Loose, deformed, inelastic skin in the thighs, buttocks and abdomen worries women no less than overweight and obesity. According to many authors, this problem occurs in 80-90% of women in different countries [11, 24]. There is a certain pattern in the prevalence of cellulite. Statistics show that women of Asian and African descent are less likely to develop cellulite than white women. In women from Mediterranean and Latin American countries, cellulite often develops in the buttocks and thighs, while in women from Anglo-Saxon and Nordic countries, it occurs on the abdomen. This may be due to national nutritional traditions and the range of most commonly consumed foods. Many authors point out that the problem of cellulite is most acute in those countries where they eat large amounts of saturated fat [12, 23]. In Japan, where the incidence of cellulite is minimal, the population consumes exclusively polyunsaturated fats and low-calorie foods. It has been noted that with lifestyle changes and the transition to a higher-calorie diet, the prevalence of cellulite among women of the Negroid and Mongoloid races increases. In addition to the nature of nutrition, physical inactivity is essential for the formation of cellulite, which in many developed countries is a problem that requires an immediate solution. Thus, the avalanche-like increase in the incidence of cellulite is due not only to subjective factors, such as growing attention to body aesthetics, but also to objective factors, in particular, changes in the nature of nutrition in most countries of the world and the growing prevalence of physical inactivity [5, 11, 23].
Pathogenetic mechanisms
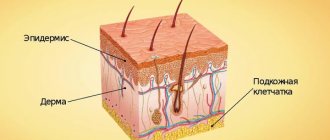
There is no doubt that, from the point of view of pathogenesis, cellulite is characterized by a triad of signs: hypertrophy of subcutaneous fatty tissue, microcirculation disorders and compaction of connective tissue. The changes that occur at the cellular and functional levels form a vicious circle leading to the progression of disorders.
Changes in adipose tissue
Sometimes it is quite difficult to figure out what comes first in the formation of cellulite: activation of lipogenesis or dyscirculatory disorders, these processes are so interconnected. A number of authors highlight the degeneration of fat cells, which leads to connective tissue fibrosis [2, 14]. They believe that the primary cause of this pathology is adipocyte hypertrophy, which changes intracellular processes and disrupts the structure of membranes. The cells swell more and more, the connective tissue septa become denser, more and more intercellular substance is synthesized - as a result, the evacuation of fat from the fat vacuole becomes increasingly difficult.
Adipose tissue, as one of the body systems involved in the pathogenesis of cellulite, is certainly important. The main component of adipose tissue in humans is adipocytes, highly specialized cells designed to create energy reserves and consisting mainly of triglycerides, which are the most efficient form of energy storage. Substances produced by adipocytes have a variety of biological effects and can influence the activity of metabolic processes in tissues and various systems of the body either directly or indirectly through the neuroendocrine system, interacting with pituitary hormones, catecholamines, and insulin. Adipose tissue produces many biologically active substances: leptin, tumor necrosis factor α, interleukin-6, free fatty acids, acetylation-stimulating protein (ASP), plasminogen anti-activator 1 (PAI-1), insulin-like growth factor 1 (IGF-1), angiotensinogen, estrogens, prostaglandins. An increase in the number or volume of adipocytes occurs due to a chronic disorder of their metabolism, that is, an imbalance between lipolysis and lipogenesis. Membrane receptors of adipocytes (α2-, β2- and β3-adrenergic receptors), G-proteins, hormone-sensitive lipase, and leptin are involved in the regulation of lipolysis. Activation of α-adrenergic receptors stimulates lipogenesis, and α-adrenergic receptors stimulate lipolysis. Regulation of lipolysis is carried out through the adenylate cyclase mechanism: when receptors are activated, AMP is converted to cAMP, which, in turn, activates hormone-sensitive lipase, which breaks down triglycerides. Phosphodiesterase then converts cAMP back to AMP, blocking further lipolysis. Norepinephrine, having a high affinity for α-adrenergic receptors, blocks lipolysis. After all α-adrenergic receptors are bound, epinephrine binds to α-adrenergic receptors, which leads to the activation of adenylate cyclase and stimulates lipolysis. The activity of adenylate cyclase is also increased by glucagon, ACTH, growth hormone, thyroid hormones, and vasopressin. Salicylates and nicotinic acid suppress lipolysis. Estrogens increase the activity of lipogenesis enzymes, which causes hypertrophy of adipocytes, which, together with fibrosclerosis, leads to the formation of micro- and macronodules in cellulite [17-19, 21, 22].
Studies have shown that the fat vacuole of the adipocyte on top of a single-layer phospholipid membrane is covered with special proteins. It turned out that these proteins are not only actively involved in processes associated with the mobilization of stored fat, but also influence the differentiation of progenitor cells, and perilipin, a protein surrounding the fat vacuole of a mature adipocyte, plays a very important role in this. Fat vacuoles in preadipocytes are surrounded by another special protein - ADRP (adipocyte differentiation-related protein). When the adipocyte matures, ADRP leaves the vacuole membrane and is replaced by perilipin. It is perilipin that prevents the degradation of triglycerides. If fat vacuoles continue to form, they are immediately coated with perilipin. When energy is needed, hormone-sensitive lipase hydrolyzes stored triglycerides, but for this they must be available to it. It is believed that perilipin is “negotiated” through phosphorylation, which changes the structure of the membrane so that triglycerides become available to hormone-sensitive lipase [20, 21, 24].
The rate of fat accumulation in adipocytes depends on the intensity of blood circulation in problem areas. When blood flow accelerates, or rather when microcirculation improves, lipolysis increases, and when it worsens, lipogenesis. With stagnation in adipose tissue, local hypertrophy of adipocytes can develop even against the background of normal body weight. If the adipocyte loses connection with the microvasculature, fat becomes trapped in the cells [25].
At the same time, the data available today regarding the pathogenesis of cellulite suggest that the accumulation of fat in adipocytes, or, more precisely, their hypertrophy, is not the leading pathogenetic factor. This is confirmed by the fact that signs of cellulite are often observed in women with normal and even low body weight. Thus, when we examined women aged 19 to 49 years who complained of cellulite, 54% had normal weight [10]. The presence of cellulite in women who are not obese or overweight indicates that adipocyte hypertrophy is an important, but not the main mechanism for the formation of this pathology. In addition, it is known that when correcting cellulite associated with obesity, weight loss by reducing the amount of adipose tissue is accompanied by a visual worsening of cellulite. Only long enough and persistent treatment can change this picture.
Why are men practically immune to cellulite?
In the male half, “orange peel” is very rare. This is explained by the fact that men and women have different structures of adipose tissue and hormonal balance in the body.
In girls, collagen fibers are located parallel to each other. As a result, they are more likely to stretch the tissues and cause fluid stagnation. There is also more estrogen in the female body than in the male body. This sex hormone has a great effect on the deposition of fat cells.
Factors that help you understand why men don't have cellulite:
- Collagen fibers intersect and have a cellular structure. This structure allows the tissues to avoid stretching.
- The body contains small amounts of estrogen.
Sometimes the fibers can stretch, but it is still not as noticeable as in women. Therefore, even if there is cellulite, no one notices it.
Microcirculation disorders
The condition of the microvasculature is directly related to the condition of large vessels. Almost all authors [3, 5, 7, 11, 13] emphasize: a decrease in muscle activity and a sedentary lifestyle worsen venous outflow, slow down lymph circulation, which leads to a decrease in metabolism, increased lipogenesis, and, as a consequence, the development of cellulite. Prolonged sedentary work and driving, typical of many actively working women, interfere with normal blood flow in the lower extremities, causing venous stagnation and capillary damage. According to our data, diseases of the veins and lymphatic vessels are present in 56% of patients with cellulite.
Violation of venous outflow and stagnation of lymph lead to increased permeability of the vascular wall and the release of plasma into the interstitial space. The resulting swelling of the interstitial tissue and hypoxia aggravate microcirculation disorders, and substances released when the endothelium is damaged promote the proliferation of fibroblasts and the compaction of connective tissue septa, which no longer delimit, but compress the lobules of adipose tissue [2]. The hydrostatic pressure in the capillaries depends on the amount of blood and lymph, which in different organs ranges from 18 to 40 mm Hg. Art. As a rule, it slightly exceeds the oncotic pressure of the blood (19-21 mm Hg), due to which the pressure gradient in the capillary walls is directed towards the tissue, and fluid filtration prevails over its reabsorption into the plasma. Excess fluid entering the tissue is removed through the lymphatic system. The pressure gradient in the interstitium causes fluid to move within it, facilitating the delivery of necessary substances to the cells. Hemodynamic parameters in capillaries are closely related to the permeability of their walls, which depends on the pressure gradient and protein concentration in the interstitial space and plasma. In turn, the physicochemical parameters of the interstitial environment of the lymphatic capillaries create the conditions for lymph formation and movement of lymph.
Lymphatic capillaries, the walls of which are formed by endothelium, remove excess fluid, proteins and metabolic products from tissues. The mechanisms of lymph movement in capillaries are not yet clear enough, but it has been proven that contractions of large lymphatic vessels (lymphangions) with a developed muscular layer play a significant role. Stagnation of fluid in the lumen of the vessel stretches its wall, disrupts the forward movement of lymph, and the absence of vascular contractions further aggravates this pathogenetic mechanism.
Thus, the condition of large drainage vessels, namely veins and lymphangions, directly affects microcirculation. Microcirculation disorders are observed in most women over 30 years of age (especially those who have given birth, taking hormonal contraceptives, wearing high-heeled shoes), so it is possible that the pathology of venous circulation is the leading link in the development of local lipodystrophy.
The main parameters characterizing the functioning of the microcirculation system are determined by the state of hemodynamics in the capillaries, the permeability of their walls, and the forces that ensure the movement of interstitial fluid and lymph. Microcirculation disorders are usually divided into vascular, intravascular and extravascular. Changes in blood flow, capillary pressure, and the functional state of the vascular wall are important for tissue perfusion. All microcirculation disorders have one thing in common: ultimately, transcapillary exchange suffers. Changes in the rheological properties of blood play a significant role in the mechanism of tissue damage and thrombus formation. The fluidity in the microcirculatory system is also affected by the aggregation state of platelets. It plays a leading role in thrombus formation and the development of intravascular aggregation of cellular elements.
Changes in the vascular wall are caused by changes in the location and shape of endothelial cells. Extravascular changes leading to impaired microcirculation are primarily associated with pathological processes in perivascular tissue. When the permeability of capillary walls decreases, the transfer of biologically active substances through the basement membrane is primarily disrupted. Changes in biochemical processes, water-salt metabolism and the nature of redox reactions lead to the development of circulatory hypoxia and deterioration in the nutrition of organs and tissues. When capillary permeability is impaired, plastic metabolism and energy supply to cells are significantly affected [3, 4]. A decrease in the efficiency of microcirculation is manifested by hypoxemia, venous hyperoxia, a decrease in tissue oxygen utilization, and the accumulation of lactic and pyruvic acids. Microcirculatory disturbances lead to decreased oxygen consumption and aerobic performance. All of the above ultimately leads to disturbances in the lipolysis-lipogenesis system. Changes in the arteriolar precapillary sphincters in the area of cellulite are described, causing an increase in pressure in the capillaries. An increase in capillary and interstitial pressure (due to excessive polymerization of glycosaminoglycans), as well as a decrease in plasma current (due to compression and compression of blood vessels) can lead to an increase in the permeability of capillaries and venules, and consequently to ectasia, swelling of the dermis and the formation of compacted partitions between individual adipocytes and between lobules of adipose tissue. A decrease in venous tone may occur in parallel with an increase in capillary fragility as a result of changes in the perivascular connective tissue, which leads to microvascular rupture and microbleeding [13, 14, 16, 21].
The fluidity of blood in the vessels depends on the composition of the plasma, the nature of the blood flow in the microvessels (turbulent or laminar), the plasticity and deformability of erythrocytes, and the tendency of cells to aggregation. It is known that hyperlipidemia affects the condition of vessel walls, blood clotting, microcirculation and organ perfusion [9]. The fluidity of blood in microvessels is largely determined by the protein-lipid composition of plasma. With a high concentration of lipoproteins in plasma, blood flow in small-diameter vessels becomes intermittent and turbulent. With hyperlipidemia, the cholesterol content in erythrocyte membranes increases, their size increases, they become less plastic, their ability to change their shape when passing through capillaries worsens, blood viscosity increases, and erythrocyte aggregation increases [1]. The study of microcirculation in people with hyperlipidemia revealed both functional disorders of capillary blood flow (slowing of blood flow, its “granularity”, formation of microaggregates, blood stagnation, microthrombosis) and morphological changes in the capillaries themselves (twisting, uneven diameter, microaneurysms, desolation with switching off blood flow ).
Hyperlipidemia is accompanied by a decrease in the arteriovenous oxygen difference and indicates a deterioration in oxygen utilization in peripheral tissues. With hyperlipidemia, the ability of the endothelium to produce the endothelial vascular relaxation factor, nitric oxide, is impaired. In addition, the hypoxia experienced by endothelial cells under conditions of hyperlipidemia leads to increased production of endothelin, a strong vasoconstrictor and nitric oxide antagonist, which ultimately leads to impaired microcirculation [9].
Cellulite is characterized by hemorheological disorders. Disturbances in the cellular link are expressed in increased aggregation of platelets and erythrocytes, and a decrease in the deformability of erythrocytes. An increase in platelet aggregation ability leads to hypercoagulation, enhances parietal microthrombosis and disrupts microcirculation. This, in turn, prevents the normal utilization of oxygen by tissues and leads to metabolic disorders with a predominance of anaerobic processes of glycolysis; on the other hand, the release of tissue thromboplastin is stimulated, which increases fibrinogen levels and enhances coagulation.
A compensatory reaction that prevents further thrombus formation is an increase in fibrinolysis. In patients with cellulite, an increase in blood viscosity at different shear rates and an increase in hematocrit were noted. Analysis of coagulogram data shows the presence of hypercoagulation syndrome, since the plasma recalcification time significantly decreases, the level of fibrinogen increases, the fibrinolytic activity of plasma and plasma tolerance to heparin decrease [1, 10]. Microcirculation studies using laser Doppler flowmetry make it possible to assess the functional activity of microvessels. There are two types of disorders: atonic and spastic types of microcirculation.
Apparently, at the initial stages of cellulite development, there is a decrease in arteriolar tone, a significant increase in intravascular resistance, slight venous stagnation and stagnation in the capillary microcirculation develop; passive mechanisms of microcirculation regulation predominate over active ones. Blood filling of the capillaries at the initial stages, on the one hand, ensures adequate trophism of tissues, and on the other hand, overflow of the capillary bed triggers pathogenetic mechanisms for the development of cellulite (expansion of capillaries, extravasation of plasma into surrounding tissues, development of edema, fluid retention in tissues, compression of surrounding tissues) . As cellulite progresses, a spastic type of microcirculation is formed, characterized by an increase in arteriolar tone, an increase in intravascular resistance, more pronounced venous stagnation, the predominance of active mechanisms of blood flow regulation, a significant decrease in basal blood flow, and insufficient blood supply in the capillary unit. Lack of blood supply in the capillary link can lead to hypoxia, activation of fibroblasts and the development of fibrosclerosis, which is typical for the third and fourth stages of cellulite. More pronounced phenomena of venous stagnation than in patients with the atonic type indicate significant disturbances and decompensation of the venular microcirculation.
Oxidative stress
A number of authors have studied changes in the parameters of oxidative processes and antioxidant protection and their effect on microcirculation. The content of lipid peroxidation products in the blood was determined: diene conjugates, malondialdehyde, as well as elastase activity, levels of α1-antitrypsin, α2-macroglobulin. The result revealed an increase in free radical oxidation processes in patients with cellulite. There was an increased content of diene conjugates, increased elastase activity with a reduced level of its inhibitor (α1-antitrypsin) and an increased level of α2-macroglobulin, coming from the interstitium into the blood with an increase in vascular permeability. All this indicates a high intensity of lipid peroxidation processes in the blood in patients with cellulite [10].
The level of oxidative stress in cellulite was assessed by the content in tissues of the product of lipid peroxidation - malondialdehyde, as well as products of protein peroxidation - carbonyl groups. The levels of total, oxidized and reduced glutathione, ceruloplasmin, superoxide dismutase, and total antioxidants were selected as indicators of the state of the antioxidant system. A decrease in the levels of some antioxidants was found while the levels of others increased, thereby maintaining the overall activity of free radical oxidation processes, which is vital for structural homeostasis. Thus, the data obtained indicate disturbances in the lipid peroxidation system and the development of oxidative stress in women with cellulite [6].
Changes in connective tissue
The third factor involved in the pathogenesis of cellulite is connective tissue. It is believed that fibroblast activation caused by estrogens causes excessive polymerization of glycosaminoglycans in the dermis and perivascular connective tissue, which increases their hydrophilicity and interstitial osmotic pressure. An increase in the level of estrogen and thyroid hormones (T3, T4) promotes the accumulation of hyaluronic acid in tissues, which binds water molecules, and therefore increases swelling. Water retention (edema) and an increase in the viscosity of the intercellular fluid lead to cell deformation and compression of blood vessels, provoking tissue hypoxia. Hypoxia causes a change in aerobic glucose metabolism, resulting in increased lactic acid production. This activates proline hydroxylase, an enzyme that facilitates the conversion of proline to hydroxyproline in procollagen with a subsequent increase in collagen synthesis. The accumulation of collagen fibers in tissues is accompanied by a decrease in the amount of elastin and interstitial substance, changes in the ratio of proteoglycans and glycoproteins, which leads to a decrease in the permeability of connective tissue, inhibition of repair, decrease in turgor and elasticity of the skin. Qualitative and quantitative changes in collagen provoke fibrosclerosis in the interlobar connective tissue septa. Thus, micronodules are formed, which are visible on the surface of the skin and can be detected by touch.
Hormonal imbalance
Hormonal imbalance contributes to the aggravation of microcirculatory disorders: decreased levels of progesterone, increased levels of androgens and aldosterone. Aldosterone enhances sodium reabsorption in the renal tubules, while vasopressin production is stimulated, water resorption occurs, and the volume of circulating plasma increases. The question of the direct participation of sex hormones in the pathogenesis of cellulite remains controversial. Most authors point to the influence of estrogens and progesterone produced by the ovaries. Extragonadal synthesis of estrogen is of great importance. At a certain period of life, its role is decisive, while most estrogens are synthesized in adipose tissue. The activity of adipose tissue aromatase depends on the topographic location of the fat. In the subcutaneous adipose tissue of the femoral-gluteal region, aromatase activity is 4 times higher than in the subcutaneous adipose tissue of the abdomen. The skin is very sensitive to the effects of female sex hormones due to the specific receptors it contains. Estrogens suppress the secretory activity of the sebaceous glands, increase the level of hyaluronic acid in the dermis, which increases the amount of intercellular fluid and converts soluble collagen into insoluble. A decrease in progesterone levels with a simultaneous increase in androgen levels contributes to fluid retention and a decrease in the rate of synaptic transmission, in particular through β-adrenergic receptors. At the same time, data on the influence of female sex hormones on the process of cellulite formation are in the nature of theoretical assumptions and have not yet received sufficient scientific confirmation [11, 16-18].
Conclusion
Based on the described mechanisms of cellulite formation, any measures aimed at its correction should take into account both the nature of microcirculation disorders, the severity of fat deposits and changes in connective tissue, and the stage of the process. Mesotherapy has in its arsenal a wide range of tools that allow it to influence the pathogenetic mechanisms of cellulite formation, and, of course, is an effective method of its correction.
Literature
- Bolotova L. G., Turova E. A., Kosheleva I. V. Complex use of physical factors (oxygen-ozone therapy and electrical myostimulation) in the correction of edematous fibrosclerotic panniculopathy. // Questions of balneology, physiotherapy and therapeutic physical culture, 2007, No. 1. P. 24-26.
- Blashmaison F. Methods for assessing cellulite: water retention index and Celluscore.// Aesthetic Medicine, 2005, No. 5. P. 89-94.
- Erofeev N. P., Orlov R. S. The lymphatic system is a necessary element of fluid homeostasis in the human body: a new look at old problems. // Bulletin of St. Petersburg University, 2008, ser. 11, No. 4 P. 78-86.
- Kapilevich L. V., Kovalev I. V., Baskakov M. B., Medvedev M. A. Intracellular signaling systems in epithelium- and endothelium-dependent processes of smooth muscle relaxation. // Advances in physiological sciences, 2001, No. 2. P. 88-98
- Korolkova T. N. Pathogenetic aspects of gynoid lipodystrophy. // Experimental and clinical dermatocosmetology, 2005, No. 4. P. 49-60.
- Korolkova T. N., Poliychuk T. P. Study of indicators of oxidative stress during oxygen-ozone therapy of local fat deposits. // Clinical dermatology and venereology, 2009, No. 2. P. 37-42.
- Koshevoy E. G. Dynamics of skin microcirculation in patients with gynoid lipodystrophy under the influence of vibration vacuum therapy. // Materials of the II International Congress “Restorative Medicine and Rehabilitation”, September 20-21, 2005, M., 2005. P. 48.
- Krupatkin A.I., Sidorov V.V. Laser Doppler flowmetry of blood microcirculation. Guide for doctors. - M.: Medicine, 2005.
- Lipovetsky B. M. Clinical lipidology. - St. Petersburg: Nauka, 2000.
- Minina A. P., Turova E. A., Bolatova L. G. et al. The use of laser Doppler flowmetry to assess microcirculation in patients with edematous fibrosclerosing panniculopathy. // Angiology and vascular surgery, 2004, No. 3. P. 46-49.
- Mikheeva S.V. Prevalence and risk factors for the formation of cellulite. // Public health and healthcare. Collection of scientific papers. St. Petersburg, 2000. pp. 11-12.
- Mikheeva S.V. Localization of cellulite in women. // Current problems of sanitary and epidemiological well-being of the population of the Northwestern region. Materials of scientific and practical conference. St. Petersburg, 2000. P. 173.
- Polenov S. A. Fundamentals of microcirculation. // Regional blood circulation and microcirculation, 2008, No. 1. P.5-19.
- Ranneva E. A., Zubkova S. A., Movchan V. N. Modern instrumental methods for diagnosing cellulite. // Experimental and clinical dermatocosmetology, 2007, No. 4. P. 48-51.
- Stanishevskaya T.I. The main types of blood microcirculation and the frequency of their occurrence in girls in the south-eastern region of Ukraine. // Scientific notes of the Tauride National University named after. V. I. Vernadsky. Series "Biology, Chemistry", 2005, No. 1. P. 131-141.
- Turova E. A., Bolatova L. G., Minina A. P. On the etiology and pathogenesis of cellulite. // Bulletin of Aesthetic Medicine, 2008, No. 4. P. 23-31.
- Chubrieva S. Yu., Glukhov N. V., Zaichik A. Yu. Adipose tissue as an endocrine regulator (literature review). // Bulletin of St. Petersburg University, 2008, ser. 11, no. 1. pp. 32-42.
- Avram MM Cellulite: a review of its physiology and treatment. // J Cosmet Laser Ther, 2004, 6. 181-185.
- Bastard JP, Maachi M, Lagathu C et al. Recent advances in the relationship between obesity, inflation and insulin resistance. // Eur Cytokine Netw, 2006, 17. 4-12.
- Hexsel DM, Abreu M, Rodrigues TC et al. Side-by-side comparison of areas with and without cellulite depressions using magnetic resonance imaging. // Dermatol Surg, 2009, 35. 1471-1477.
- Khan MH, Victor F, Rao B, Sadick NS Treatment of cellulite: Part I. Pathophysiology. // J Am Acad Dermatol, 2010, 62. 361-370.
- Lupi O., Semenovitch IJ, Treu C. et al. Evaluation of the effect ects of caffeine in the microcirculation and edema on thighs and buttocks using the orthogonal polarization spectral imaging and clinical parameters. // J Cosmet Dermatol, 2007, 6.102-107.
- Milani GB, Natal Filho A., Amado Joao SM Correlation between lumbar lordosis angle and degree of gynoid lipodystrophy (cellulite) in asymptomatic women. // Clinics (Sao Paulo), 2008, 63. 503-508.
- Quatresooz P., Xhauflaire-Uhoda E., Pierard-Franchimont C., Pierard GE Cellulite histopathology and related mechanobiology. // Int J Cosmet Sci, 2006, 28. 207-210.
- Smalls LK, Hicks M, Passeretti D et al. Effect of weight loss on cellulite: gynoid lypodystrophy. // Plast Reconstr Surg, 2006, 118. 510-516.
Methods for preventing and eliminating cellulite
Since this problem arises due to a whole range of different reasons, the methods for solving it should be multidirectional and include:
- diet;
- physical exercise;
- cosmetic procedures.
You need to start by making an appointment with a body cosmetologist, who will conduct an examination, collect anamnesis, and prescribe a course of treatment, taking into account the stage of cellulite and the characteristics of your health condition.
The main methods for getting rid of “orange peel” are:
- Massage (manual and hardware);
- Wraps;
- Fitness;
- Proper nutrition.
Let's pay more detailed attention to each point.
Massage for cellulite
Let's start with a massage. This is an effective way to eliminate fat deposits, restore skin firmness and elasticity, and shape your figure.
There are many massage techniques. Within the framework of our topic, first of all, it is worth mentioning anti-cellulite manual massage. It is usually intended to smooth and tone the skin on the legs. The technique for performing this massage is as follows: the massage therapist’s hand movements should be fast and include 50% rubbing and 50% squeezing. The impact is superficial. A course of at least 10 sessions is recommended.
Hardware methods for treating cellulite
Hardware methods - LPG and Endosphere - have also proven themselves well.
LPG is a vacuum-roller effect on body tissue. The technique was developed in France in the 80s of the 20th century. With the help of self-propelled rollers located in the handpiece, the skin fold is mechanically kneaded, which is captured by the vacuum. The whole body is massaged: the specialist moves the handpiece horizontally and vertically, and the rollers rotate in one direction or the other. The most problematic areas of the body (hips, butt and others) are treated with special attention.
Result of LPG massage:
- Removing excess fluid;
- Stimulation of lipolysis;
- Activation of blood circulation and lymph flow;
- Production of collagen in tissues.
All this leads to the fact that the skin is evened out, excess volumes and kilograms are lost, the silhouette becomes more toned. This type of massage requires a special elastic suit that protects the surface of the skin, making the procedure comfortable, and ensures hygiene. The standard course is 10 sessions, the duration of 1 session is 35 minutes in accordance with the protocol of the device manufacturer.
Endosphere therapy was developed by Italian scientists in the early 2000s. This is a method of compression microvibration transmitted to the body using a special device - a cylinder equipped with rotating spheres made of special silicone. The vibration of the spheres causes the deep layer of tissue to “work”, stimulating the work of mechanoreceptors (Merkel particles), thereby activating the process of lipolysis (fat breakdown) and the breakdown of fibrous compounds.
When carrying out the procedure, the cosmetologist changes the speed of movement of the handpiece and thereby sets the parameters of vibration of the spheres and their rotation, providing pressure on the body (“pump effect”). In this case, the specialist varies the intensity of the impact depending on the individual tasks of the patient.
Endosphere therapy is done directly on the skin, onto which massage oil is applied for better gliding of the spheres. Even if cellulite is only on the thighs, the procedure involves not only one or another leg, but also the body as a whole - otherwise the procedure will be ineffective.
This is a course technique, on average 6 to 12 sessions are required, each of which lasts 1 hour 15 minutes in accordance with the recommendations of the creators of the technology.
Endosphere Effect:
- Lymphatic drainage effect;
- Smoothing the skin surface (eliminating cellulite);
- Elimination of local fat deposits;
- Figure correction;
- Weight reduction.
By removing excess water, puffiness is relieved, the skin becomes dense and elastic, more toned.
These devices are recognized leaders in the field of body care.
Many people are interested in:
- Which one is better?
- How is LPG different from Endosphere?
In answering these questions, we must first say that these are two fundamentally different techniques of influence, as can be seen from their description. Secondly, which of these devices will be effective can only be decided by a cosmetologist after examining the patient, taking into account the medical history and the stage of cellulite. Third, a combination of these two methods may be required to achieve the desired effect.
As mentioned above, getting rid of cellulite requires an integrated approach. Therefore, it will be useful to combine massage with wraps, which have a beneficial effect on the quality of the skin. They can be of various types: based on oligo-elements (algae, for example), mud, cream. The temperature regime used is also different - there are hot wraps and cold ones.
At home, such procedures can be carried out only after consultation with a specialist: if cosmetics are used incorrectly, the timing of the procedure and other requirements are not followed, the disease can be aggravated.
How does cellulite wrap work?
A special composition is applied to the skin, then the body is wrapped in a thermal blanket, the desired temperature is set and after the allotted time the procedure ends. The temperature chosen by the cosmetologist should activate the effect of cosmetic products, due to which lymphatic drainage occurs, the functioning of blood vessels is normalized, the skin is nourished and becomes smoother.