Acne is a serious problem, but it can and should be dealt with. Modern medicine has a sufficient arsenal of means for a comprehensive, systemic elimination of both the result (acne of varying severity) and many causes and factors that provoke the course and development of the disease.
Undoubtedly, the first important step is to contact a specialist - try to avoid self-treatment of acne (pimples, acne), which may not only not bring the desired result, but also aggravate the situation. In particular, it is strongly recommended not to open, squeeze or otherwise remove pimples and pustules - this leads to the formation of significant scars and also contributes to the additional spread of infection. It is a professional dermatologist who will help you find the optimal way to combat acne and organize effective treatment.
It is necessary to take into account that in any case, treatment of acne and post-acne will require considerable patience and careful adherence to medical prescriptions over a long period (several months). In addition, you need to mentally prepare for certain difficulties - some stages of therapy may be accompanied by a slight deterioration in the condition of the skin.
Complex treatment of acne disease involves solving a number of diverse problems:
- Implementation of effective prevention designed to prevent the appearance of new manifestations of acne (comedones, papules, pustules, etc.); this is ensured through a set of measures for the general health of the patient’s body, as well as careful care of problem areas of the skin using special products, and compliance with general hygiene requirements.
- Elimination of existing formations; The removal of comedones is usually carried out in specialized beauty salons, where comedo extractors are used for these purposes, as well as a wide range of anti-acne procedures (photo-, light therapy).
- Reducing the level of sebum secretion from the corresponding glands of the skin; to ensure a clinically significant healing effect, it is necessary to reduce the level of secretion by at least 30%; For such adjustment, various medications are used that affect the patient’s hormonal levels (estrogens, antiandrogens).
- Localization and subsequent elimination of foci of skin inflammation; This stage involves the comprehensive use of antibacterial drugs for external and internal use.
- Minimizing the visibility of the results and consequences of acne, primarily scars; The main tool is cosmetic procedures such as cryotherapy, laser therapy, dermabrasion, etc.
As a rule, modern acne treatment, which provides an integrated approach to the problem, demonstrates the greatest effectiveness:
- combined use of drugs and medications that have a systemic effect on the body as a whole;
- the use of drugs that influence the maximum number of factors contributing to the development and aggravation of acne (including hypersecretion, keratinization of hair follicles, the course of inflammatory processes, etc.);
- identification and elimination of all factors that cause the occurrence and development of acne, complicate treatment and recovery, contribute to relapses, as well as the elimination of all associated pathologies (gynecological, endocrine, gastrointestinal, infectious, etc.).
How to treat mild acne
Quite often, mild acne can be treated with over-the-counter acne products. This category includes various lotions, gels, creams, which contain substances such as resorcinol, azelaic acid, benzoyl peroxide, sulfur, and salicylic acid.
They produce the following effect:
- benzoyl peroxide - destroys bacteria that provoke the formation of acne;
- azelaic acid - complex anti-inflammatory, antibacterial, keratolytic effect;
- salicylic acid, resorcinol, sulfur - elimination of comedones of any type (today the share of these substances in cosmetology is decreasing).
Such products are supposed to be applied daily to problem areas, immediately after hygienic cleansing of the skin. If irritation or dry skin occurs, the frequency of use of creams and gels is reduced (every 2-3 days).
The face should be cleansed twice a day using soap for problem skin or another gentle product. When using cosmetics, it is advisable to give preference to water-based products that do not clog skin pores.
If possible, it is worth using face masks to eliminate excess sebaceous secretions.
Despite the fact that mild cases can be easily treated on their own, it is recommended to consult a dermatologist on how to treat acne, especially if acne is noticeably progressing (increasing number of pimples, severe scarring, etc.).
How to treat moderate acne
Treatment of moderate acne involves the use of local preparations based on retinoids (gels, creams, etc. applied to the skin) in combination with systemic agents (capsules and tablets to influence pathogenic factors from the inside). If necessary (lack of desired effect), systemic antibiotics are prescribed in a limited volume; Women may be prescribed hormonal contraceptives.
Getting rid of moderate acne requires a relatively long course of medication - antibiotics are taken for a minimum of 6-8 weeks, and a maximum of 4-5 months. In addition, the doctor may prescribe a repeat course (the break between courses is 5-7 days).
If a significant number of pustules are observed, then topical antibacterial drugs are used as an additional measure; In this case, it is important to consider the compatibility of systemic and local medications.
The use of systemic antibiotic drugs may affect the skin's sensitivity to ultraviolet radiation, so it is better to avoid direct sunlight during the treatment period, especially in summer.
In addition, some antibiotics can provoke allergic reactions, thrush, and intestinal disorders.
For women, a combination course may be prescribed, including both systemic antibiotics and oral contraceptives.
If acne removal using all of the above measures was not effective or there was a need for accelerated treatment (the patient has acute psychological problems), then systemic retinoids, which are highly effective, but have certain limitations and side effects, can be used to a limited extent.
Consultation and observation by a dermatologist is mandatory. The doctor will not only help you decide how to treat acne and relieve inflammation, but will also determine whether the risk of recurrence can be completely eliminated.
Minolexin® (Minolexin)
With long-term use of minocycline, the cellular composition of peripheral blood should be regularly monitored, liver function tests should be performed, and the concentration of nitrogen and urea in the serum should be determined.
When using contraceptives with estrogens, additional contraceptives or a combination of contraceptives should be used during minocycline therapy.
A false increase in the level of catecholamines in urine is possible when they are determined by the fluorescent method.
When examining a biopsy of the thyroid gland in patients who have been receiving tetracyclines for a long time, one should take into account the possibility of dark brown staining of the tissue in micropreparations.
While taking the drug and 2-3 weeks after stopping treatment, diarrhea caused by Clostridium difficile (pseudomembranous colitis) may develop. In mild cases, it is sufficient to discontinue treatment and use ion exchange resins (colestyramine, colestipol); in severe cases, replacement of loss of fluid, electrolytes and protein, and the appointment of vancomycin, bacitracin or metronidazole are indicated. Do not use medications that inhibit intestinal motility.
To avoid the development of resistance, minocycline should be used only in accordance with the results of a sensitivity study of pathogenic microorganisms. If susceptibility testing of microorganisms is not possible, the epidemiology and susceptibility profile of microorganisms in a particular region should be taken into account.
In the case of sexually transmitted diseases, if concomitant syphilis is suspected, before starting treatment it is necessary to conduct dark-field microscopy studies. Serological diagnostics of blood serum is recommended to be carried out at least once every four months.
Periodic laboratory diagnostics of body functions, including hematopoietic and renal functions, as well as the condition of the liver, are necessary.
Algorithms for action in the event of certain side effects:
If superinfection develops, minocycline should be discontinued and adequate therapy should be prescribed.
If intracranial pressure increases, minocycline should be discontinued.
Diarrhea is a common disorder associated with antibiotic use. If diarrhea occurs during treatment with minocycline, you should immediately consult a doctor.
Antibiotics of the tetracycline group cause increased sensitivity to direct sunlight and ultraviolet radiation. If erythema occurs, you should stop taking the antibiotic.
How to treat severe acne
The fight against severe acne is based on courses of systemic antibacterial therapy using antibiotics, as well as external therapy with local drugs (retinoids).
In the presence of cystic formations, phlegmons and nodules, therapy can take a long time (the average course duration is from 4 to 9 months).
If such measures are not effective, your doctor may prescribe systemic isotretinoin-based retinoids. Their high effectiveness is due to their effect on the sebaceous glands - the production of sebum is suppressed, and with prolonged use of the drug the glands themselves become smaller. These changes are saved after the course, which allows you to consolidate the results obtained. In addition, isotretinoin demonstrates good antibacterial and anti-inflammatory effects.
This acne treatment shows high effectiveness; Before and after photos allow you to clearly evaluate the result.
Treatment of severe forms involves regular consultations with a doctor, as well as timely completion of all necessary tests.
In the treatment of moderate, moderate and severe forms of acne, antibiotics play the main role. Minocycline for acne stands out against the general background of other drugs of the tetracycline group, demonstrating the greatest effectiveness in the absence of significant disadvantages (increased photosensitivity, poor absorption from food).
Material and methods
The study included 386 male and female patients over 14 years of age who voluntarily wished to participate in the study, with manifestations of mild to moderate acne (papulopustular form), with a disease duration of at least 3 months, and not receiving systemic acne therapy for at least 1 month and external therapy - at least 2 weeks. The absence of pregnancy was confirmed by a test. Breastfeeding women were also not included in the study. There was no history of hypersensitivity to any of the components of the drugs. There was no history of liver or severe renal failure at the time of the study. The survey revealed no data on chronic intoxication. There were no other skin diseases that could interfere with acne assessment. All patients did not simultaneously participate in other clinical studies.
All patients were informed about the type of drug and the nature of the clinical trial, after which written consent to participate in the trial was issued. Informed consent was obtained from each patient before the procedures began.
All patients were divided into two groups.
In experimental subgroup Ia (main, n
=104 people) patients with papulopustular acne with a predominance of papules were included.
Patients received combination therapy: Azelik
2 times a day (morning, afternoon),
Klenzit
1 time a day (evening) locally, in a thin layer on dry skin.
The course of treatment with Klenzit
+
Azelik
was 2 months, followed by monotherapy
with Azelik
for up to 6 months.
In experimental subgroup Ib (main, n
=97) patients with papulopustular acne with a predominance of pustules were included.
Combination therapy was prescribed: Clindovit
2 times a day (morning, evening) spot on pustules,
Azelik
on all other problem areas 2 times a day (morning, evening) locally, in a thin layer on dry skin.
The course of treatment with Clindovit
+
Azelik
was 2 months, followed by monotherapy
with Azelik
for up to 6 months.
In subgroup IIa (control, n
=98) patients with papulopustular acne with a predominance of papules were included.
Klenzit
monotherapy was carried out 2 times a day (morning and evening) locally, in a thin layer on dry skin. The course of treatment is 2 months.
In subgroup IIb (control, n
=87 people) patients with papulopustular acne with a predominance of pustules were included.
Patients were prescribed monotherapy: Clindovit
applied to areas of inflammation 2 times a day (morning, evening) with a thin layer on dry skin. The course of treatment is 2 months.
After 1, 2 and 6 weeks, the effectiveness of treatment, safety and tolerability of the drugs were assessed in all groups.
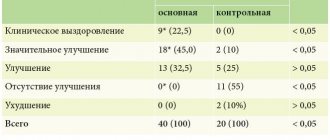
The effectiveness of treatment was assessed clinically according to the following criteria: reduction in sebum secretion, reduction in comedonation, regression of elements, dynamics of post-inflammatory elements. Recovery was considered complete regression of the rash.
At the beginning of treatment and after 1.5 months, all patients underwent a questionnaire survey about the quality of life (dermatological quality of life index - DQL). The index is calculated by summing the scores for each question. The result can vary from 0 to 30 points. The maximum index value is 30 points, and the closer the indicator is to this mark, the more negatively the disease affects the patient’s quality of life.
After completion of therapy, the results of subgroups Ia and IIa, subgroups Ib and IIb were compared.
Statistical processing of the results was carried out using the SPSS 17.0 for Windows application package. The critical level of significance when testing statistical hypotheses in this study was taken equal to 0.05 ( p -
achieved level of significance). The distribution of quantitative data was checked using the Shapiro-Wilk test. The results of the study were summarized using the χ2 criterion.
Advantages of Minolexin in the treatment of moderate to severe forms of acne:
- Minolexin is well absorbed, actively penetrates fat follicles, intensively accumulates in the sebaceous glands, suppressing the growth of pathogenic microorganisms and providing an anti-inflammatory effect
- Minolexin effectively destroys many types of bacteria
- Minolexin is highly effective in lower doses and with shorter duration of treatment
- The result is visually noticeable already in the 6th week of taking Minoleksin
- Minolexin is easy to use and can be taken with meals
- Minolexin is widely and successfully used in Europe and the USA, now the drug is available on the Russian market
- Low resistance of pathogenic organisms to Minolexin - less than 5% (for other antibiotics, bacterial resistance to the drug can reach 62%)
Publications:
- E.S. Snarskaya, M.E. Minakova, E.V. Kuznetsova. Russian Journal of Skin and Venereal Diseases. Minolexin and its place in the standards of treatment of acne vulgaris, No. 3, 2014.
- S.A. Masyukova, I.V. Ilyina, E.G. Sanakoeva, E.V. Gorbakova et al. Minocycline in the treatment of acne and rosacea. Abstracts of the XXXII scientific-practical conference Rakhmanov readings. Dermatology in Russia. 2015; 4 (S1): 82. Pp. 27
- T.A. Belousova, M.V. Goryachkina. Antibiotics in the treatment of acne: the problem of rational choice. EFFECTIVE PHARMACOTHERAPY. Dermatovenereology and dermatocosmetology” No. 1 (4), 2014.
- A.V. Samtsov. Minocycline in systemic acne therapy. Bulletin of dermatology and venereology. 2020; 96(1):67–71.
- E.S. Snarskaya. Antibacterial therapy for acne vulgaris. Bulletin of dermatology and venereology. 2019;95(5):58–67.
- L.S. Kruglova, N.V. Gryazeva. Experience with the use of minocycline in a daily dosage of 50 mg and topical therapy in patients with acne vulgaris. PHARMATEKA, 2022, VOLUME 27 No. 8.
Acne (acne vulgaris) is a multifactorial disease, in the pathogenesis of which genetically determined hyperandrogenism and a genetically determined type of secretion of the sebaceous glands play an important role. Rosacea at the present stage is considered as angioneurosis of the facial skin, which has a polyetiological nature and is characterized by a progressive course, as well as resistance to traditional therapy. Inflammation in acne is primary and precedes follicular hyperkeratosis, and P. acnes takes an active part in the formation of microcomedones. As a result, the innate and adaptive immunity is activated and immune inflammation is formed around the sebaceous gland, the main participants of which are: IL-1α - the “king” of comedonogenesis, IL-6, 8, FNO-α, and P. acnes - the cause of activation of TLRs - receptors and, accordingly, CD4 lymphocytes, interleukins and cytokines of skin cells. The complex mechanism of immune inflammation in rosacea with the participation of pro-inflammatory cytokines (Il-8, Il-6, Il-18) is due to the interaction of trigger factors (stress, UV radiation, etc.) and innate immune factors against the background of abnormal amounts of cathelicidin and kallikrein 5 in the skin patients, which leads to the activation of vascular endothelial growth factor (VEGF), corticotropin-releasing factor (CHR) and the universal nuclear transcription factor kappa-bi (Nk-kB). The “target” of external and internal trigger factors are Langerhans cells, endothelial cells and immunocompetent cells. The release of neuropeptides leads to the formation of neurogenic inflammation, which in turn leads to disruption of neoangiogenesis, dysregulation of neurovascular connections in the skin, changes in the architecture of the intercellular matrix. Immune and neurogenic inflammation is accompanied by pathomorphological changes in the skin: telangiectasia, elastosis, perivascular and perifollicular infiltrates, represented mainly by lymphocytes, neutrophils, epithelioid cells. The first-line drugs for the treatment of acne are retinoids (topical and systemic), the second are antibiotics, which are used for moderate and moderate forms, including acne inversa, to which adolescents respond better at the onset of the disease and women with late acne. also in milder forms during hormonal therapy. For subtype II rosacea, first-line drugs are also tetracycline antibiotics. The answer to the question why tetracyclines are basic antibiotics in the treatment of acne and rosacea lies in the effect on the pathophysiological mechanisms of the development of these dermatoses. It is noted that the effect of systemic doxycycline in acne and subtype II rosacea is that it affects the ATP-regulated release of proinflammatory cytokines (IL-8, IL-1a), blocking the effects of IL-8, reduces neutrophil chemotaxis, changes the metabolism of arachidonic acid, inhibits the pro-inflammatory activity of phospholipase A2, suppresses the activity of nitric oxide (NO), suppresses the synthesis of reactive oxygen species by neutrophils (ROS), inhibits the activity of matrix metalloproteinases, including collagenases (MMP-8,-13), gelatinases (MMP-2,-9), elastase (MMP-12p). We conducted a clinical study of an antibiotic from the tetracycline group, minocycline (Minolexin®), for acne and rosacea, which, according to its mechanism of action, has a bacteriostatic effect, disrupting protein synthesis in the microbial cell. The drug has the ability to accumulate in the sebaceous glands, is highly lipophilic and penetrates the lipid layer of bacteria. In terms of therapeutic activity, it is comparable to doxycycline, but exceeds it in the rate of onset of the anti-inflammatory effect. In 2006, the FDA approved new expanded recommendations for the use of minocycline in the treatment of acne, and in 2012 it was included in the European recommendations (Belousova T.A. et al., 2013). Purpose of the study: to study the clinical effectiveness of minocycline in the treatment of moderate and moderate forms of acne and papulopustular (subtype II) rosacea. Under observation were 98 patients, 67 women and 31 men aged from 12 to 52 years with a disease duration of one to 12 years. For moderate severity of acne and papulopustular form of rosacea, the drug was prescribed in a daily dose of 50 mg 2 times a day and/or 100 mg once for 4 weeks and then 50 mg 1 time per day for up to 8-12 weeks. . For moderate forms, minocycline was prescribed in a daily dose of 100 mg 2 times a day for 4 weeks, then 100 mg 1 time a day for 16 weeks. The effectiveness of treatment was assessed using the Dermatological Acne Index (DAI), Dermatological Symptom Score (DIS) and dermatoscopy. Conclusion: the clinical effectiveness of minocycline in the treatment of moderate and moderate forms of acne, as well as rosacea, was 92.6%, 91.5%, 92.4%, respectively. There were no side effects or refusals of treatment during the observation of patients, which allows us to conclude that the use of minocycline as the drug of choice in the treatment of moderate and moderate forms of acne and subtype II rosacea is advisable.