Where is Chlorhexidine used?
The pharmaceutical product is used for the treatment and prevention of diseases caused by microorganisms sensitive to Chlorhexidine.
Depending on the concentration of the substance, the medicine can be used in the treatment of various pathologies.
After operations, in order to prevent infectious pathologies, doctors resort to using a pharmaceutical solution.
Chlorhexidine is often used for dental purposes for the treatment of dentures. In some cases, medication is used to treat periodontitis, stomatitis, and they are used to rinse the gums.
The medicine is used in:
- Urology
- Gynecology
- Surgery
Chlorhexidine and coronavirus
It has been proven that alcohol-based antiseptics are effective against coronavirus, and its content should be at least 60%, but preferably more. Therefore, chlorhexidine in an aqueous solution effectively copes with bacteria, but not with viruses.
But, as we said above, chlorhexidine is also made with alcohol, which makes this antiseptic effective in the fight against COVID 19. To do this, you can purchase an alcohol solution of chlorhexidine with a concentration of 0.5% at the pharmacy. Another option: take a 20% aqueous solution of the substance and a 70% alcohol-containing liquid and mix these two components in a ratio of 1 to 40. You need to treat your hands with the composition according to this principle:
- First, wash your hands with soap for 15 seconds.
- Then rub in the alcohol solution of chlorhexidine for 2 minutes.
- The amount of liquid rubbed in should be approximately 5 ml.
But you can wipe surfaces with aqueous solutions; with prolonged contact with the pathogen, most of the virus will still be destroyed.
Often, antiseptics with chlorhexidine are produced in the form of a gel containing alcohol and depanthenol, which moisturizes the skin.
Contraindications
Chlorhexidine is contraindicated:
- In case of hypersensitivity to the components of the drug
- People suffering from dermatitis
- Do not use together with other antiseptics, for example, with hydrogen peroxide
- For ophthalmic use, rinsing the eyes with this product is prohibited.
- For disinfection of the surgical field
- After intervention on the auditory canal and central nervous system
It is important to know that the pharmaceutical product should be used with caution when treating children.
Possible side effects
As with any other drug, the use of chlorhexidine is fraught with side effects. People sensitive to the drug may experience allergic reactions.
Sometimes the effect of a solution or gel is manifested by photosensitivity - sensitivity of the skin and mucous membranes to ultraviolet radiation.
Rinsing with a solution is fraught with a change in the color of tooth enamel, the deposition of tartar, and the taste may also be affected.
sells antiseptics with chlorhexidine. We supply certified goods of our own production in bulk, guarantee quality and competitive prices, and organize delivery.
Brief instructions for use
To prevent sexually transmitted diseases, after unprotected sexual intercourse, after a maximum of 2 hours, 2-3 ml of a 0.5% solution should be administered into the urinary canal of a man, 1 ml into the canal for women and 5-10 ml into the vagina. You can treat skin areas near the genitals with the product. After administering the drug, try to postpone urination for 2 hours.
Your doctor should tell you about douching for gynecological diseases.
For sore throat, rinse the mouth with 0.5% or 0.2% Chlorohexidine solution.
For inflammatory pathologies of the urinary tract, it is necessary to inject 2-3 ml of 0.05% of the product into the urinary canal.
Before using the drug, you should consult your doctor.
Application in cosmetology
The scope of application of chlorhexidine for cosmetic purposes is quite extensive. Most often it is used in the treatment of acne and various pustular lesions. But you should figure out whether everyone can use chlorhexidine to wipe their face.
You should wipe your face with chlorhexidine no more than 2 times a day.
The positive effect of chlorhexidine on the skin is obtained due to:
- its deep penetration into the affected area and the destruction of microbes and bacteria present there, which are the source of inflammation;
- ability to stop the inflammatory process;
- ability to remove dead cells from the surface of the epidermis;
- cleansing and disinfecting wounds in case of an abscess breakthrough.
Based on the available reviews on the use of the drug, we can conclude that if used correctly, everyone can achieve an excellent antiseptic effect. From its influence, bacteria and harmful microorganisms lose their ability to multiply and fester.
You might be interested in learning about Rejuvenating the skin around the eyes with Aevita + reviews
Where to put candles
Depending on the type of disease, the method of administering Chlorhexidine suppositories can be different: rectal or vaginal.
But it is important to understand that the use of suppositories is only permissible as prescribed by a doctor.
Before using the suppository, you need to wash and dry your hands well, then you need to remove it from the package and insert it into the vagina in a lying position.
To avoid leakage of the drug, do not rush to get out of bed.
Chlorhexidine suppositories help well with thrush and cystitis.
When is chlorhexidine needed? Indications
- After tooth extraction . The doctor may prescribe oral baths with chlorhexidine if the tooth was removed due to severe inflammation and not planned. During normal extractions, there is no need to make baths or rinse, so as not to damage the blood clot in the socket of the extracted tooth.
- For stomatitis . This is an inflammation of the mucous membranes of the cheeks and lips, which manifests itself in small wounds. Inflammation can be caused by various reasons: hormonal, taking medications, allergic reactions and household ones, for example, when eating crackers or seeds.
- For inflammation of the gums . In this case, you can use an antiseptic at home for pain and discomfort, but you should definitely see a doctor. Most often, the gums become inflamed due to supra- and subgingival plaque that needs to be removed. The procedure is called periodontal oral hygiene and after it the doctor will no longer prescribe chlorhexidine.
This is due to the peculiarity of the product to create a film on the surface of the teeth, to which new plaque and coloring pigments will “stick”. Therefore, after a course of chlorhexidine, a dark plaque forms on the teeth. Residues of food “stick” to this roughness, which are already difficult to remove on your own, they begin to provoke inflammation and the problem appears all over again. Thus, all the benefits of treatment are negated.
Why is Chlorhexidine better than peroxide?
- Hydrogen peroxide and Chlorhexidine are antiseptics. Medicines differ in their spectrum of effects and medicinal properties.
- Hydrogen peroxide, unlike Chlorhexidine, is available in only one dosage form, which is not very convenient.
Chlorkesidine suppositories are used for the treatment of gynecological and urological pathologies.
Both products disinfect wounds and abrasions well.
Chlorhexidine has a wider range of therapeutic effects; it is used to treat the hands of the surgeon and nurse before surgery, and it is also used in gynecology.
Infections caused by antibiotic-resistant microflora represent an ever-growing threat in both hospital and community settings. Nosocomial infections lead to a decrease in the effectiveness of therapy, an increase in the duration of hospitalization and an increase in mortality.
Chlorhexidine bigluconate was developed in Great Britain in 1950. It is the first internationally recognized antiseptic for skin and wounds. One of the advantages of chlorhexidine, in addition to its pronounced antimicrobial effect, is its ability to bind to various biological substrates while maintaining its antibacterial activity, and then be slowly released, which leads to the preservation of effective concentrations of the drug. To date, there are no reports of resistance to chlorhexidine, despite more than 60 years of active use of the drug in the clinic. Chlorhexidine gluconate remains important in the prevention of nosocomial infections.
Widespread use of antiseptic methods for the prevention and treatment of infections followed the publication of Joseph Lister's The Antiseptic Principle in Surgical Practice in 1867. At the same time, “Lister’s antiseptics” met ardent opponents, whose main argument was the toxicity of the antiseptic they used (carbolic acid). Despite the availability of numerous antiseptics, the question of the safety and effectiveness of this group of drugs remains constantly relevant. The “longevity” of chlorhexidine and the prospects for its further use as one of the most powerful antiseptics widely used in clinical practice is a pressing issue for clinicians.
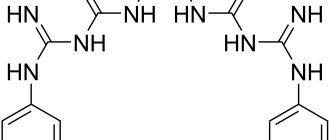
A cationic detergent (detergent), later named chlorhexidine, was synthesized during the development of antimalarial drugs in 1947. This compound has bactericidal antimicrobial activity, especially against gram-positive microorganisms. Of the 10,040 compounds, the first to enter the market was chlorhexidine gluconate, registered in 1954 by Imperial Chemical Industries Co.LTD (UK) as “Gibitan” - the first internationally recognized antiseptic for the treatment of wound surfaces and skin. In 1957, only 3 years after entering the market, the indications for its use were expanded to include not only skin treatment, but also use in ophthalmology, urology, gynecology and otorhinolaryngology. In 1959, chlorhexidine began to be used to control bacterial plaque, leading to its widespread use in dentistry. Currently, in clinical practice, chlorhexidine is preferred not only when treating the skin (hands, surgical field), but also as an oral antiseptic, including for the prevention of nosocomial infection. The most commonly used concentrations are 0.2% and 0.12% solutions. In addition to its effect on plaque and gum condition (gingivitis), chlorhexidine is effective in the prevention and treatment of caries, secondary infections after dental procedures or implant placement. Chlorhexidine reduces the bacterial load and the risk of bacteremia after dental procedures. It is also used in the treatment of recurrent atrophic stomatitis and stomatitis associated with the installation of dentures, primarily in groups of patients with orthodontic appliances and immune disorders. One of the main advantages of chlorhexidine, in addition to its powerful antimicrobial effect, is its ability to retain its antimicrobial activity when bound to various substrates. At the same time, it is released slowly while maintaining an effective concentration. This property is known as substantiveness. Chlorhexidine is not susceptible to blood, pus, or saliva. Chlorhexidine is pharmaceutically incompatible with soap and detergents (for example, those containing lauryl sulfate), alkalis and other anionic compounds (colloids, gum arabic, carboxymethylcellulose), and iodine. Compatible with ethyl alcohol, benzalkonium chloride (contained in contraceptives for local use Pharmatex and Benatex). Ethanol enhances the effectiveness of the drug. The bactericidal effect increases with increasing temperature. At temperatures above 100°C, the drug partially decomposes. Used in a neutral environment; at pH 5-8 the difference in activity is small; at pH above 8 it precipitates. The use of hard water reduces bactericidal properties. Compatible with drugs containing a cationic group (benzalkonium chloride, cetrimonium bromide).
The unique combination of properties of chlorhexidine also determines the variety of dosage forms.
Chlorhexidine is available in the following forms: • 20% concentrated solution – intended for dilution before use, used in medical institutions; • 0.05% solution in plastic and glass bottles of 70 and 100 ml - used without dilution, including at home; • Vaginal suppositories (suppositories) “Heksikon” containing 0.016 g of chlorhexidine, 1 or 10 suppositories in a package; • Vaginal suppositories (suppositories) “Heksikon D” containing 0.008 g of chlorhexidine – intended for children, 10 suppositories per package; • Gel containing 0.5% chlorhexidine. Chlorhexidine is included in the following preparations: • Solutions for mouth rinsing for dental diseases and manipulations (tooth extraction, opening of abscesses, professional cleaning, etc.) – Elgidium, Amident, Eludril; • Gels for gums, intended for the treatment of dental diseases and pain relief in the oral cavity (for example, when getting used to dentures), one of the components of which is chlorhexidine - Dicloran Denta, Elugel, Metrohex, Parodium, Elgifluor, Dentamet, Metrogyl Denta; • Elgidium toothpaste; • Solutions with other antiseptics – Baktoderm (with benzalkonium chloride), Chlorhexidine alcohol spray – for the treatment of skin infections, Citeal (with hexamidine and chlorocresol) – for topical use in gynecology, dermatology; • Ointments Bepanten plus and Depantol (with panthenol - wound healing effect), Bemilon (with betamethasone - anti-inflammatory effect); • Vaginal suppositories Depantol (with panthenol) – used in gynecology after surgical interventions; • Chlorhexidine in combination with lidocaine for local anesthetic action in the Lidocaine-Asept spray and Instillagel and Kategel gels with lidocaine; • Lozenges for sore throat, stomatitis and other diseases of the oropharynx and oral cavity – Hexoral tabs, Anti-Angin formula, Sebidin.
Can alcohol be used as an antiseptic?
In its pure form, we do not recommend using alcohol as an antiseptic. In sanitizers, the amount of ethyl ranges from 60 to 80%; they are no longer used. The alcohol strength is 96%, meaning this concentration will almost certainly cause skin problems, especially with repeated use. In addition, even the simplest sanitizer contains auxiliary substances - glycerin, hydrogen peroxide and others. They not only perform antiviral functions, but also serve as softeners, humidifiers, etc. Thus, using alcohol carries the risk of burns, irritation, and other problems.
By the way, you cannot use vodka either, it is ineffective, since its strength is only 40%, which will not kill viruses.
Indications for use
Chlorhexidine digluconate is used in medical practice to disinfect the surface of the skin of patients before surgery, the surface of wounds, sterilization of surgical instruments and treatment of the skin of the hands of medical personnel. For these purposes, a 1% chlorhexidine solution is used.
A 2% solution is used to treat sexually transmitted diseases, infections of the genitourinary system, and for disinfection in gynecology.
Chlorhexidine for the oral cavity: at a concentration of 0.3% it prevents the appearance of plaque and stomatitis. Rinsing and irrigation help against candidiasis and gingivitis. Chlorhexidine for the face (reviews from consumers and dermatologists are similar) can be used to treat acne, although manufacturers do not indicate this method of use in the instructions.
Skin interaction
Chlorhexidine is a cationic surfactant with a broad spectrum of antibacterial activity; it also acts against fungi, but to a lesser extent. It destroys the membranes of microbial cells and coagulates their cytoplasmic proteins. At pH 5-8, chlorhexidine salts dissociate, resulting in the formation of a positively charged chlorhexidine cation.
This cation binds to the negatively charged bacterial cell wall. Chlorhexidine inhibits cell membrane enzymes and disrupts the interaction of lipids and proteins in membranes, the bacterial cell membrane becomes permeable and the cell contents leak out.
At higher concentrations of chlorhexidine (more than 0.01%), cytoplasmic proteins coagulate, denature, and the bacterial cell dies. Mold cells are destroyed by the same mechanism. At high concentrations, chlorhexidine destroys the virus envelope.
The effect of chlorhexidine lasts for several hours. It is non-toxic in low concentrations and does not irritate the skin.
Chlorhexidine applied to the facial skin for 8-12 weeks significantly reduces the amount of acne. An ointment containing chlorhexidine gluconate as an active substance reduces the formation of comedones. Acne occurs due to dysfunction of the sebaceous glands and excessive secretion of oily skin secretions.
If the disease is accompanied by hyperkeratosis, in which epidermal cells do not exfoliate regularly enough, then comedones are formed. Skin secretions are a breeding ground for bacteria, including Propionibacterium acnes. Bacteria multiply in closed pores and cause inflammation.
Antibacterial agents, which include chlorhexidine, act against bacterial flora, so inflammation is reduced. But these remedies do not treat the causes of acne, which explains the negative reviews about its use.
Some dermatologists also recommend using chlorhexidine to treat the skin of the face and body to treat acne. Other experts believe that chlorhexidine is toxic and should only be used when the benefits outweigh its harmful effects. Chlorhexidine against acne on the back and shoulders: the product is quite effective, since the skin in these areas is less sensitive.
Chlorhexidine is used to eliminate inflammation on the face.
Chlorhexidine for the face (consumer reviews of its use as an anti-acne product, both negative and positive) is more suitable for skin with intense secretion, that is, for oily skin or combination skin. On skin with insufficient sebum production and sensitive skin, chlorhexidine often causes peeling and irritation.
In what cases can you wipe your face with chlorhexidine?
In cases where acne and pimples appear on the face, especially during adolescence, a teenager may wonder whether it is possible to wipe the face with chlorhexidine. If this problem occurs, not everyone will receive a dermatologist’s recommendation for the use of chlorhexidine as a cosmetic product.
The skin of the face becomes contaminated when decay products of most types of bacteria and microorganisms that cause the process of decay enter the pores. By squeezing pimples, infected particles can be brought inside, and then they can spread through the blood throughout the body and cause complications.
You can use chlorhexidine solution for disinfection for teenage acne
If the causes of the rash are other, for example, demodicosis (damage to the epidermis by skin mites) or infection, then chlorhexidine will not be a panacea. This requires other treatment prescribed by a doctor.
Note! The drug can be used only after finding out the cause of the problem and receiving a recommendation from a dermatologist . Then it will be precisely established that there are no contraindications for the use of the drug, and it will be established whether it is possible for a particular person to wipe the face with chlorhexidine.