated with obesity and insulin resistance conditions is based on reducing insulin levels in the circulation; Often a simple diet can significantly reverse skin damage.
Other underlying clinical conditions should be treated appropriately (as, for example, in the case of thyroid pathologies or adrenal disorders).
If the condition is caused by medications, your doctor may consider changing or changing your prescription for the medications that are causing the side effect.
Once the underlying medical condition has been diagnostically confirmed to improve the appearance of the skin, or if the lesions become itchy or irritating, a doctor may prescribe a topical cream or lotion.
Treatment for acanthosis nigricans includes the following:
- losing weight , changing eating habits and practicing regular exercise;
- application of preparations containing alpha hydroxy acids , such as glycolic or lactic acid;
- lotions containing salicylic acid ;
- creams containing urea (often recommended in concentrations of 20%);
- cortisone cream (if areas are itchy);
- retinoids , such as tretinoin (Retin-A), tazarotene or adapalene, to whiten affected areas (they mainly perform an exfoliating action, renewing the more superficial layers of the dermis);
- antibacterial soaps or topical antibiotics to reduce itching and discomfort.
None of these treatments are specifically designed to treat acanthosis sufferers, but they can all help alleviate the symptoms of the disorder.
Treatment for most resistant cases of acanthosis nigricans may include:
- fish oil included in the diet and taking nutritional supplements;
- Isotretinoin , a potent drug, is commonly used in the treatment of scars and acne.
Some procedures for aesthetic treatment of acanthosis nigricans include:
- dermabrasion , a mechanical, controlled surgical scraping of the skin that can help reduce the consistency of some affected areas;
- laser therapy , which reduces the thickness of the skin (destroys the most superficial layers).
What is the prognosis if affected by this disease?
It is impossible to make an unambiguous prediction about a person’s condition after a full course of treatment. Whether he will fully recover or not depends on the type of pathology:
- In a benign form, if the primary source is identified in time and managed to eliminate it, then the symptoms may disappear completely or begin to regress intensively. If it manifests itself in adolescence, then after puberty the disease disappears completely.
- In the case of a malignant form, the scenario is often unfavorable due to the rapid metastasis of the tumor. Even with high-quality treatment, the patient is given no more than 2 years of life.
- In the case of pseudoacanthosis, most patients recover after returning their weight to normal.
Childhood and juvenile acanthosis is mostly benign and does not have negative consequences.
Plastic surgeon Daniel Barrett
But in middle-aged and elderly patients there is a high probability of this type of dermatosis developing into seborrhea and fungal infections. Especially if the form is malignant.
At the first signs of acanthosis nigricans, you should immediately consult a dermatologist. It should be remembered that this type of dermatosis can signal more serious malfunctions in the body.
Signs and symptoms
Skin changes are the only signs of acanthosis nigricans. Skin changes tend to develop slowly, sometimes over several months or years. If symptoms appear suddenly, you should consult a dermatologist immediately, as the lesions can be a danger signal for very serious conditions.
At the skin level, the following symptoms can be noted:
- dark spots, which can vary in color from gray to brown or black, are located near the folds of the body (see photo above);
- the lesions appear as “velvety” thickenings (dry and rough skin) compared to the surrounding skin;
- dark brown skin may form small ridges (papillomatosis);
- the affected area may also be aching or itchy.
The body folds most commonly affected by an attack of acanthosis include:
- sides and back of the neck;
- armpits;
- groin.
Less commonly, skin lesions of acanthosis nigricans may also affect the following areas:
- face (front);
- inner thighs;
- elbows;
- knees;
- breast;
- navel or belly.
Very rarely, acanthosis nigricans can develop from:
- nipples;
- palms of hands;
- leg;
- centuries;
- lips;
- oral cavity.
Prevention
The best way to prevent acanthosis nigricans is to keep yourself in good physical shape and adopt a healthy lifestyle.
You should also adhere to the following rules:
- periodically visit a dermatologist for a routine examination and blood donation;
- do not resort to self-medication;
- at the slightest suspicion of problems with the endocrine system, contact the appropriate specialist;
- monitor blood sugar levels;
- do not take medications without medical prescription.
Risk factors
Acanthosis nigricans can affect people of any age (including children) and all ethnic groups. However, it is more common in adults and people with darker skin, such as Native Americans, Hispanics and some African populations. Men and women suffer equally.
People most susceptible to developing acanthosis nigricans are:
- people who are overweight or obese;
- subjects with endocrine or metabolic changes;
- patients who regularly take certain medications (eg, oral contraceptives, systemic corticosteroids, etc.);
- subjects who have undergone kidney transplantation;
- people with a malignant tumor on an internal organ (a very rare cause of acanthosis nigricans, especially malignant ones).
Expert opinion
- Cosmetologist
- Surgeon
Anna Avaliani
practicing cosmetologist
Acanthosis nigricans is accompanied by hyperketarosis and hyperpigmentation (skin thickness increases and darkens). Darkening is often observed in the fold area. The area most affected is the armpits and neck.
Aisha Baron
plastic surgeon
Most often, this problem appears in people with extra pounds, polycystic ovary syndrome, and those who have been diagnosed with hyperinsulinemia.
There is no special treatment for this pathology. Therapy is mainly aimed at combating the cause (the underlying disease). As a result, the skin is restored and pigmentation disappears. Summarizing all of the above, you can understand how dangerous this disease is. If you start treatment in the initial stages of development, then there will be no trace of the disease.
Otherwise, irreversible consequences for the body are possible, including death from cancer. To gather more information about acanthosis nigricans, it is recommended to read reviews on the Internet and visit online forums on this topic.
Possible complications
The severity of complications depends on the type of pathology. In case of false or benign genodermatosis, after treatment of the underlying disease, a decrease in the intensity of pigmentation is observed. In this case, complete restoration of the skin is possible. In this case, acanthosis does not cause complications.
Possible complications
When diagnosing a malignant type of pathology or its chronic form, fungal infections, psoriasis or seborrheic rashes may appear. Also, this type of genodermatosis can lead to the death of the patient from metastases of cancer tumors.
Skin roughness and dark discoloration often indicate the development of acanthosis nigricans. Photos of people with this pathology also show papillomatous rashes and a pronounced skin pattern. If such changes in the epidermis are detected, you should immediately undergo an examination by a dermatologist and oncologist. Self-medication in this situation is strictly prohibited.